Abstract
Compared with total parotidectomy and complete superficial parotidectomy for the removal of aparotidpleomorphic adenoma, partial superficial parotidectomy with dissection and preservation of the facial nerve--defined as the excision of a tumor with a 2-cm margin of normal parotid parenchyma except at the point where the tumor abuts' the facial nerve--is associated with a lower incidence of transient facial nerve dysfunction, facial contour disfigurement and subsequent Frey's syndrome. The partial procedure is not associated with any increase in recurrence, and it requires less operating time. The author hypothesized that the use of this procedure to remove a benign pleomorphic adenoma might result in even less morbidity (transient or permanent facial nerve dysfunction, facial contour disfigurement, Frey's syndrome, and hypoesthesia) without increasing the risk of recurrence if only a 1-cm margin of normal parotid parenchyma was removed and if the posterior branches of the great auricular nerve were preserved. To test this hypothesis, the author conducted a retrospective study of 30 patients--15 who had undergone the standard partial procedure (2-cm margin with great auricular nerve sacrifice) and 15 who had undergone the modified version (1-cm margin with great auricular nerve preservation). After a mean follow-up of 10 years, there were no significant differences between the two groups in terms of facial nerve dysfunction, facial contour disfigurement, Frey's syndrome, and recurrence. Moreover, preservation of the posterior branches of the great auricular nerve did not prevent alterations in sensitivity (i.e., hypoesthesia) in 7 of the 15 patients (46.7%). Although a 1-cm area of normal parotidparenchyma around a benign pleomorphic adenoma was a safe margin, it was no better than a 2-cm margin in terms of morbidity and recurrence. Preservation of the posterior branches of the great auricular nerve will result in an objective reduction in hypoesthesia in approximately half of patients, but because it does not ensure freedom from sensitivity alterations in all cases, patients should be advised of the risk of postoperative numbness in the earlobe and the infraauricular area.
Introduction
For the purpose of this article, standard partial superficial parotidectomy with dissection and preservation of the facial nerve is defined as the excision of a 2-cm margin of normal parotid parenchyma except at the point where the tumor abuts the facial nerve. Compared with total parotidectomy and complete superficial parotidectomy, partial superficial parotidectomy is associated with a lower incidence of transient facial nerve dysfunction, facial contour disfigurement, and subsequent Frey's syndrome (auriculotemporal syndrome: localized sweating and flushing of the ear and cheek in response to eating). (1) The partial procedure is not associated with any increase in recurrence rates, and it requires less operating time. (1)
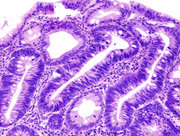
During parotidectomy, the great auricular nerve, located near the posterior border of the sternocleidomastoid muscle and anterior to the mastoid tip, is often sacrificed at the parotid inferior pole. This sacrifice results in numbness, primarily in the earlobe and infraauricular area. (2) Patients with postparotidectomy hypoesthesia can experience traumatic lesions because they are unable to appreciate pain there. (3) Most great auricular nerves have one or two anterior branches and two posterior branches (a superficial branch and a deep branch). The posterior nerve branches can often be preserved during parotidectomy by carefully dissecting them until they pass away from the surgical field and into the subcutaneous tissue of the earlobe (figure).
[FIGURE OMITTED]
The author hypothesized that partial superficial parotidectomy with facial nerve dissection and preservation might result in even less morbidity if only a 1-cm margin of normal parotid parenchyma was removed and the posterior branches of the great auricular nerve were preserved. To test this hypothesis, the author conducted a retrospective study of 30 patients.
Patients and methods
Patient characteristics. The author reviewed the records of 30 patients who had undergone partial superficial parotidectomy for the treatment of parotid pleomorphic adenoma between 1986 and 1998. This group was made up of 15 patients who had undergone the standard partial procedure with a 2-cm margin of normal parotid parenchyma and sacrifice of the great auricular nerve (group A), and a matched group of 15 patients who had undergone the modified version with a 1-cm margin and preservation of the posterior branches of the great auricular nerve (group B). In both groups, the facial nerve was dissected and preserved.
