Abstract
We retrospectively reviewed 35 cases of adenoid cystic carcinoma that had originated in the minor salivary glands of the paranasal sinuses or nasal cavity. All patients had been seen at two tertiary-care referral centers in western New York State between 1960 and 2000. Twenty patients had been treated with surgery and adjuvant radiotherapy, 10 patients with surgery alone, three with radiotherapy alone, and two with concurrent radiotherapy and chemotherapy. During the study, 22 patients developed recurrent disease--11 locally; three distantly; seven locally and distantly; and one locally, regionally, and distantly. At the conclusion of the study, 14 patients were alive and disease-free, and eight were alive with disease; 10 patients had died with disease, and three had died of other causes with no evidence of disease. Adenoid cystic carcinoma of the paranasal sinuses or nasal cavity is an aggressive neoplasm that results in a high incidence of both local recurrence and distant metastasis, regardless of treatme nt modality. Most cases are ultimately fatal, although long disease-free intervals have been observed. A combination of surgery and radiotherapy offers these patients the best chance for disease control.
Introduction
Adenoid cystic carcinoma is an uncommon tumor that accounts for fewer than 1% of all head and neck malignancies and 10% of all salivary gland neoplasms. (1,2) It occurs more often in the minor salivary glands than in the major salivary glands. (1,2) The paranasal sinus is the most common site of minor salivary gland involvement. (1,3-5) Of all malignant paranasal sinus tumors, 5 to 15% are adenoid cystic carcinomas. (4) As with other sinus tumors, its onset can be insidious. (6) On initial evaluation, most patients have advanced disease. The complexity of the local anatomy can make treatment difficult. (7)
Adenoid cystic carcinoma is a slowly progressive and relentless tumor that has a tendency to recur locally and metastasize distantly. (8,9) Recurrence and metastasis can occur even decades after treatment of the primary tumor. (10) This has led some authors to consider adenoid cystic carcinoma to be an incurable neoplasm. (11,12) The steadfastness of this tumor is partially attributable to its ability to extend through submucosal and fibrous tissue planes around the primary site and its tendency for perineural spread along major and minor nerves. (2,13) It is by examining the clinical characteristics, treatments, and outcomes of patients with adenoid cystic carcinoma of the paranasal sinuses or nasal cavity that we can develop an understanding of this rare and unusual malignancy.
Patients and methods
We identified all patients who had come to our institutions between 1960 and 2000 with adenoid cystic carcinoma that had originated in the minor salivary glands of the paranasal sinuses or nasal cavity. The two centers are the Roswell Park Cancer Institute and the University of Rochester Medical Center, both located in western New York State. Data were obtained from medical charts in a retrospective manner. Our primary goals were to ascertain the pattern of recurrence, treatment response, and survival. The median follow-up was 5 years.
Results
Demographics. We identified 35 patients--17 men and 18 women, aged 18 to 82 years (mean: 57)--who had a histologic diagnosis of adenoid cystic carcinoma of the paranasal sinuses or nasal cavity. Twenty-five patients had newly diagnosed tumors and 10 patients presented with recurrent disease.
Tumor location and staging. Tumors were located in the maxillary sinus in 19 patients, the nasal cavity in 10, and the ethmoid sinus in six. Twenty-six patients (74.3%) had advanced disease at the time of our initial evaluation; overall, nine patients had stage II tumors, 10 patients were stage III, 14 were stage IV-A, and two were stage IV-C. (14) No patient had any evidence of cervical lymph node metastasis at the initial evaluation, although two had a distant metastasis.
Overall survival. Overall survival rates were 65% at 5 years, 55% at 10 years, and 28% at 15 years (figure 1). Of the 13 patients who had died during the study, 10 died of disease and three died of other causes without evidence of disease. At the conclusion of the study, 14 patients were alive and disease-free and eight patients were alive with disease.
Mode of therapy. Of the 35 patients, 20 had been treated with a combination of surgery and adjuvant radiotherapy, 10 patients with surgery alone, three with radiotherapy alone, and two with concurrent radiotherapy and chemotherapy (table 1). Of the 30 patients who had surgery, 26 underwent procedures that included maxillectomy, six underwent orbital exenteration, and three underwent craniofacial resection. All gross disease was removed in all surgically treated patients. However, despite aggressive surgery, 19 of the 30 (63.3%) had positive margins on postoperative microscopic examination.
