INTRODUCTION: Wheezing is a common symptom among infants and toddlers most frequently due to asthma, viral infection/ bronchiolitis, or foreign body aspiration. We present a case of a 17 month old girl with wheezing refractory to bronchodilator treatments, without a history suspicious for foreign body aspiration or recurrent wheezing.
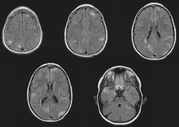
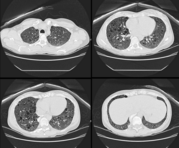
CASE PRESENTATION: The patient is a 17 month old female who presented with a one day history of congestion, cough and tactile fever. She rapidly progressed to respiratory failure and was intubated prior to transport. During the patient's transport and after her arrival at our institution, she was difficult to ventilate, unless she was deeply sedated. When sedated she had normal airway compliance. The transport nurse noted a large "apple-sized" pulsatile midline mass in her abdomen suspicious for an abdominal aortic aneurysm and she was hypertensive. Initial chest x-ray demonstrated significant deviation of the upper thoracic esophagus, prominence of the aortic shadow and dysplastic ribs. Computed tomography with contrast of the thorax, abdomen, and pelvis revealed dilatation of the descending thoracic aorta, with a saccular protrusion off the medial aspect of the proximal descending aorta which compressed the distal thoracic trachea. (Figure 1) The trachea at that level measured 2.5mm in the anterior to posterior diameter. There were two other saccular aneurysms of the thoracic aorta. Below the level of the superior mesenteric artery there was again marked aortic dilatation that extended to the aortic bifurcation and included the proximal-most portion of the right common iliac artery. The fight renal artery came off the aneurysm and was also saccular in nature. The right kidney was small with irregular contour containing multiple cysts. (Figure 2) Five days after her initial presentation the thoracic aorta was repaired due to tracheal compression. Ten days after her admission she underwent repair of the large abdominal aneurysm and right nephrectomy due to her hypertension and the aneurysm size. Magnetic resonance imaging of her brain demonstrated multiple cortical tubers, as well as nodules thought to be early giant cell tumors and multiple subependymal nodules. The diagnosis of tuberous sclerosis complex (TSC) was made based on these findings.
[FIGURES 1-2 OMITTED]
DISCUSSIONS: TSC was described in the 1880's by a French physician name Bourneville. TSC, also known as Bourneville's disease, is an autosomal dominant condition with variable penetrance that occurs de novo in approximately 60% of cases. (1) TSC typically involves abnormalities of the skin, brain, kidney and heart with widespread development of hamartomas. The diagnosis of TSC is based on clinical findings and the criteria for diagnosis were revised in July 1998. (2) The patient must have two major features or one major feature plus two minor features for a definitive diagnosis of TSC. Two causative genes, TSC1 and TSC2, have been identified. Molecular testing is available for confirmatory diagnostic testing, prenatal diagnosis, and for genetic counseling. Most children with TSC have brain involvement and seizures and developmental disabilities are common. Aneurysms are an uncommon presentation for TSC in children, Jost et. al. reported a review of the literature with the addition of two new cases n = 15. Most of the patients had either a thoracic aortic aneurysm or abdominal aortic aneurysm, and only one patient had both. The series reported an acute mortality rate of 40%. (3).
CONCLUSION: Tuberous sclerosis complex affects approximately one in 8,000 adults and one in 6,000 newborns(ref). Although rare, aortic aneurysms do occur.
REFERENCES:
(1) Tuberous Sclerosis Complex http://biology.kenyon.edu/slonc/bio38/ howell/tsc.htm Access date: April 29 2005
(2) Gene Reviews http://www.genetests.org/servlet/access?db=geneclinics& site=gt&id=8888891&key=143YUK-Kv- 2.VeL&gry=&fen=y&fw=JOs&filename=/profiles/tuberous-sclerosis/index.html Access date: April 28 2005
(3) Jost CJ, Gloviczki P, Edwards WD, et al. Aortic aneurysms in children and young adults with tuberous sclerosis: report of two cases and review of the literature. J Vasc Surg. 2001; 33:639-642
DISCLOSURE: Melissa Gowans, None.
Melissa J. Gowans MD * Heather T. Keenan MD Susan L. Bratton MD Constance Maves MD John Hawkins MD University of Utah, Salt Lake City, UT
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group