Group A was made up of 12 women and 3 men aged 23 to 78 years (mean: 45); group B included 11 women and 4 men aged 25 to 73 years (mean: 42).
Most patients in group A were treated during the first half of the study period and vice versa.
Tumor characteristics. Preoperatively, all tumors were mobile parotid pleomorphic adenomas located in the superficial lobe; none exhibited any clinical or cytologic evidence of malignancy. All tumors were smaller than 4 cm; tumor sizes ranged from 1.0 to 3.2 cm (mean: 2.0) in group A and 0.8 to 3.1 cm (mean 2.0) in group B.
Intraoperatively, a sterile ruler or calipers was used to measure the margin of normal parotid parenchyma around each tumor except at the point where the tumor abutted the facial nerve. A margin of normal parotid parenchyma around the tumor can be obtained except where the tumor abuts the facial nerve or superficial fascia, a nearly universal finding in parotid surgery for pleomorphic ademona.
Tactile sensation. Postoperatively, tactile sensation was evaluated 1 week postoperatively and again at a follow-up of at least 1 year. Tactile sensitivity was assessed by placing a wisp of cotton on the surface of both the earlobe and the infraauricular area on two separate occasions. With their eyes closed, patients were asked to indicate where they felt the wisp of cotton. A failure to correctly identify the presence of the cotton at both sites on either attempt was considered to be indicative of hypoesthesia.
Frey's syndrome. The presence or absence of Frey's syndrome was evaluated by subjective complaint. No patient underwent a Minor's starch-iodine test. (During this test, a solution of iodine, castor oil, and absolute alcohol is applied to the patient's cheek and then dusted with powder.) Almost all patients who undergo Minor's test will exhibit objective Frey's syndrome. Approximately 10% of patients who undergo partial superficial parotidectomy report subjective Frey's syndrome. (1)
Operating time. The length of each operation--from the initial incision to the completed wound closure was recorded.
Long-term follow-up. The overall length of follow-up ranged from 6 to 17 years (mean: 12) for patients in group A and 4 to 13 years (mean: 8) for those in group B. The mean length of follow-up for the entire study population was 10 years.
Results
Facial nerve dysfunction. At both short- and long-term follow-up, the author found no differences between the two groups in terms of facial nerve dysfunction. In fact, no patient in either group experienced any permanent dysfunction. Transient facial nerve dysfunction occurred in 2 patients in group A (13.3%) and in 3 patients in group B (20.0%), but in no case did the degree of temporary paresis exceed House grade III. (4)
Facial contour disfigurement. Likewise, no patient in either group experienced facial contour disfigurement, and none felt that reconstructive surgery for neck deformity was necessary.
Tactile sensation. At the 7-day follow-up, all patients in both groups experienced tactile hypoesthesia of the earlobe and/or infraauricular area. However, at the 1-year follow-up, tactile sensation had returned to 8 of the group B patients (53.3%), compared with none of the group A patients. Although this difference is certainly significant, it does indicate that preservation of the posterior branches of the great auricular nerve does not prevent alterations in sensitivity in all patients. Of the 7 patients in group B whose tactile sensitivity was not preserved, 5 (33.3%) had earlobe hypoesthesia and all 7 (46.7%) had infraauricular hypoesthesia.
Frey's syndrome. Subjective Frey's syndrome occurred in 1 patient in each group (6.7%).
Operating time. The length of operating time ranged from 80 to 175 minutes (mean: 110) in group A and from 80 to 190 minutes (mean: 119) in group B--not a significant difference.
Long-term recurrence. There was no recurrence in either group on long-term follow-up (mean: 10 yr).
Discussion
Narrowing the width of the normal parotid parenchyma margin surrounding a benign pleomorphic adenoma from 2 to I cm resulted in no significant difference in the incidence of permanent or transient facial nerve dysfunction, facial contour disfigurement, or Frey's syndrome.