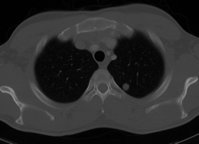
Metastatic disease. Overall, the lung was the most common site of metastatic disease (10 patients); other sites were bone (5), the liver (3), the brain (1), the kidney (1), the spleen (1), and the spine (1).
Patients presenting with recurrent disease. All 10 patients who presented with recurrent disease had been previously treated with local excision at other institutions; none had undergone previous radiotherapy. All came to our institutions with local disease. We treated five of these patients with surgery plus radiation, four with surgery alone, and one with radiation alone (table 2). Despite our treatment, new local recurrences and distant metastases were common. Seven of the 10 patients eventually died of disease. Among the three who remained alive at study's end, two had recurrent disease and one had no evidence of disease.
Patients presenting with primary tumors. Among the 25 patients who had received primary treatment at our institutions, 15 underwent surgery plus radiation, six had surgery alone, and four had radiation with or without chemotherapy (table 3). Again, local recurrences and/or distant metastases were common, developing in eight of the 15 patients who underwent surgery plus radiation, in four of the six who underwent surgery alone, and in all four who underwent radiation with or without chemotherapy. Patients in the surgery-alone group had a higher rate of local recurrence (4/6 [66.7%]) than did those in the surgery-plus-radiation group (5/15 [33.3%]), but they also had a higher 10-year survival rate (67 vs 57%; p = 0.49), according to Kaplan-Meier calculations (figure 2). However, none of these differences was statistically significant.
In the surgery-plus-radiation group, the eight patients who developed a local recurrence or distant metastasis had received a mean total postoperative radiation dose of 6,023 cGy, while the seven who remained disease-free received a mean dose 5,930 cGy.
Among the 25 patients who presented with primary disease, tumor site did not correlate with disease recurrence. Recurrence developed in four of five patients who had ethmoid tumors (80.0%), five of 12 with antral tumors (41.7%), and three of eight with nasal cavity tumors (37.5%).
There was a trend toward an increase in the incidence of local recurrence with higher T stage, but the correlation was not statistically significant. Local recurrence developed in two of seven patients who had a T2 tumor (28.6%), three of seven with a T3 tumor (42.9%), and six of 11 with a T4 tumor (54.5%).
Among the 21 primary-treatment patients who underwent surgery, 12 had microscopically positive surgical margins and nine had negative margins. Local recurrence was more common in patients with positive margins. The percentages of combined local recurrences and distant metastases in the two groups were similar--58.3 % (7/12) among patients with positive margins and 55.6% (5/9) in those with negative margins. However, the 10-year survival rate among patients with positive margins was only 43%, compared with 75% for those with negative margins, although the difference was not statistically significant (p = 0.13) (figure 3).
Discussion
Adenoid cystic carcinoma originating in the minor salivary glands of the paranasal sinuses and nasal cavity was described in 1962 by Tauxe et al as a cancer that "pursues [its] course relentlessly and maliciously." (15) They added that "few more horrible deaths can be imagined," as patients must endure "severe pain, paresthesia, blindness, dysphagia, deafness, dysarthria, and facial disfigurement that [occurs] over long periods and with ever increasing intensity." Of all patients with adenoid cystic carcinoma of the head and neck, those whose disease originates in the paranasal sinuses or nasal cavity have the poorest prognosis. (16,17) This finding was described by Leafstedt et al in a review from the Roswell Park Cancer Institute more than 30 years ago. (16)
Surgical margins. Most of our surgical patients (63.3%) had positive microscopic margins despite aggressive surgery, including maxillectomy, orbital exenteration, and craniofacial resection. The proximity of the tumors to the skull base and the major nerves combined with the tumor's tendency to spread perineurally contributed to the difficulty in obtaining surgical margins free of microscopic disease. In our series, the primary-treatment patients who had positive margins experienced local recurrences at a higher rate than did those with negative margins (41.7 vs 22.2%; p = 0.34).
