Considerable progress has been made towards three key objectives in tropical infectious diseases in recent years: a clearer understanding of basic microbiology, pathogenesis, and host defence; expanded epidemiology; and new approaches to overall clinical management. However, problems have also emerged. Development of vaccines has been slow or non-existent, the efficacy of conventional treatment has fallen, HIV has affected the course of some diseases,[1] the cost of some new drugs has prohibited their use, and drug development for tropical diseases has fallen.[2] Inadequate vector control; poor nutrition, sanitation, and drinking water; civil war; and bare bones health budgets continue to present obstacles to preventing and controlling epidemics.[2 3]
This report highlights the current state of and recent advances made in diagnosis, treatment, and prevention in five tropical infections: African trypanosomiasis, leishmaniasis, lymphatic filariasis, malaria, and schistosomiasis. We have focused on these diseases because of their high level morbidity or mortality.[2] Although we have discussed only clinical management, experimental work in research laboratories continues to drive these clinical advances.[4]
Methods
This article is based on the hands-on clinical and laboratory research knowledge of the authors, who are experts in the diseases discussed. HWM wrote the section on leishmaniasis, JP the section on African trypanosomiasis, TBN the section on lymphatic filariasis, SLH the section on malaria, and AAFM the section on schistosomiasis. Personal knowledge was supplemented by review of relevant recent literature.
African trypanosomiasis
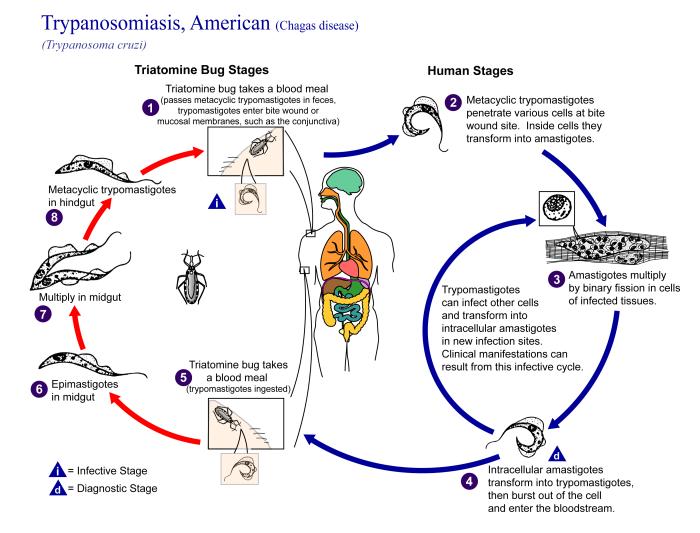
Tsetse flies (Glossina sp) transmit Trypanosoma brucei gambiense (in west and central Africa) and T b rhodesiense (in east and southern Africa). In Gambian infection, a long asymptomatic stage gives way to a subacute febrile illness followed by late stage chronic meningoencephalitis; the Rhodesian form progresses more rapidly. Although T b rhodesiense trypanosomiasis is currently quiescent, with several hundred cases reported annually, Gambian infection has surged in central Africa[5]: over 27 000 cases were reported in Congo in 1998 and epidemics in Angola, southern Sudan, and Uganda bring the current total for Africa to nearly 100 000 new infections a year. The relentless spread of disease in central Africa contrasts with the remarkable recent success of control programmes in South American trypanosomiasis (Chagas' disease).[6]
In early stage Gambian infection, daily pentamidine injections for seven days produce pronounced drug accumulation, modest cerebrospinal fluid penetration,[7] and a cure rate of 93%; a World Health Organisation trial is planned to compare three versus seven days of treatment. In "early-late stage" disease (cerebrospinal fluid white blood count 6-20/[mm.sup.3]), a 10 day pentamidine course has produced conflicting results; short course intravenous melarsoprol remains preferable in such patients. A new, more rational,[8] melarsoprol regimen (2.16 mg/kg/day for 10 days) is being tested; toxicity seems similar to that of previous regimens that included drug free intervals. Although more experience is needed, this 10 day regimen shortens hospital stay and reduces total dose and cost by one third.
