* Context.-Basaloid squamous cell carcinoma (BSCC) of the esophagus is a rare malignant tumor that morphologically could bear some resemblance to adenoid cystic carcinoma (ACC) originating from salivary glands.
Objective.-The purpose of this study is to describe the histologic, immunohistochemical, and ultrastructural findings of BSCCs of the esophagus, with an emphasis on comparing tumors with or without adenoid cystic features.
Design.-We reviewed 239 cases of primary esophageal carcinoma and detected 12 cases (5%) of BSCC. The light and electron microscopic findings and immunocytochemical localization of various antigens, including cytokeratins (AE1, AE3), carcinoembryonic antigen, epithelial membrane antigen, S100, smooth muscle actin, and p53, were examined in these BSCC cases.
Results.-Histologically, all BSCCs were composed of solid lobules or nests of basaloid cells with well-demarcated outlines surrounded by a fibrous stroma. Seven of 12 tumors showed areas of ACC-like features, that is, cribriform-like pseudoglandular lumina formation and hyaline material surrounding the tumor nests, whereas the remaining 5 tumors were apparently pure basaloid carcinomas. These 2 groups of tumors were histologically and immunohistochemically identical in many aspects, namely, high-grade nuclei of the tumor cells with frequent mitoses, abundant comedo-type necrosis, focal areas of concomitant squamous differentiation, consistent immunoreactivity for cytokeratins, and poor or absent staining for S100 and smooth muscle actin. Ultrastructurally, the basaloid tumor cells exhibited relatively undifferentiated cellular characteristics and undeveloped cell organelles.
Conclusion.-Basaloid squamous cell carcinomas of the esophagus frequently have an intimate association with ACC-like patterns, but their histologie, immunocytochemical, and ultrastructural features correspond more to poorly differentiated squamous cell carcinoma than to salivary gland ACC. This distinction is important because genuine ACC is much less aggressive than BSCC.
(Arch Pathol Lab Med. 2004;128:1124-1130)
Basaloid squamous cell carcinoma (BSCC) is an uncommon variant of squamous cell carcinoma that most commonly affects the upper aerodigestive tract in the region of the hypopharynx, the oral cavity, and the larynx.1*3 In the esophagus, the term basaloid squamous cell carcinoma is relatively new because, in the past, this type of carcinoma was confused with adenoid cystic carcinoma (ACC). Many of the previously reported cases of esophageal ACC would be more properly designated as BSCC.4 Unlike the slow-growing behavioral characteristics of typical salivary gland ACC, most of the esophageal tumors reported as ACC5-9 are aggressive, deeply invasive, and rapidly fatal following diagnosis. Histologically, the basaloid cells are much larger than those of the salivary gland tumors, the nuclei are high grade, and mitoses are common.4,6,10,11 Our review of previously published reports revealed only a few cases that were bona fide examples of ACC.12-14 In view of the apparent behavioral differences between BSCC and typical ACC, it is important to ascertain whether the previously misnamed ACC of the esophagus, a tumor sharing some of the histologie features of ACC, merely represents another unusual histologie variant of squamous cell carcinoma, that is, BSCC. In this report, we describe the histologie, immunohistochemical, and ultrastructural features of 12 BSCCs of the esophagus, with an emphasis on comparing tumors with or without adenoid cystic features.
