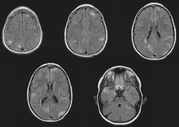
Introduction: Tuberous sclerosis complex (TSC) is a rare, autosomal dominant disorder. We report a patient with multiple signs of TSC, referred for evaluation of a chest radiograph showing small lung nodules.
Case Report: A 45 year-old woman was referred because of an abnormal chest radiograph. The patient reported previous good health, with no known lung diseases. She had no respiratory symptoms. One year ago, during a routine medical evaluation, the patient was noted to have an elevated serum creatinine. An abdominal CT scan revealed bilateral renal masses. Needle biopsy of one of the masses showed a "hamartomatous smooth muscle lesion similar to the elements of an angiomyolipoma." A chest radiograph showed diffuse, subcentimeter pulmonary nodules. Bronchoscopy with transbronchial biopsy was "nondiagnostic." The patient was referred for urologic evaluation and, subsequently, pulmonary consultation.
There was no history of cough, sputum production or dyspnea. The patient was able to walk several miles without shortness of breath. A seizure disorder was diagnosed four years previously and treated with diphenylhydantoin. In addition, there was a history of hypothyroidism, treated with levothyroxine. A vaginal hysterectomy was performed 10 years previously for dysfunctional uterine bleeding. The patient never smoked; there was no history of alcohol or illicit drug use. She was employed as a lien searcher and had no occupational exposures to dusts or fumes. She had not traveled outside the United States and had no pets. There was no family history of pulmonary disease. The patient's son had his first seizure at age 21 years.
On physical examination the patient was a well-appearing, thin woman. Raised red nodules were noted on the nose. The chest was symmetric and the lung fields were clear to auscultation. The heart was regular, with normal first and second heart sounds. Abdominal examination was normal. The extremities were without clubbing, cyanosis or edema. Neurologic examination was normal.
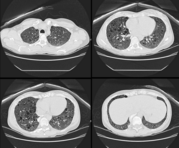
A chest radiograph demonstrated multiple small nodules throughout the upper and lower lung fields bilaterally. A chest CT scan showed multiple, well circumscribed nodules measuring 3 to 5 mm in diameter. No other significant abnormalities were noted. Pulmonary function studies were normal.
Video-assisted thoracoscopic lung biopsy revealed multiple, well-demarcated nodules composed of slightly thickened alveolar septa lined by hyperplastic type II pneumocytes; mild cytologic atypia was noted. HMB-45 stains were negative, and tuberin immunoreactivity in the nodules was positive. The findings are consistent with a diagnosis of multifocal micronodular pneumocyte hyperplasia (MNPH).
Discussion: Tuberous sclerosis (TSC) is a rare disorder characterized by mental retardation, seizures, and hamartomatous proliferations involving the skin, kidneys, and brain. Familial and sporadic cases have been described. Pulmonary involvement, which occurs in fewer than 3% of patients, is usually clinically indistinguishable from lymphangioleiomyomatosis (LAM). MNPH is a newly-recognized, rare pulmonary manifestation of TSC. MNPH may occur in concert with LAM or, as in this case, occur alone. The clinical significance of MNPH is uncertain. However, the prognosis does not appear to be as severe as in LAM based on case series. MNPH may represent a forme frust of TSC or, alternatively, be part of the spectrum of LAM.
Conclusion: MNPH is a newly-recognized pulmonary manifestation of TSC, which appears to have less impact than LAM on patients' clinical course.
J. D. Christie, MD and M. A. Grippi, MD--University of Pennsylvania Health System, Philadelphia, PA
COPYRIGHT 1999 American College of Chest Physicians
COPYRIGHT 2000 Gale Group