In late stage Gambian trypanosomiasis, a 14 day regimen of intravenous eflornithine has been shown to be superior to seven days of treatment (97% v 86% cure).[9] Eflornithine fails more frequently in Uganda. For relapses, seven days' treatment with eflornithine is as effective as 14 days.[9] However, this drug is overpriced, and its future availability is unclear. Patients coinfected with HIV may respond less well to eflornithine.
Control of African trypanosomiasis relies on identifying and treating the largely asymptomatic human reservoir. Large scale use of the card agglutination test for trypanosomiasis, a serological assay which doubles case finding sensitivity, would improve disease control if such programmes could be sustained. Diagnostic advances such as the quantitative buffy coat technique[10] are little use in clinical practice. Clinical research priorities include improvement of existing drugs and evaluation of combination treatments. No vaccine is under development.
Leishmaniasis
Irrespective of geography or clinical form (cutaneous, mucosal, or visceral (kala-azar)), all leishmania infections, which are transmitted by phlebotomine sandflies, produce initial (and probably lifelong) parasitisation of tissue macrophages. Many cutaneous lesions self heal, and most visceral infections are actually subclinical, attesting to the power of T cell dependent, multi-cytokine induced macrophage activation. This same response may also cause inflammatory mucosal destruction. Despite initial immunological or pharmacological control, remote relapses of intracellular leishmanial infections are well recognised. Kala-azar also behaves like an opportunistic infection in immunosuppressed patients such as transplant recipients and those with advanced HIV disease. Most cases of HIV related kala-azar have so far been reported in southern Europe along the Mediterranean basin. Depletion of CD4 cells induced by HIV can alter any clinical aspect of kala-azar, including the response to treatment and propensity for relapse.[11]
Diagnosis in leishmaniasis depends on microscopic detection of amastigotes in smears of tissue aspirates or biopsy samples (fig 1). Sometimes the parasite can be cultured in microscopy negative samples. In American cutaneous infection, species identification may help to predict response to treatment and risk of developing mucosal disease. Parasite DNA can also be reliably detected in tissue aspirates and peripheral blood by polymerase chain reaction analysis. Immunochromatographic strip testing of blood from a finger prick for leishmanial (K39) antibody, which has been shown to be an accurate and rapid diagnostic method in India,[12] is now being tested elsewhere.
[Figure 1 ILLUSTRATION OMITTED]
Despite its toxicity and the need for prolonged treatment, pentavalent antimony remains first line treatment for all forms of leishmaniasis worldwide (table 1).[13] The important exception is kala-azar in India, which accounts for half of the world's cases. Resistance to antimony is now widespread in Bihar state (where 90% of Indian cases occur), and antimony should be abandoned in that region.
Table 1 Current and promising treatments in leishmaniasis and malaria(*)
(*) Details of treatment of African trypanosomiasis, lymphatic filariasis, and schistosomiasis, for which there are no promising new treatments, are available in a table on the BMJs website. Further details of updated treatment schedules are available at www.medletter.com.
([dagger]) Alternative treatments according to geographical region and aetiological species.
([double dagger]) P ovale and P malariae infections respond to choloroquine.
([sections]) All agents listed are given orally.
([paragraph]) Not yet licensed for this indication in the United States or many other countries.
(**) If P vivax or P ovale exposure is presumed, terminal prophylaxis with primaquine is recommended after screening for glucose 6-phosphate dehydrogenase activity.
Mucosal disease continues to be difficult to treat.[13] Preliminary work in Brazil, however, suggests that therapeutic vaccination with multiple recombinant leishmanial antigens may induce responses in drug refractory mucosal disease (S Reed, personal communication). If cutaneous infection requires treatment, parenteral antimony is most reliable; intralesional injections, topical paramomycin, and oral imidazoles have produced conflicting results.[13] Topical application of S-nitroso-N-acetylpenicillamine, a nitric oxide donor, is a new treatment based on the leishmanicidal effects of macrophage derived nitric oxide.[14] In kala-azar, highly active treatment regimens include conventional amphotericin B, injectible paramomycin (aminosidine), short courses (5-10 days) of a lipid formulation of amphotericin B, and oral miltefosine.[13 15] The cost of these new treatments will determine their usefulness worldwide.
