Study objectives: To investigate the clinicopathologic features of primary tracheobronchial adenoid cystic carcinoma (ACC), and to examine kit protein (CD117) expression, and a possible correlation between the histologic grade and Ki-67 positivity.
Design: Retrospective 10-year study (from 1992 to 2001).
Setting: Referral center for interventional pulmonology.
Patients: Fourteen patients referred to our institution for laser resection of tracheal or endobronchial tumors.
Interventions: Twelve patients were treated primarily by laser resection via bronchoscopy with subsequent radiation therapy. The remaining two patients had tracheal resection with postoperative radiation and radiation therapy alone.
Results: Fourteen patients (5 men and 9 women) had an average age of 44 years at diagnosis (age range, 29 to 57 years). Five of 14 patients were smokers (average smoking history, 28.5 pack-years), 8 were nonsmokers, and the smoking history was unknown in 1 patient. Major symptoms at presentation included cough (57.1%), dyspnea (71.4%), and hoarseness (14.3%). Two patients (14.3%) presented with respiratory failure. Eleven patients (78.6%) had one or more recurrences, and 4 patients (28.6%) had metastases, primarily to the lungs. The average time to either recurrence or metastasis was 4.6 years after the initial diagnosis. Five patients (35.7%), all of whom had recurrences and/or metastasis during the course of their disease, died of their disease (average time, 8.2 years). Thirteen of 13 cases stained for CD117 were positive in the tumor cell cytoplasm with membranous accentuation. Our cases included g grade I tumors, 4 grade II tumors, and 2 grade III tumors, which did not correlate with the degree of Ki-67 positivity.
Conclusions: Tracheobronchial ACCs in our study were more common in women and nonsmokers who presented with nonspecific respiratory symptoms and followed a clinical course generally comparable to that of tumors in the salivary glands. CD117 expression was present in all cases tested, and Ki-67 stain results did not correlate with the tumor grade.
Key words: adenoid cystic carcinoma; c-kit; CD117; Ki-67; tracheobronchial
Abbreviations: ACC = adenoid cystic carcinoma; CD117 = kit protein
**********
Adenoid cystic carcinoma (ACC), known as cylindroma in the past, is a variant of adenocarcinoma with distinct histopathologic and clinical features. ACC occurs most commonly in the salivary glands and, less commonly, at other sites such as the breast, skin, uterine cervix, upper aerodigestive tract, and lung. (1-7) ACC of the salivary gland is an indolent low grade carcinoma with a tendency for local recurrence and late metastases typically over a long period. (8) Due to this natural history, the overall long-term prognosis of salivary ACCs is unfavorable. (8)
Because ACCs outside of major and minor salivary glands are rare, clinicopathologic characteristics have generally been extrapolated from those of salivary gland ACCs. However, breast ACCs have been reported (9-13) to follow a favorable clinical course with a better prognosis than that in salivary ACCs. Furthermore, breast ACCs also demonstrate a distinct biological feature from those of conventional breast carcinomas with a comparable histologic grade (ie, well-differentiated), in that breast ACCs are consistently negative for estrogen and progesterone receptors, (9-13) as opposed to the positive estrogen and progesterone receptor status in most well-differentiated, low-grade mammary carcinomas. Whether tracheobronchial ACCs manifest the clinical/biological differences seen in breast ACCs has not been well-documented in the literature.
Kit protein (CD117), encoded by c-kit proto-oncogene, is a type III tyrosine kinase receptor. (14-17) CD117 is structurally related to other transmembrane tyrosine kinase receptors, including platelet-derived growth factor, vascular permeability factor/vascular endothelial cell growth factor, and colony-stimulating factor-1. (14-17) CD117 plays an important physiologic role in the development of hematopoietic cells, melanocytes, and germ cells. (18) CD117 expression has been reported in many tumors including mastocytosis, GI stromal tumors, and germ cell tumors. (19) CD117 positivity has been used as a marker for a potential tyrosine kinase inhibitor therapy, which has been highly effective in a subset of advanced GI stromal tumor cases. (20) Previous studies (21-23) have reported CD117 expression in salivary gland ACCs, but CD117 expression in tracheobronchial ACCs has not been reported in the literature. Ki-67 is a marker for cell proliferation and has been used as an adjunct to histologic grade or as a prognostic indicator in some tumors. (24) We present our experience at the University of California San Diego Medical Center with 14 cases of primary ACC in the tracheobronchial location with emphasis on the clinico-pathologic features, CD117 expression, and correlation between the histologic grade and reactivity to a proliferation cell marker Ki-67 stain.