MATERIALS AND METHODS
Twelve cases of BSCC of the esophagus were selected through histologie review of 239 cases of primary esophageal carcinomas in the surgical pathology files of Linxian County Hospital, Henan, China. Selection criteria for BSCC included the presence of neoplastic basaloid cells forming well-defined nests and lobules, which were clearly distinguishable from squamous cell carcinoma, as described by Wain et al.1 Tumors with or without adenoid cystic differentiation (ie, microcystic or cribriform arrangements and prominent hyaline material surrounding the tumor nests) were evaluated and separated into 2 groups for immunocytochemical and ultrastructural comparison. The 12 BSCC patients included 7 men and 5 women, ranging in age from 48 to 60 years (mean, 55.6 years). Eight tumors arose from the middle portion of the esophagus, 3 from the mid-lower portion, and 1 from the lower portion. Information regarding other clinical details and follow-up was not available for analysis. All the specimens used in this study were resected materials that were fixed in buffered formalin and processed routinely for paraffin embedding. Four-micrometer-thick sections were stained with hematoxylin-eosin, periodic acid-Schiff (PAS), and Alcian blue (pH 2.5). Immunohistochemical studies were performed on paraffin sections using the streptavidin-biotin-peroxidase complex method. The antibodies used were as follows: cytokeratins (clone AEl, clone AE3, ready to use; Zymed Laboratories, South San Francisco, Calif), carcinoembryonic antigen (clone II-7, ready to use; Dako-Cytomation, Carpinteria, Calif), epithelial membrane antigen (clone E29, ready to use; DakoCytomation), SlOO (polyclonal, 1: 100; DakoCytomation), α smooth muscle actin (SMA) (clone 1A4, 1:100; DakoCytomation), and p53 (clone 1801, 1:50; Zymed). To enhance immunostaining, sections were predigested with 0.1% pepsin for cytokeratins and microwave-heated in citrate buffer for p53. Staining was revealed using the LSAB kit (DakoCytomation) and 3,3'-diaminobenzidine (Research Genetics, Huntsville, Ala).
For electron microscopic examination, paraffin-embedded samples of 3 BSCCs (2 of which exhibited adenoid cystic features) were postfixed with a mixture of 2% paraformaldehyde and 2% glutaraldehyde in 0.1M cacodylate buffer (pH 7.2) and were subsequently re-embedded in Poly-Bed 812 resin (Polysciences, Inc, Warrington, Pa). Thin sections were contrasted with uranyl acetate and lead citrate and examined with a Phillips CMlOO transmission electron microscope at 60 kV.
RESULTS
Histopathology
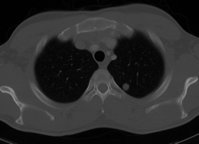
All 12 BSCCs were composed predominantly of solid tumor nests with rounded, sharply demarcated outlines surrounded by a fibrous stroma. The tumor nests or strands were made up of round to ovoid basaloid cells with scanty cytoplasm (Figure 1, a and b). At low power, the tumor cells appeared to be monotonous, yet were found to be more pleomorphic on high-power examination. Mitotic figures were characteristically numerous (Figure 1, c). Atypical mitotic figures were seen frequently. The cells at the edges of the carcinoma nests tended to show peripheral nuclear palisading. Focal areas exhibiting cribriform-like pseudoglandular lumina formation and hyaline material surrounding the tumor nests, resembling ACC, were identified in 7 tumors (Figure 1, d through f). The remaining 5 tumors predominantly contained solid sheets of basaloid cells with no apparent adenoid cystic pattern. Comparison of histologie findings between the 2 groups of lesions is shown in Table 1. In the center of the tumor nests, especially the larger ones, comedo-type necrosis was found in 10 cases (Figure 2, a). Small foci of clear-cut squamous differentiation were seen in 7 cases (Figure 2, b). Carcinoma in situ and/or varying degrees of dysplasia of the surface mucosa epithelium were noted in 3 cases (Figure 2, c [inset]). There appeared to be areas of continuity between the surface epithelium and the underlying tumor (Figure 2, d). The microcytic and intertrabecular spaces were often filled with basophilic mucoid matrix, which was Alcian blue positive but PAS negative (Figure 2, e). The stromal hyaline material surrounding the tumor nests or between the tumor cells was positive for PAS staining (Figure 2, f). The basaloid carcinoma cells were negative for both PAS and Alcian blue.
