Abbreviations: LAM = lymphangioleiomyomatosis; TSC = tuberous sclerosis
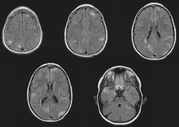
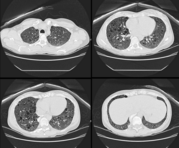
Lymphangioleiomyomatosis (LAM) and multifocal micronodular pneumocyte hyperplasia produce cystic and nodular disease, respectively, in the lungs of patients with tuberous sclerosis (TSC). The objective of this study was to prospectively characterize the prevalence, clinical presentation, and genetic basis of lung disease in TSC. CT scanning of the chest on 23 asymptomatic women with TSC identified cystic or nodular changes in 52%. Cystic pulmonary parenchymal changes consistent with LAM were found in nine patients (39%). These patients tended to be older than cyst-negative patients (31.9 [+ or -] 7.6 years vs 24.8 [+ or -] 11.6 years, p = 0.09), and there was no correlation between presence of cysts and tobacco use, age at menarche, history of pregnancy, or use of estrogen-containing medications. Three of the cyst-positive patients had a prior history of pneumothorax. Pulmonary function studies revealed evidence of gas trapping but normal spirometric indexes in the cyst-positive group. All 9 cyst-positive patients had angiomyolipomas, which were larger (p < 0.05) and more frequently required intervention (p = 0.08) than cyst-negative patients (8 of 14 patients with angiomyolipomas, p < 0.05). Ten patients (43%) had pulmonary parenchymal nodules. Pulmonary nodules were more common in women with cysts (78% vs 21%, p < 0.05). TSC2 mutations were identified in all cyst-positive patients who were tested (n = 8), while both TSC1 and TSC2 mutations were identified in patients with nodular disease. Correlation of the mutational and radiographic data revealed one pair of sisters who were discordant for cystic disease, two mother-daughter pairs who were discordant for nodular disease, and no clear association between cyst development and a specific mutational type. This prospective analysis demonstrates that cystic and nodular pulmonary changes consistent with LAM and multifocal modular pneumocyte hyperplasia are common in women with TSC.
* From the Departments of Pediatrics (Dr. Sethuraman), Neurology (Dr. Franz, Ms. Leonard, Ms. Chuck), Radiology (Drs. Brody and Meyer), and Medicine (Dr. McCormack), Division of Pulmonary and Critical Care Medicine, University of Cincinnati, Cincinnati, OH; the Department of Pathology (Dr. Colby), Mayo Clinic, Scottsdale, AZ; and the Department of Medicine, Division of Hematology (Drs. Dabora and Kwiatkowski), Brigham and Women's Hospital, Boston, MA.
Correspondence to: Frank McCormack, MD, Division of Pulmonary and Critical Care Medicine, MSB Room 6001, 231 Albert Sabin Way, Cincinnati, OH 45267-0564; e-mail:frank.mccormack@uc.edu
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group