MATERIALS AND METHODS
Case Selection and Histopathologic Review
All cases with a diagnosis of ACC in the tracheobronchial tree were retrospectively identified from the surreal pathology file during the period from 1992 to 2001 at the University of California San Diego Medical Center. All patients in the present study were treated at our Pulmonary Special Procedures Unit, which specializes in treating obstructive airway diseases with Nd-YAG laser photoresection via rigid bronchoscopy. Two pathologists (EA and ESY) examined all the hcmatoxylin-cosinstained glass slides to verify the diagnosis and independently graded each case according to the previously published criteria, (25) as follows: grade I, tubular and cribriform pattern only with no solid areas; grade II, < 30% solid areas; and grade III, [greater than or equal to] 30% solid areas, often with accompanying necrosis, cellular atypia, and mitoses. Pertinent clinical information was obtained by a review of medical records and contact with the primary physicians when necessary.
Immunohistochemistry
Immunohistochemical stains were performed with an autostainer (DAKO; Carpinteria, CA) on 5-[micro]m-thick sections of formalin-fixed, paraffin-embedded tissues using a detection system (Envision; DAKO) with antibodies to CD117 (ie, polyclonal rabbit antibody, 1:200 dilution; DAKO) and Ki-67 (monoclonal antibody-1, monoclonal mouse antibody, 1:50 dilution; DAKO). CD117 immunostaining was interpreted as positive if [greater than or equal to] 5% of the tumor cells stained positively in the cytoplasm with membranous accentuation. In each case, CD117 staining was scored according to the following criteria: 0, < 5%; 1, 5 to < 25%; 2, 25 to < 50%; 3, [greater than or equal to] 50%, as in a previous study. (22) Ki-67 positivity (nuclear staining) was scored with the following criteria: 0, < 1%: 1, 1 to < 5%; 2, 5 to < 19%: 3, 10 to < 59%; 3, [greater than or equal to] 50%.
Statistical Analysis
The Spearman rank correlation coefficient was used for the analysis of the relationships among histologic grade, CD117 score, and Ki-67 score, A p value of < 0.05 was considered to be statistically significant.
RESULTS
Clinical Features
The clinical characteristics of each patient are summarized in Table 1. Five patients (35.7%) were men and 9 (64.3%) were women, with a presenting age at diagnosis ranging from 29 to 53 years (average age, 44 years). Five patients (35.7%) were smokers (average smoking history, 28.5 pack-years), 8 patients (57.1%) were nonsmokers, and the smoking history was unknown in 1 case. Major symptoms at the time of presentation included cough in 8 patients (57.1%), dyspnea in 10 patients (71.4%), and hoarseness in 2 patients (14.3%). One patient (7.1%) presented with hemoptysis, and two patients (14.3%) presented with respiratory failure secondary to near complete obstruction of the trachea. Seven patients (50.0%) had wheezing or stridor as the major physical finding, often leading to an empirical treatment of asthma before the discovery of the obstructing masses. Pulmonary function tests were not available for our review, as most patients were referred to our institution for definitive management of their airway disease after diagnosis by bronchoscopy or radiographic imaging.