Long-term recurrence. Based on findings during long-term follow-up, the modified partial procedure was not associated with any increase in the risk of recurrence of parotid pleomorphic adenoma, as the recurrence rate in both groups was 0%. A 1-cm margin would therefore appear to be a safe margin. However, it is possible that a recurrence might still occur beyond the follow-up period in this series (mean: 10 yr).
At the point where a benign pleomorphic adenoma abuts the facial nerve, parotidectomy with facial nerve dissection and preservation involves a controlled partial enucleation. Low rates of recurrence are reported because a margin of normal parotid parenchyma is obtained at points where the tumor does not abut the nerve. A 1-cm margin appears to be a safe margin for benign pleomorphic adenoma. Subcentimeter margins may result in higher recurrence rates because of an inadvertent entry into the pseudocapsule and rupture of the tumor.
Tactile sensation. A significant number of patients in group B (7 of 15 [46.7%]) experienced a tactile sensory deficit despite preservation of the posterior branches of the great auricular nerve. This finding is consistent with studies by other authors, who have reported persistent earlobe and infraauricular hypoesthesia in as many as 50% of patients whose posterior branches were preserved. (3,5) Patients are less attentive of hypoesthesia of the infraauricular area than that of the earlobe; several patients in this series were unaware of infraauricular hypoesthesia until they had undergone tactile testing. Perhaps the reason for this can be explained by the greater degree of collateral nerve supply to the angle of the mandible from the lesser occipital nerve posteriorly and from the transverse cutaneous nerve of the neck; both of these nerves derive from the second and third cervical nerves, as does the great auricular nerve. In contrast, the sensory supply to the external ear is more diverse; the earlobe is innervated by the cervical nerves, the vagus nerve, and the mandibular branch of the trigeminal nerve. (5)
The result of preservation of the posterior branches of the great auricular nerve is that significantly fewer patients will experience hypoesthesia of the earlobe or infraauricular area. This can be achieved without increasing the risk of recurrence or significantly increasing the length of operating time. However, all patients who undergo parotidectomy with facial nerve dissection and preservation should be advised of the risk of numbness, even when the planned operation includes preservation of the posterior branches of the great auricular nerve.
With respect to the anterior branches of the great auricular nerve, it was not possible to perform any procedure in this series without sacrificing them.
References
(1.) Witt RL. The significance of the margin in parotid surgery for pleomorphic adenoma. Laryngoscope 2002; 112:2141-54.
(2.) Vieira MB, Maia AF, Ribeiro JC. Randomized prospective study of the validity of the great auricular nerve preservation in parotidectomy. Arch Otolaryngol Head Neck Surg 2002; 128:1191-5.
(3.) Brown AM, Wake MJ. Accidental full thickness bum of the ear lobe following division of the great auricular nerve at parotidectomy. Br J Oral Maxillofacial Surg 1990;28:178-9.
(4.) House JW. Facial nerve grading systems. Laryngoscope 1983;93: 1056-69.
(5.) Brown JS, Ord RA. Preserving the great auricular nerve in parotid surgery. Br J Oral Maxillofacial Surg 1989;27:459-66.
From the Section of Otolaryngology--Head and Neck Surgery, Department of Surgery, Christiana Care Health Systems, Wilmington, Del., and the Department of Otolaryngotogy, Jefferson Medical College, Philadelphia.
Reprint requests: Robert L. Witt, MD, 2401 Pennsylvania Ave., #112, Wilmington, DE 19806. Phone: (302) 888-1980; fax: (302) 888-1982; e-mail: RobertLWitt@aol.com
Originally presented as a poster during the Southern Section meeting of the Triological Society; Jan. 8-11, 2004; Marco Island, Fla.
COPYRIGHT 2005 Medquest Communications, LLC
COPYRIGHT 2005 Gale Group