Immunohistochemistry
Immunohistochemical staining results are summarized in Table 2. Overall, there was no apparent difference in immunostaining for various markers between tumors with or without adenoid cystic features. Reactivity for cytokeratins AEl and AE3 was consistently detected in all BSCCs (Figure 3, a and b). The basaloid component showed poor or patchy staining with SlOO in 3 cases (Figure 3, c), and no positive staining was detected in the cribriform component, despite satisfactory positive internal controls (small nerve bundles staining strongly with SlOO). Patchy SMA staining was detected in only 1 case. The coexistence of 2 distinct cell types, that is, duct-lining cells staining for cytokeratin and myoepithelial cells staining for S100 and SMA, which is typical of ACC, was not identified in any of the tumors. Carcinoembryonic antigen staining appeared to highlight the glandular spaces of the tumor in 4 cases (Figure 3, d). Nuclear p53 immunoreactivity was detected in 6 of the 12 cases (Figure 3, e). Patchy epithelial membrane antigen staining was also noted in 2 cases.
Electron Microscopy
Electron microscopic examination revealed closely packed, medium-sized cells connected by variable numbers of desmosomes. The basaloid cells possessed oval nuclei with scattered chromatin, rare tonofilaments, and moderately developed rough endoplasmic reticulum, mitochondria, and lysosomes. No neurosecretory granules, mucin droplets, microvilli, or myofilaments were identified in the 3 cases examined by electron microscopy. Duplicated basement membrane was observed around the tumor nests or cells in areas showing cribriform pattern in light microscopy (Figure 3, f). Cystlike spaces were also seen in some areas.
COMMENT
Basaloid squamous cell carcinoma, first characterized by Wain et al,1 is a rare but distinctive malignant tumor occurring mainly at the upper aerodigestive tract, especially the larynx, pharynx, and base of tongue. More than 100 cases of BSCC of the head and neck have been described to date.1-3,15 In the esophagus, it seems that many cases of BSCC had been reported previously as ACC, as Tsang et al demonstrated.4 Considering the delayed recognition of this neoplasm, the true incidence of BSCC in the esophagus is still uncertain. The 3 recently reported series found quite different relative incidences (1.9%,10 3.6%,16 and 11.3%11). Our 12 cases constituted 5% of 239 cases of esophageal cancer from Linxian County, a region known for having a high incidence of esophageal cancers in China.
Apart from a few reported genuine ACCs of the esophagus,12-14 most of the cases reported as ACC of the esophagus showed significant differences in comparison to the typical ACC in the salivary gland.4-11 From a review of the literature4-11,16 and our own series, we found that esophageal BSCC occurs more often in males, with a mean age around 55 to 60 years. These features correspond more closely to squamous cell carcinoma of the esophagus than to salivary gland ACC, which tends to have a female preponderance and earlier age of occurrence.1718 Histologically, the esophageal BSCCs in our series, including those with adenoid cystic pattern, differed from typical ACC of the salivary gland in several important respects. Although the microcystic or cribriform pattern was identifiable in 7 of our cases, there appeared to be a greater tendency to formation of solid or basaloid areas than would be expected in typical salivary gland lesions. Confluent (comedo-type) necrosis was a frequent finding, but this feature is rarely seen in salivary gland ACC. While both tumor types appear to be composed of small basaloid cells at low power, high-power examination of the lesions in our series showed a significantly greater degree of nuclear pleomorphism, a more "crowded" nuclear appearance, and in particular, a considerably increased mitotic rate in comparison to typical salivary gland lesions. Tumors of the present series, irrespective of the presence or absence of adenoid cystic features, all revealed prominent mitotic activity and a significant degree of cellular pleomorphism. Coexistence of a squamous component or continuity to the surface squamous epithelium was frequently observed in the present series, but this has not been reported as a feature of salivary gland ACC. Our findings therefore support previous studies that suggested that many cases of "ACC" of the esophagus were in fact BSCCs with adenoid cystic features.