The tendency toward local recurrence in patients with positive margins might be explained by the biologic behavior of adenoid cystic carcinoma. Howard and Lund reported histologic evidence of an embolic pattern of perineural spread in paranasal sinus adenoid cystic carcinoma. (18) Their findings called into question the value of negative microscopic surgical margins in these patients. Clear margins might correlate with better local control but not with better survival, Support for this theory has been expressed by other investigators. (12,19)
Our data suggest that despite the difficulty of achieving negative margins, doing so does appear to confer some benefit. Therefore, we believe that aggressive surgical treatment is indicated. However, the aggressiveness and extent of surgery should be tempered by quality-of-life considerations. For example, the removal of a normally functioning eye in order to clear a microscopic surgical margin is of questionable benefit.
Haddad et al suggested that positive surgical margins might be a reflection of a disease that is more aggressive, invasive, and resistant rather than a reflection of inadequate resection. (2) The possibility that positive margins are a marker for more aggressive disease warrants further study.
Surgery plus radiotherapy vs surgery alone. There was no statistically significant difference in our series in overall survival rates between patients who were treated with surgery plus adjuvant radiotherapy and those treated with surgery alone. Adenoid cystic carcinoma is considered to be a radiosensitive but not radiocurable tumor. (16,20) The rationale for administering postoperative radiation therapy is that it treats residual microscopic disease, which is present in most patients.
Our findings are consistent with those of Spiro et al, who wrote that postoperative irradiation most likely delays rather than prevents local recurrence. (21) In our patients, the mean time to the development of recurrent disease was 4 years and 2 months following surgery plus radiotherapy, and 3 years and 11 months following surgery alone--a difference of 3 months. Other authors have recognized the importance of adjuvant radiation in controlling disease in patients with adenoid cystic carcinoma of the head and neck. (1,8,13,22,23) Adjuvant radiation following surgical resection is the mainstay of treatment for patients with adenoid cystic carcinoma of the paranasal sinuses or nasal cavity.
Metastatic and recurrent disease. Unlike other head and neck cancer patients, patients with adenoid cystic carcinoma of the paranasal sinuses or nasal cavity often survive for long periods of time with distant metastatic disease. (1,16,24) In our series, patients whose initial sign of recurrence was a distant metastasis had a mean survival of 2 years and 5 months (range: 5 mo to 12 yr 6 mo). Therefore, the presence of distant metastatic disease is not a contraindication to surgical treatment of the primary tumor in order to achieve local control. Cervical lymph node metastasis of adenoid cystic carcinoma is rare, (7,12) and no patient in our series presented with such.
Only one of our patients developed a recurrence in the neck; this patient had a particularly aggressive tumor and died within 6 months of surgery, with local recurrence, cervical node metastasis, and distant metastases to the bone and liver. The predilection of adenoid cystic carcinoma to spread hematogenously and perineurally but not lymphatically has been noted by other authors. (4,7,12)
Future study. Further investigation of the role of adjuvant chemotherapy combined with surgery and/or radiation needs to be carried out. As well, patients with adenoid cystic carcinoma of the paranasal sinuses or nasal cavity undergo treatments that are associated with very significant morbidity for a disease to which most will eventually succumb. It is therefore critical that quality-of-life issues be addressed in this patient population.
[FIGURE 1 OMITTED]
[FIGURE 2 OMITTED]
[FIGURE 3 OMITTED]
References
(1.) Kim KH, Sung MW, Chung PS, et al. Adenoid cystic carcinoma of the head and neck. Arch Otolaryngol Head Neck Surg 1994;120:721-6.
(2.) Haddad A, Enepekides DJ, Manolidis S, Black M. Adenoid cystic carcinoma of the head and neck: A clinicopathologic study of 37 cases. J Otolaryngol 1995;24:201-5.
(3.) Spiro RH, Huvos AG, Strong EW. Adenoid cystic carcinoma of salivary origin. A clinicopathologic study of 242 cases. Am J Surg 1974;128:512-20.
(4.) Kim GE, Park HC, Keum KC, et al. Adenoid cystic carcinoma of the maxillary antrum. Am J Otolaryngol 1999:20:77-84.
(5.) Miller RH, Calcaterra TC. Adenoid cystic carcinoma of the nose, paranasal sinuses, and palate. Arch Otolaryngol 1980:106:424-6.
(6.) Kraus DH, Roberts JK, Medendorp SV, et al. Nonsquamous cell malignancies of the paranasal sinuses. Ann Otol Rhinol Laryngol 1990;99:5-11.
