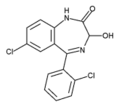
Lorazepam
Lorazepam (marketed under the brand names Ativan®, Temesta®, Tavor®) is a drug which is a benzodiazepine derivative. Pharmacologically, it is classified as a sedative-hypnotic, anxiolytic and anticonvulsant. more...
Pharmacology and pharmacokinetics
Lorazepam is rapidly and nearly completely absorbed after any mode of application (oral, sublingual, i.m., i.v.). The onset of action is several minutes after i.v. injections, 30 to 45 minutes after oral/sublingual administration, and up to 1 hour after i.m. injections.
The duration of action depends on the dose, and is normally 6 to 12 hours. The half-life of lorazepam in patients with normal liver function is 11 to 18 hours. Therefore, 2 to 4 daily doses are often needed.
0.5mg (500µg) of lorazepam is equivalent to 5mg of diazepam . Other experts estimate a proportion of 1mg lorazepam to 5mg diazepam.
Indications
Lorazepam is indicated for:
- Treatment of anxiety disorders
- Short-term treatment of insomnia, particularly if associated with severe anxiety
- Treatment of symptoms associated with alcohol withdrawal
- As a premedication,
- To facilitate unpleasant procedures, such as endoscopies and dental surgery.
- To augment the action of the primary anaesthetic drug.
- To produce varying degrees of anterograde amnesia for the duration of the procedure.
- Long-term treatment of otherwise resistant forms of petit mal epilepsy
- Acute therapy of status epilepticus
- Acute therapy of catatonic states alone/or with haloperidol
- As an initial adjunctive treatment for depressions, mania and psychosis
- Treatment of acute delirium, preferrably together with haloperidol
- Supportive therapy of nausea/emesis frequently associated with cancer chemotherapy, usually together with firstline antiemetics like 5-HT3-antagonists
Lorazepam is available in tablets and as a solution for intramuscular and intravenous injections. It is also available as a parenteral patch.
Dosage
Daily doses vary greatly from 0.5 mg bedtime for insomnia and 2.5 mg every 6 hours and more in the acute treatment of mania, before the firstline drugs (lithium, valproic acid) control the situation.
Catatonia with inability to speak is very responsive and sometimes controlled with a single dose of 2 mg oral or slow i.v. injection. Catatonia may reoccur and treatment for some days may be necessary. Sometimes haloperidol is given concomitantly.
The control of status epilepticus requires slow i.v. injections of 2 to 4 (or even 8) mg. Patients should be closely monitored for respiratory depression and hypotensive effects.
In any case, dose requirements have to be individualized especially in the elderly and debilitated patients in whom the risk of oversedation is greater. Safety and effectiveness of lorazepam is not well determined in children under 18 years of age, but it is used to treat serial seizures. With higher doses (preferably i.v.-doses) the patient is frequently not able to recall unpleasant events (anterograde amnesia) such as therapeutic interventions (endoscopies etc.), which is a desirable effect. But in these cases the risk is given that a patient later makes unjustified allegations of sexual abuse during treatment due to poor recall.
Read more at Wikipedia.org