The immunocytochemical profiles of the BSCCs with or without adenoid cystic features were similar, providing further evidence that they represent the same tumor type. A remarkable feature was the poor or absent immunoreactivity for SlOO and SMA in the basaloid as well as cribriform components of the BSCCs. This is in striking contrast to the consistent S100/SMA immunoreactivity in the basaloid tumor cells of salivary gland ACC.1"20 These results, in general agreement with several previous studies,341021 suggest that BSCC, with or without adenoid cystic features, is not an ACC. The p53-positive rate of 50% in our series is quite similar to that of typical squamous cell carcinoma of the esophagus.11,22,23 Ultrastructurally, although densely replicated basement membrane (a known ultrastructural feature of ACC) was frequently observed in areas showing microcystic or cribriform arrangement, the basaloid tumor cells exhibited relatively undifferentiated cellular characteristics and undeveloped cell organelles, thus lacked features of myoepithelial differentiation. There were no apparent differences between tumor cells in the solid/basaloid areas and those in the microcystic or cribriform areas. These ultrastructural features, which were also described in several previous stu0 dies,1,10,16 appeared to confirm that the tumor cells were not myoepithelial cells, a predominant cellular component of typical ACC.
Regarding its biologic behavior, it is widely believed that BSCC is more aggressive than typical ACZC and its course more closely parallels that of squamous cell carcinoma of the esophagus.1,4,6,10,11,15,16 The histogenesis of esophageal BSCC remains open to question. Several origins have been postulated, such as the embryonal rests of the tracheobronchial tree,24 submucosal glands or their intercalated ducts, or surface epithelium.5 7 Based on our observations as well as previously presented evidence,1,6,10,11,16 we agree with Tsang et al4 that BSCC of the esophagus originates from a totipotent primitive cell of the surface epithelium that is capable of differentiating focally into epithelial structures, myoepithelium, or other elements. The tumor can probably be viewed as a peculiar variant of poorly differentiated squamous cell carcinoma. The associated dysplastic changes in the esophageal mucosa, the intimate relationship of the tumors with the surface epithelium, and the focal identifiable areas of squamous differentiation within a BSCC, as demonstrated in the present series, all lend support for this hypothesis. On the other hand, the reported extremely rare cases of true esophageal ACC have typically presented as intramural masses presumably corresponding to an origin in the submucosal glands located in the proximal and distal esophagus.
In conclusion, our findings support the idea that many cases previously labeled ACC of the esophagus are in fact BSCCs with adenoid cystic features. An intimate association between a basaloid component and ACC-like areas is frequently encountered in esophageal BSCC, but these tumors have noticeable morphologic differences when compared with typical salivary gland ACCs. Basaloid squamous cell carcinoma of the esophagus appears to be a distinctive variant of squamous cell carcinoma and should therefore be differentiated from the less aggressive ACCs.
References
1. Wain SL, Kier R, Vollmer RT, Bossen EH. Basaloid-squamous carcinoma of the tongue, hypopharynx, and larynx: report of 10 cases. Hum Pathol. 1986; 17: 1158-1166.
2. Batsakis JG, EI-NaggarA. Basaloid-squamous carcinomas of the upper aerodigestive tracts. Ann Otol Khinol Laryngol. 1989:98:919-920.
3. Banks ER, Frierson HF, Mills SE, George E, Zarbo R), Swanson PE. Basaloid squamous cell carcinoma of the head and neck: a clinicopathologic and immunohistochemical study of 40 cases. Am I Surg Pathol. 1992:104:594-598.
4. Tsang WYW, Chan IKC, Lee KC, Leung AKF, Fu YT. Basaloid-squamous carcinoma of the upper aerodigestive tract and so-called adenoid cystic carcinoma of the esophagus: the same tumor type? Histopathology. 1991:19:35-46.
5. Sweeney EC, Cooney T. Adenoid cystic carcinoma of the esophagus: a light and electron microscopic study. Cancer. 1980:45:1516-1525.
6. Epstein Jl, Sears DL, Tucker RS, Eagan JW |r. Carcinoma of the esophagus with adenoid cystic differentiation. Cancer. 1984:53:1131-1136.
7. Pourzand A, Freant L, Levin R, Peabody ], Absolon K. Primary adenoid cystic carcinoma of the esophagus: report of a case and review of the literature. ) Thorac Cardiovasc Surg. 1975:69:785-789.
8. AIIard M, Farkouh E, Atlas H, Paquin JG. Primary adenoid cystic carcinoma of the esophagus. Can / Surg. 1981:24:405-406.