Bronchoscopic Findings
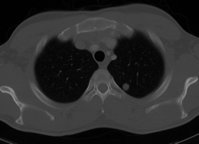
Marked obstruction of the tracheal lumen, ranging from 60 to 98%, was seen in 7 of 14 patients (50.0%). Three of the patients (21.4%) had obstruction of either the right or left main bronchus. Overall, the trachea was involved in 12 patients (85.7%), 4 of whom also showed coexisting bronchial lesions. Two patients (14.3%) had a right or left bronchial involvement without tracheal disease. On bronchoscopy, the ACCs typically presented as multiple, white-yellow lobulated masses with increased vascularity, covered with bronchial mucosa (Fig 1).
[FIGURE 1 OMITTED]
Treatment
Twelve patients (85.7%) were treated with Nd-YAG laser photoresection via rigid bronchoscopy; and 4 of these patients subsequently required placement of Silastic stents to maintain airway potency. Three patients (21.4%) underwent tracheal resection with end-to-end anastomosis. All 14 patients were treated with external beam radiation. Two patients who did not have laser resection were treated with tracheal resection plus radiation or with radiation alone (Table 1).
Follow-up
Recurrence of primary disease occurred in 11 of the 14 patients (78.6%) and occurred from 1 month to 6 years after the initial diagnosis. Four patients (28.6%) had metastasis to the lungs, and one of these patients also had liver metastases. The average time to recurrence or metastasis was 4.6 years after the initial diagnosis. Multiple recurrences were documented in five patients (35.7%). Recurrence occurred primarily at the original tumor site, in either the trachea or bronchi, in 50.0% of patients. Five patients (35.7%) died of disease an average of 5.6 years after the initial diagnosis (median, 8 years). All five of these patients experienced either recurrences or metastases. Of the remaining nine patients, one was alive without evidence of disease and seven were alive with disease at the time of their last clinical follow-up. One patient received a diagnosis, was treated, and was discharged from our facility within a 2-week time span, but subsequently was lost to follow-up. Pertinent clinical details are summarized in Table 1.
Histopathology and Immunohistochemistry
The tumors were located in the submucosa with no evidence of connection or transition to surface bronchial lining epithelium. Some tumors showed areas associated with the tracheobronchial seromucous glands. All cases showed characteristic features of ACC with variable combinations of cribriform, tubular, and solid patterns. Eight cases were grade I (57.1%), four cases were grade II (28.6%) and two cases were grade III (14.3%) [Fig 2]. Perineural invasion was identified in three patients (21.4%), which consisted of 1 grade I case and 2 grade II cases. There was no significant correlation between histologic grade and Ki-67 score (r = 0.27; p = 0.37), as demonstrated by a high Ki-67 score in a tumor with low histologic grade (Fig 3). Cytoplasmic CD117 immunoreactivity with membranous accentuation was seen in all 13 patients (1 patient's paraffin block was not available for staining) [Fig 4]. The cases with a cribriform pattern revealed the CD117 staining in the luminal cell population (Fig 4) as described in a previous study (22) of salivary gland ACCs. There was no significant correlation between histologic grade and CD117 score (r = 0.01; p = 0.99), or between CD117 score and Ki-67 score (r=0.35; p = 0.24). The histologic grade, CD117 score, and Ki-67 score in each case are summarized in Table 2.
[FIGURES 2-4 OMITTED]
DISCUSSION
We report the clinicopathologic features of 14 ACC cases occurring in the tracheobronchial tree. In the past 20 years, the use of lasers for treating endobronchial disease has been tested and accepted as an important therapeutic modality for obstructive endobronchial or tracheal lesions. (26) Although the primary role of laser resection in oncology patients is a palliative one, this technique may allow a prolonged survival when combined with other therapies. (27) Most of our patients underwent subsequent surgical excision and/or radiation therapy after laser resection. Due to the small sample size, we could not appreciate any significant correlation between survival and treatment type on statistical analysis using both Kaplan-Meier curves and the Cox proportional hazards model (data not shown).
The largest series of bronchial ACCs was published in 1978 by Coulan et al, (4) with 20 cases at Mayo Clinic over a 50-year period between 1927 and 1977, which included 7 new cases of their own and 13 earlier cases previously reported by Payne et al. (6) They reported that the best clinical outcome was seen in the group in which complete resection of the ACC was possible. However, this study also found that some patients had a prolonged survival and minimally associated morbidity, even when residual tumor was knowingly left behind. (6) A previous study (28) on salivary ACCs reported that surgery and postoperative radiotherapy resulted in the best local control but had no impact on overall survival.