Vaccine development is under way, and a killed promastigote plus BCG preparation is being tested in cutaneous leishmaniasis in Iran and Ecuador and in epidemic visceral infection in Sudan.[16]
Lymphatic filariasis
Up to 130 million people worldwide may be infected with one of the three lymph dwelling filariae, Wuchereria bancrofti, Brugia malayi, and B timori. In lymphatic filariasis, infective larvae are inoculated by mosquitoes; adult worms are found in lymph nodes or adjacent lymphatics, and offspring (microfilariae) circulate in the blood, often only at night.
The variable clinical manifestations of lymphatic filariasis include subclinical microfilaraemia or asymptomatic carriage of adult worms, acute adenolymphangitis, and lymphatic obstruction (for example, hydrocoele, or elephantiasis). The pathogenesis of adenolymphangitis and obstruction is complex and includes immune mediated inflammatory processes; secondary bacterial infection superimposed on lymphatic dysfunction is an important contributing factor.[17]
In brugian filariasis, diagnosis rests on microscopic detection of the parasite, most commonly the microfilariae. In bancroftian filariasis, detection of circulating antigen by enzyme linked immunosorbent assay (ELISA) or rapid immunochromatographic testing has replaced microscopy.[18] Filarial DNA can also be detected by polymerase chain reaction. Ultrasonography identifies adult worms in situ (commonly seen in scrotal lymphatics as the "filaria dance sign"[19]); lymphoscintigraphy helps to define the nature and extent of lymphatic damage or dysfunction.
Oral diethylcarbamazine kills both macrofilariae and microfilariae and remains the treatment of choice in all forms of lymphatic filariasis including subclinical infection. Repeated courses may be necessary. In subclinical infection, alternative treatments include diethvlcarbamazine plus oral albendazole or albendazole plus oral ivermectin. Tools to assess infection status (ultrasonography, circulating antigenaemia) are allowing more rational use of antifilarial drugs.[20] In adenolymphangitis, antipyretics and analgesics are recommended along with diethylcarbamazine; antibiotics are also useful if secondary infection is likely. For chronic manifestations of lymphatic filariasis, adjunctive regimens to diethylcarbamazine which emphasise hygiene and skin care, limb elevation, prophylactic antibiotics to reduce secondary bacterial infections, and physiotherapy have gained wide acceptance. Hydrocoeles can be drained repeatedly or managed surgically.
Programmes are being established to eliminate lymphatic filariasis worldwide.[21] These efforts will be similar to the integrated control programmes for onchocerciasis in Africa and the Americas, which are based on interrupting transmission. Long term microfilarial suppression is envisaged from the use of mass, annual distribution of single dose combinations of albendazole plus diethylcarbamazine or ivermectin; these regimens are known to suppress microfilariae for over a year. An added benefit of these regimens is their effect on gastrointestinal helminths.[22] Vaccine development is in its infancy.
Malaria
Plasmodium falciparum results in the death of more children each year than any other single infectious agent, and together with P vivax, P malariae, and P ovale, infects 300-500 million and kills 1-3 million people annually. Ninety percent of malaria cases and deaths are believed to occur in sub-Saharan Africa.[23] Fortunately, HIV coinfection has not materially altered the course of malaria.[1] Resistance of P falciparum to chloroquine, and more recently to pyrimethamine-sulfadoxine (Fansidar), is now widespread; however, out of necessity, both drugs are still often used as initial treatment in Africa. Mortality from severe infection in rural hospitals also remains substantial, and malaria looms as a potential health calamity in the tropics.[23] Nevertheless clinically useful advances in management have occurred.
Although diagnosis by microscopic examination of blood films remains standard, rapid immunochromatographic detection of circulating parasite antigen has entered clinical practice. These dipstick strip tests are specific, almost as sensitive as thick blood films, and simple to perform.[24] Polymerase chain reaction testing for plasmodium antigen is most sensitive but is a research tool.