(7.) Naficy S, Disher MJ, Eselamado RM. Adenoid cystic carcinoma of the paranasal sinuses. Am J Rhinol 1999;13:311-4.
(8.) Vikram B, Strong EW, Shah JP, Spiro RH. Radiation therapy in adenoid-cystic carcinoma. Int J Radiat Oncol Biol Phys 1984;10:221-3.
(9.) Tran L, Sidrys J, Horton D, et al. Malignant salivary gland tumors of the paranasal sinuses and nasal cavity. The UCLA experience. Am J Clin Oncol 1989;12:387-92.
(10.) Fordice J, Kershaw C, EI-Naggar A, Goepfert H. Adenoid cystic carcinoma of the head and neck: Predictors of morbidity and mortality. Arch Otolaryngol Head Neck Surg 1999;12S:149-52.
(11.) Dal Maso M, Lippi L. Adenoid cystic carcinoma of the head and neck: A clinical study of 37 cases. Laryngoscope 1985;95:177-81.
(12.) Chilla R, Schroth R, Eysholdt U, Droese M. Adenoid cystic carcinoma of the head and neck. Controllable and uncontrollable factors in treatment and prognosis. ORL J Otolaryngol Relat Spec 1980;42:346-67.
(13.) Goepfert H, Luna MA, Lindberg RD. White AK. Malignant salivary gland tumors of the paranasal sinuses and nasal cavity. Arch Otolaryngol 1983;109:662-8.
(14.) American Joint Committee on Cancer Staging. Cancer Staging Handbook. AJC Cancer Staging Manual. 5th ed. Philadelphia: Lippincott-Raven, 1998:51-5.
(15.) Tauxe WN, McDonald JR. Devine KD. A century of cylindromas. Arch Otolaryngol 1962;75:94-106.
(16.) Leafstedt SW, Gaeta JF, Sako K, et al. Adenoid cystic carcinoma of major and minor salivary glands. Am J Surg 197 l;122:756-62.
(17.) Cleveland D, Abrams AM, Melrose RJ, Handlers J. Solid adenoid cystic carcinoma of the maxilla. Oral Surg Oral Med Oral Pathol 1990;69:470-8.
(18.) Howard DJ, Lund VJ. Reflections on the management of adenoid cystic carcinoma of the nasal cavity and paranasal sinuses. Otolaryngol Head Neck Surg 1985;93:338-41.
(19.) Garden AS, Weber RS, Morrison WH, et al. The influence of positive margins and nerve invasion in adenoid cystic carcinoma of the head and neck treated with surgery and radiation. Int J Radiat Oncol Biol Phys 1995;32:619-26.
(20.) Berdal P. de Besehe A. Mylius E. Cylindroma of salivary glands. A report of 80 cases. Acta Otolaryngol Suppl 1969;263:170-3.
(21.) Spiro RH, Huvos AG, Strong EW. Adenoid cystic carcinoma: Factors influencing survival. Am J Surg 1979;138:579-83.
(22.) MeNicoll W, Hopkin N, Dailey VM, Shaw HJ. Cancer of the paranasal sinuses and nasal cavities. Part II. Results of treatment. J Laryngol Otol 1984;98:707-18.
(23.) Konno A, Ishikawa K, Numata T, et al. Analysis of factors affecting long-term treatment results of adenoid cystic carcinoma of the nose and paranasal sinuses. Acta Otolaryngol Suppl 1998;537:67-74.
(24.) Spiro RH, Koss LG, Hajdu SI, Strong EW. Tumors of minor salivary origin. A clinicopathologic study of 492 cases. Cancer 1973;31:117-29.
From the Roswell Park Cancer Institute, Buffalo, N.Y. (Dr. Wiseman, Dr. Rigual, Dr. Hicks, Dr. Orner, and Dr. Loree), and the University of Rochester (N.Y.) Medical Center (Dr. Popat. Dr. Wein, and Dr. McGary).
Reprint requests: Thorn R. Loree, MD, Department of Head and Neck Surgery, Roswell Park Cancer Institute, Elm and Carlton Sts., Buffalo, NY 14263. Phone: (716) 845-3158; fax: (716) 845-8646; e-mail: thom.loree@roswellpark.org
COPYRIGHT 2002 Medquest Communications, LLC
COPYRIGHT 2002 Gale Group