The age distribution of our patients was similar to the overall ages of salivary gland ACC patients, but our small series suggests a possible female predominance as opposed to an equal sex distribution reported in salivary ACCs or a male predominance in common primary bronchogenic carcinomas. (8) Over half of our tracheobronchial ACC patients were nonsmokers, as opposed to the presence of a positive smoking history, in most bronchogenic carcinoma patients. Many salivary ACCs initially present as an asymptomatic mass, although 20 to 30% of parotid ACC patients may show facial paralysis or paresthesia at presentation. (8) Most of our patients complained of nonspecific respiratory symptoms such as cough and shininess of breath, which probably were associated with large airway obstruction. Interestingly, some patients were given a clinical diagnosis of asthma due to their prominent wheezing and stridor, which delayed the definitive treatment for years.
There has been controversy as to the prognostic value of histologic grade and perineural invasion in salivary gland ACCs. Some studies (29-34) have reported that grade II and III ACCs, or those with a solid component, follow a significantly worse clinical course, while other studies (28,35,36) failed to demonstrate any correlation between the histologic grade and survival or the incidence of local failure. In a study of 12 cases of ACCs in the trachea and mainstem bronchus, Nomori et al (5) observed that ACCs with tubular/cribriform pattern (grade I) follow an entirely intraluminal growth pattern, while grade III tumors (with [greater than or equal to] 20% solid component) show a predominantly extraluminal growth pattern. In two patients who died of distant tumor metastasis, the tumor showed grade III changes. Thus, they concluded that the histologic grade of tracheobronchial ACCs correlated with the growth pattern and prognosis. (5) A series of 16 primary ACCs of the lung (including 2 patients with distal lung parenchyma as well as 14 patients with endobronchial tumors) reported that the disease stage at diagnosis, but not the histologic features (eg, pattern of growth, cytologic atypia, and mitotic activity), predicted the clinical outcome. (2) This study also suggested that ACCs arising in the lung may possibly behave more aggressively than ACCs in the salivary gland. (2)
In our series, both patients with grade III tumors experienced multiple recurrences, and one had pulmonary metastases. Both patients died, 3 and 8 years after diagnosis. Of the four patients with grade II tumors, two experienced at least one recurrence with lung metastasis, and the remaining two did not have recurrence or metastasis. All four of these patients are known to be alive or are presumed to be alive. Of the eight patients with grade I tumors, six experienced at least one recurrence and three died. Thus, histologic grade as a prognostic factor remained inconclusive in our study of tracheobronchial ACCs. We identified perineural invasion in three patients; however, this did not appear to correlate with histologic grade. Two of the three patients with perineural invasion (cases 1 and 11) were alive with or without evidence of disease, and the remaining patient (case 2) died of disease. Due to the small number of cases, we could not determine the correlation between perineural invasion and survival or prognosis.
CD117 positivity has been proposed as a useful marker for distinguishing ACC from polymorphous low-grade adenocarcinoma, a low-grade carcinoma with a much better long-term prognosis than ACC. (22) We used the same criteria as Penner et al (22) for CD117 scoring in this study to compare results. Our tracheobronchial ACC cases also demonstrated CD117 positivity in a luminal or uniform pattern, an was described. Another previous study (23) reported that CD117 is associated with certain subtypes of salivary gland carcinomas, including ACCs, lymphoepithelioma-like carcinomas, and myoepithelial carcinomas, but not other types of salivary gland carcinomas. Ki-67 is a marker for cell proliferation and has been used as an adjunct to histologic grade or as a prognostic indicator in some tumors. In our study, neither histologic grade nor CD117 positivity correlated with the Ki-67 score.
