[TABLES HAVE BEEN OMITTED]
Although tuberous sclerosis is an inherited disorder with an autosomal dominant pattern of transmission, 50 percent of cases are sporadic. The disease is characterized by mental retardation, seizures and adenoma sebaceum; however, mental deficiency is not always present. Approximately 30 percent of patients have normal intelligence. Seizures are always present in patients with mental retardation and in most patients with normal intelligence.1
Cutaneous markers, a characteristic feature of the disease, include adenoma sebaceum (a slightly elevated rash that is most commonly seen in the nasolabial folds and on the cheeks); the shagreen patch (a roughened area of skin usually seen in the midline of the lower back), and hypopigmented spots in the midline of the lower back or anywhere on the trunk and limbs. The hypopigmented areas on the trunk and limbs may not be visible to the unaided eye, but can be seen under ultraviolet light.
Pathophysiology
Tuberous sclerosis derives its name from cortical tubers on the gyral surface of the brain, one of the many forms of hamartomas in this disease. Subependymal nodules, common along the inner margins of the cerebral ventricles, are another form of central nervous system hamartoma. Tuberal calcification commonly occurs, which often allows the disease to be diagnosed on plain radiographs of the skull.2 Malignant degeneration of the tubers occasionally occurs, usually in the form of giant cell astrocytoma.
Hamartomas are benign tumors consisting of an overgrowth of one or more tissues normally found in the area of tumor development. In tuberous sclerosis, hamartomas may develop in the central nervous system, ovaries, adrenal glands, liver and thyroid gland.3 In addition, cardiac rhabdomyomas and sclerotic lesions of bone may be seen. Renal lesions, often multiple and bilateral, are seen in approximately 75 percent of patients.
Patients with renal lesions commonly develop angiomyolipomas (tumors composed of variable amounts of fat, muscle and blood vessels). Because the vascular components of angiomyolipomas lack the normal elastic components, aneurysm formation is relatively common. The sudden onset of flank pain or anemia may herald the onset of renal hemorrhage secondary to intrarenal aneurysmal rupture. Isolated angiomyolipomas may be seen in otherwise normal patients, most commonly in middle-aged women.
Pulmonary abnormalities are also seen in tuberous sclerosis and are marked by progression of smooth muscle in pulmonary septae, bronchi and lymphatics. These abnormalities also occur in lymphangiomyomatosis, a condition in young females that is manifested by recurrent pleural effusions and pneumothoraces.
Radiologic Manifestations
Calcified intracranial hamartomas can be visualized on plain radiographs of the skull Figure 1). However, such radiographic findings are nonspecific, since intracranial calcification may also be seen in a number of infectious processes, including intrauterine toxoplasmosis, intrauterine cytomegalovirus infection and adult toxoplasmosis. In addition, hyperparathyroidism may produce calcification in the basal ganglia. Furthermore, areas of increased density within the skull vault are seen in approximately half of patients with tuberous sclerosis,2 and may be difficult to distinguish on plain radiographs from intracerebral calcification.
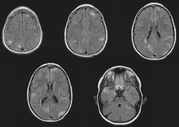
Computed tomography (CT) demonstrates the predominantly periventricular location of the calcified hamartomas Figures 2 and 3). The subependymal and subcortical hamartomas may undergo malignant degeneration to giant cell astrocytomas. This change may be manifested by contrast enhancement of one of these lesions. Giant cell astrocytomas occurring at the foramen of Monro can result in hydrocephalus due to ventricular outlet obstruction.1
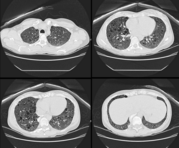
Plain radiographs of the chest often demonstrate a progressive reticulonodular abnormality. This abnormality cannot be distinguished radiographically from idiopathic pulmonary fibrosis. In pulmonary fibrosis, however, lung volumes are diminished; they are normal or increased in tuberous sclerosis. Recurrent pleural effusions may be seen in tuberous sclerosis and lymphangiomyomatosis.
Renal abnormalities are best evaluated by ultrasound examination or, preferably, CT scanning. Ultrasound may demonstrate a variety of findings, including a renal mass with intrarenal foci of increased echogenicity (bright regions). These areas represent fat or hemorrhage within an angiomyolipoma. However, when the lipomatous component is not pronounced, the renal mass may be difficult to distinguish from other renal neoplasms. CT examination often allows a specific diagnosis Figure 4). The kidney usually appears enlarged and heterogeneous, with low attenuation (dark regions) representing fat interspersed within the kidney. Regions of acute hemorrhage are demonstrated as focal areas of high attenuation (bright areas).
In the appropriate clinical setting, the diagnosis may be made with confidence by CT examination. Angiographic features of renal involvement are multiple intrarenal aneurysms and tortuous vessels. However, these findings are often absent if the angiomatous component of the tumor is not pronounced. In the absence of a known diagnosis of tuberous sclerosis or when the characteristic features are lacking, pathologic examination following nephrectomy is necessary.
REFERENCES
1. Gean A. The phakomatoses. In: Taveras JM, Ferrucci JT, eds. Radiology: diagnosis, imaging, intervention. Vol. 3. Philadelphia: Lippincott, 1988.
2. Medley BE, McLeod RA, Houser OW. Tuberous sclerosis. Semin Roentgenol 1976;11:35-54.
3. Bender BL, Yunis EJ. The pathology of tuberous sclerosis. Pathol Ann 1982;17(Pt 1):33982.
4. Pare JA, Fraser RG. Synopsis of diseases of the chest. Philadelphia: Saunders, 1983:660-2.
COPYRIGHT 1991 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group