A 35-year-old woman was referred for evaluation of a right facial mass that had slowly enlarged over the previous 4 years. Her condition was thought to represent an infectious process, and antibiotics were prescribed. However, the mass continued to grow, causing the patient great concern about her appearance (figure 1). She denied any facial weakness, pain, numbness, or decrease in saliva. Magnetic resonance imaging (MRI) demonstrated a solid, well-circumscribed, 2.3 x 2.3 x 2.3-cm mass anterior to the border of the right parotid gland (figure 2). Fine-needle aspiration biopsy of the mass established the diagnosis of pleomorphic adenoma.
[FIGURES 1-2 OMITTED]
The patient was not in favor of an external approach because of cosmetic concerns. She instead opted for a transoral approach, and the mass was successfully resected. Final pathology revealed a completely excised 2.8 x 1.6 x 1.5-cm pleomorphic adenoma of an accessory parotid gland with an intact capsule. Examination 9 months postoperatively showed a well-healed oral mucosa, excellent facial nerve function and cosmesis, and no evidence of recurrence.
According to cadaveric studies, accessory parotid glands are found in approximately 21% of the population. (1) These small structures are typically noted clinically only in a diseased state. Accessory parotid glands, once believed to be simple extensions of the main parotid gland, are small, flat structures that function completely independently of the main parotid gland. The accessory parotid gland is located approximately 6 mm anterior to the main parotid gland, between the skin and the masseter muscle along an imaginary line that extends from the tragus to a point midway between the ala of the nose and the vermilion border of the lip. (2,3)
Anatomically, the accessory and main parotid glands share two important characteristics. First, both glands drain into Stensen's duct through at least one minor tributary (at times two or three minor tributaries in the case of the accessory gland). (1) The more important similarity is their intimate relationship with the facial nerve. In the main parotid gland, the trunk of the nerve courses deep to the superficial body of the gland. In the accessory parotid gland, the zygomatic and buccal rami run superficial to the gland.
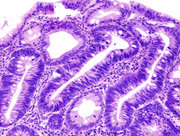
According to the literature, benign tumors of the accessory parotid gland account for approximately 50 to 74% of all accessory parotid neoplasms; the rate of malignancy ranges from 26 to 50%. (4) In the main parotid gland, the rate of malignancy is far lower--approximately 18.5%. (4) In 1993, Toh et al theorized that this variation between the two glands was secondary to the difference in their tissue composition. (5) On histologic examination, the accessory parotid gland is made up of both serous and mucinous cells such as those seen in the submandibular gland. In contrast, the main parotid gland is predominantly serous. Despite this difference in histology, the most common benign tumor in both the accessory and main parotid gland remains the pleomorphic adenoma, a slow-growing, well-encapsulated neoplasm.
References
(1.) Frommer J. The human accessory parotid gland: Its incidence, nature, and significance. Oral Surg Oral Med Oral Pathol 1977;43:671-6.
(2.) Batsakis JG. Accessory parotid gland. Ann Otol Rhinol Laryngol 1988;97 (4 Pt 1):434-5.
(3.) Lewkowicz A, Levy Y, Zeltser R, et al. Accessory parotid gland masses. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89:610-12.
(4.) Perzik SL, White IL. Surgical management of the preauricular tumors of the accessory parotid apparatus. Am J Surg 1966:112; 498-503.
(5.) Toh H, Kodama J, Fukuda J, et al. Incidence and histology of human accessory parotid glands. Anat Rec 1993;236:586-90.
From the Department of Otolaryngology, Charles R. Drew University of Medicine and Science (Dr. Osborne, Dr. purohit, and Dr. Hamilton), and the Head and Neck Cancer Center, Cedars-Sinai Medical Center (Dr. Osborne), Los Angeles.
COPYRIGHT 2005 Medquest Communications, LLC
COPYRIGHT 2005 Gale Group