In summary, ACCs of the tracheobronchial tree appear to behave in a similar biological Fashion and to follow a clinical course similar to that of salivary gland ACCs. Tracheobronchial ACCs consistently showed CD117 expression, as do ACCs of the salivary gland. There were no significant correlations among histologic grade, Ki-67 score, and CD117 positivity. We did not observe conclusive evidence for a correlation between histologic grade or immunohistochemical markers and survival.
REFERENCES
(1) Lawrens JB, Mazur MT. Adenoid cystic carcinoma: a comparative pathologic study of tumors in salivary gland, breast, lung, and cervix. Hum Pathol 1982; 13:916-924
(2) Moran CA, Suster S, Koss MN. Primary adenoid cystic carcinoma of the lung: a clinicopathologic and immunohistochemical study of 16 cases. Cancer 1994; 73:1390-1397
(3) Olofsson J, van Norstrand AWP. Adenoid cystic carcinoma of the larynx: a report of four cases and a review of the literature. Cancer 1977; 40:1307-1313
(4) Conlan AA, Payne WA, Woolner LB, et al. Adenoid cystic carcinoma (cylindroma) and mucoepidermoid carcinoma of the bronchus: factors affecting survival. J Thorac Cardiovasc Surg 1978; 76:369-377
(5) Nomori H, Kaseda S, Kobayashi K, et al. Adenoid cystic carcinoma of the trachea and main-stem bronchus. J Thorac Cardiovasc Surg 1988; 96:271-277
(6) Payne WS, Ellis FH, Woolner LB, et al. The surgical treatment of cylindroma (adenoid cystic carcinoma) and muco-epidermoid tumors of die bronchus. J Thorac Cardiovasc Surg 1959; 38:709-726
(7) Moran CA. Primary salivary gland-type tumors of the lung. Semin Diagn Pathol 1995; 12:106-122
(8) Rice DH. Salivary gland disease: malignant salivary gland neoplasms. Otolaryngol Clin North Am 1999; 32:875-886
(9) Kleer CG, Oberman HA. Adenoid cystic carcinoma of the breast: value of histologic grading and proliferative activity. Am J Surg Pathol 1998; 22:569-575
(10) Arpino G, Clark GM, Mohsin S, et al. Adenoid cystic carcinoma of the breast: molecular markers, treatment, and clinical outcome. Cancer 2002; 94:2119-2127
(11) Trendell-Smith NJ, Peston D. Shousha S. Adenoid cystic carcinoma of the breast: a tumour commonly devoid of oestrogen receptors and related proteins. Histopathology 1999; 35:241-248
(12) Gupta RK, Green C, Naran S, et al. Fine-needle aspiration cytology of adenoid cystic carcinoma of the breast. Diagn Cytopathol 1999; 20:82-84
(13) Shin SJ, Rosen PP. Solid variant of mammary adenoid cystic carcinoma with basaloid features: a study of nine cases. Am J Surg Pathol 2002; 26:413-420
(14) Besmer P, Murphy JE, George PC, et al. A new acute transforming feline retrovirus and relationship of its oncogene v-kit with the protein kinase gene family. Nature 1986; 320:415-421
(15) Yarden Y, Kuang W-J, Yang-Feng T, et al. Human proto-oncogene c-kit: a new cell surface receptor tyrosine kinase for an unidentified ligand. EMBO J 1987; 6:3341-3351
(16) Qiu F, Ray P, Brown K, et al. Primary structure of c kit: Relationship with the CSF-1/PDGF receptor kinase family-oncogenic activation of v-kit involves deletion of extracellular domain and C terminus. EMBO J 1988; 7:1003-1011
(17) de Varies C, Escobedo JA, Ueno H. The fms-like tyrosine kinase, a receptor for vascular endothelial growth factor. Science 1992; 255:898-991
(18) Lammie A, Drobnjak M, Gerald W, et al. Expression of c-kit and kit ligand proteins in normal human tissues. J Histochem Cytochem 1994; 42:1417-1425