9. Mukada T, Sato E. Adenoid cystic carcinoma of the esophagus. Tohoku I Exp Med. 1974:113:257-262.
10. Abe K, Sasano H, ltakura Y, NishihiraT, Mori S, Nagura H. Basaloid-squamous carcinoma of the esophagus: a clinicopathologic, DNA ploidy, and immunohistochemical study of seven cases. Am I Surg Pathol. 1996:20:453-461.
11. Cho KJ, Jang JJ, Lee SS, Zo Jl. Basaloid squamous carcinoma of the esophagus: a distinct neoplasm with multipotential differentiation. Histopathology. 2000:36:331-340.
12. Kabuto T, Taniguchi K, Iwanaga T, et al. Primary adenoid cystic carcinoma of the esophagus: report of a case. Cancer. 1979;43:2452-2456.
13. Nelms DC, Luna MA. Primary adenocystic carcinoma (cylindromatouscarcinoma) of the esophagus. Cancer. 1972;29:440-443.
14. Zardawi IM,TalbotlC. Primary adenoid cystic carcinoma of theesophagus. Diagn Histopathol. 1983:6:39-46.
15. Barnes L, Ferlito A, Altavilla G, MacMillan C, Rinaldo A, Doglioni C. Basaloid squamous cell carcinoma of the head and neck: clinicopathologic features and differential diagnosis. Ann Otol Rhinol Laryngol. 1996:105:75-82.
16. Sarbia M, Vereet P, Bittinger F, et al. Basaloid squamous cell carcinoma of the esophagus: diagnosis and prognosis. Cancer. 1997;79:1871-1878.
17. Spiro RH, Huvos AG, Strong EW. Adenoid cystic carcinoma of salivary origin: a clinicopathologic study of 242 cases. Am / Surg. 1974:128:512-520.
18. Perzin KH, Gullane P, Clairmont A. Adenoid cystic carcinomas arising in salivary glands: a correlation of histologie features and clinical course. Cancer. 1978:42:265-282.
19. Azumi N, Battifora H. The cellular composition of adenoid cystic carcinoma: an immunohistochemical study. Cancer. 1987;60:1 589-1 598.
20. Crocker J, Jenkins R, Campbell ), FuggleWj, Shah VM. Immunohistochemical demonstration of S-100 protein in salivary gland neoplasms. J Pathol. 1985; 146:115-121.
21. Hishida T, Nakanishi Y, Shimoda T, et al. Esophageal basaloid carcinoma with marked myoepithelial differentiation. Pathol Int. 2002:52:313-317.
22. Yang G, Zhang Z, Liao J, et al. Immunohistochemical studies on Waf1p21, p16, pRb and p53 in human esophageal carcinomas and neighboring epithelium from a high-risk area in northern China, lnt J Cancer. 1997;72:746-751.
23. Rarenti AR, Ruggc M, Shiao YH, et al. bcl-2 and p53 immunotypes in preinvasive, early and advanced esophageal squamous cancer. Histopslhology. 1997:31:430-435.
24. Bergmann M, Charnas RM. Tracheobronchial rests in the esophagus, their relation to some benign structures and certain types of cancer of the esophagus. Thorac Surg. 1958;35:97-104.
Tie-jun Li, PhD; Yong-Xin Zhang, MD, PhD; Julie Wen, MS; Daniel F. Cowan, MD; John Hart, MD; Shu-Yuan Xiao, MD
Accepted for publication June 10, 2004.
From the Department of Oral Pathology, Peking University School of Stomatology, Beijing, People's Republic of China (Dr Li); the Department of Pathology, University of Chicago Hospitals, Chicago, III (Drs Zhang and Hart); and the Department of Pathology, University ofTexas Medical Branch, Calveston (Ms Wen and Drs Cowan and Xiao).
The authors have no relevant financial interest in the products or companies described in this article.
Reprints: Shu-Yuan Xiao, MD, Department of Pathology, Route 0588, University ofTexas Medical Branch, 301 University Blvd, Galveston, TX 77550 (e-mail: syxiao@utmb.edu).
Copyright College of American Pathologists Oct 2004
Provided by ProQuest Information and Learning Company. All rights Reserved