(19) Arber DA, Tamayo R, Weiss LM. Paraffin section detection of the c-kit gene product (CD117) in human tissues: value in the diagnosis of mast cell disorders. Hum Pathol 1998; 28:498-594
(20) Demetri GD. Identification and treatment of chemoresistant inoperable or metastatic GIST: experience with the selective tyrosine kinase inhibitor inainib mesylate (STI 571). Eur J Cancer 2002; 38:S52-S59
(21) Holst VA, Marshall CE, Moskaluk CA, et al. KIT protein expression and analysis of c-kit gene mutation in adenoid cystic carcinoma. Mod Pathol 1999; 12:956-960
(22) Penner CR, Folpe AL, Budnick SD. C-kit expression distinguishes salivary gland adenoid cystic carcinoma from polymorphous low-grade adenocarcinoma. Mod Pathol 2002; 15:687-691
(23) Jeng Y-M, Lin C-Y, Hsu H-C. Expression of the c-kit protein is associated with certain subtypes of salivary gland carcinoma. Cancer Lett 2000; 154:107-111
(24) Ueda T, Aozasa K, Tsujimoto M, et al. Prognostic significance of Ki-67 reactivity in soft tissue sarcomas. Cancer 1989; 63:1607-1611
(25) Szanto PA, Luna MA, Tortoledo E, et al. Histologic grading of adenoid cystic carcinoma of the salivary glands. Cancer 1984; 54:1062-1069
(26) Strong MS, Jako GJ. Laser surgery in the larnynx: early clinical experience with continuous C[O.sub.2] laser. Ann Otol Rhinol Layngol 1972; 81:791-798
(27) Duhamel DR, Harrell JH. Laser bronchoscopy. Surg Clin North Am 2001; 11:769-789
(28) Sur RK, Donde B, Levin V, et al. Adenoid cystic carcinoma of the salivary glands: a review of 10 years. Laryngoscope 1997; 107:1276-1289
(29) Greiner TC, Robinson RA, Maves MD. Adenoid cystic carcinoma: a clinicopathologic study with flow cytometric analysis. Am J Clin Pathol 1989; 92:711-720
(30) Fordice J, Kershaw C, El-Naggar A, et al. Adenoid cystic carcinoma of the head and neck: predictors of morbidity and mortality. Arch Otolaryngol Head Neck Surg 1999; 125:149-152
(31) Batsakis JG, Luna MA, El-Naggar A. Histopathologic grading of salivary gland neoplasms: III. Adenoid cystic carcinomas. Ann Oral Rhinol Laryngol 1990; 99:1007-1009
(32) Santucci M, Bondi R. New prognostic criterion in adenoid cystic carcinoma of salivary gland origin. Am J Clin Pathol 1989; 91:132-136
(33) Nascimento AG, Amaral LP, Prado LAF, et al. Adenoid cystic carcinoma of salivary glands: a study of 61 cases with clinico-pathologic correlation. Cancer 1986; 57:312-319
(34) Perzin KH, Gullane P, Clairmont AC. Adenoid cystic carcinoma arising in salivary glands: a correlation of histologic features and clinical course. Cancer 1978; 42:265-282
(35) Spiro RH, Huvos AG. Stage means inure than grade in adenoid cystic carcinoma. Am J Surg 1992; 164:623-628
(36) Kim KH, Sung MW, Chung PS, et al. Adenoid cystic carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg 1994; 120:721-726
Elizabeth Albers, MD; ([dagger]) Thomas Lawrie, MD; ([dagger]) James H. Harrell, MD, FCCP; and Eunhee S. Yi, MD
* From the Departments of Pathology (Drs. Albers and Yi) and Medicine (Drs. Lawrie and Harrell), School of Medicine, University of California San Diego, San Diego, CA.
([dagger]) Drs. Albers and Lawrie contributed equally to the study.
Manuscript received July 31, 2003; revision accepted December 4, 2003.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Eunhee S. Yi, MD, Department of Pathology, University of California San Diego Medical Center, 200 West Arbor Dr, San Diego, CA 92103-8720: e-mail: jeyi@ucsd.edu
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group