Chloroquine resistant P vivax is now being encountered, and P falciparum continues to develop resistance to newly introduced drugs. The two most important groups of drugs for malaria treatment are still based on quinine or artemisinin (table 1). For uncomplicated malaria in Thailand caused by multi-drug resistant P falciparum, mefloquine combined with artesunate (an artemisinin derivative) provides sustained, high level efficacy. A separate combination, atovaquone plus prognanil (Malarone), is active against malaria around the world. In complicated severe malaria, parenteral administration of artemether and artesunate is as effective as intravenous quinine or quinidine, active against quinine resistant parasites, and often easier to use.[25]
Chemoprophylaxis may soon be advanced if Malarone, primaquine, or Tafenaquine (a new 8-aminoquinoline) become licensed for this indication. Malarone or primaquine are taken daily, but Tafenaquine will probably need to be taken only once a week. In contrast to current drugs which target the blood stage of infection (fig 2) these drugs act on the liver stage so will probably require just a few days of treatment after departure from a malarious area.[26]
[Figure 2 ILLUSTRATION OMITTED]
Insecticide impregnated bednets appreciably reduce mortality in children in Africa, and major efforts are under way to widely deploy them in endemic regions. Despite a firm immunological rationale (fig 2) and tremendous effort and promise, a licensed vaccine is not anticipated in the next five years.[27 28] Almost all vaccine trials have had to focus on only two of the estimated 6000 P falciparum proteins. Publication of the DNA sequence of chromosomes 2[29] and 3 of P falciparum has raised hopes that sequencing of the entire genome will lead to new, clinically useful directions in vaccine development as well as in diagnosis, treatment, and overall control of malaria. The WHO's new Roll Back Malaria campaign is aimed at expanding prevention and treatment to substantially reduce morbidity and mortality in the next five to 10 years.[30]
Schistosomiasis
Human infection with any of the five species of this trematode can cause serious disease in multiple organs.[31] Attempts to control infection and disease in many endemic areas have not been uniformly successful, partly because of pressure to develop land for agricultural use and irrigation schemes.
Recent advances in schistosomiasis have recognised both the parasite and the host immunopathological response in basic pathogenesis and its regulation. Susceptibility to infection maps to a region on chromosome 5q31-q33,[32] and hepatomegaly correlates with expression of specific class I and II histocompatibility antigens. Development of liver fibrosis maps to chromosome 6q22-q23; this region is linked to the gene encoding the receptor for the antifibrogenic cytokine, interferon-gamma.[33]
Accurate and non-invasive ultrasonography has advanced clinical assessment and gives quantifiable and specific information on liver fibrosis, associated portal hypertension and oesophageal varices, and urinary tract disease (Schistosoma haematobium).[34] HIV coinfection has not adversely affected the clinical or therapeutic response in schistosomiasis; dually infected individuals may actually pass fewer eggs.[1]
Progress has been achieved in serological testing for diagnosis and assessment of disease activity. Available tests for antibody detection are highly sensitive and specific.[35] Tests for schistosome antigen in serum or urine are also available and offer the added advantage of close correlation with intensity of infection and disease activity.
Current chemotherapy is much safer and more effective than previous treatments. Praziquantel, a single dose oral drug used in both acute and established infection, reduces egg counts by over 95% and produces parasitological cure in about 85%. Oxamniquine and metrifonate are alternative oral drugs. Praziquantel is now recommended for every infected individual and in selective population, chemotherapy based, control programmes. The use of one drug on a massive scale, however, may lead to resistance. One challenge for the near future, therefore, is to find additional antischistosomal drugs. Candidate vaccine antigens have been tested in experimental animals; none is ready for human studies.
We thank Dr Shyam Sundar of Banaras Hindu University, Varanasi, India for the aspirate smear from a patient with kala-azar.
Funding: Supported by NIH grant AI 16963 (to HWM).
Competing interests. None declared.
Recent advances
In Central Africa, Gambian sleeping sickness has surged dramatically
New drug development in African trypanosomiasis is impossible for commercial reasons; priority should be given to improving the use of old drugs
Vaccine testing is under way in cutaneous and visceral leishmaniasis, and short-course parenteral and oral treatment alternatives to pentavalent antimony are now available
Widespread annual distribution of single-dose combinations of albendazole plus either diethylcarbamazine or ivermectin may largely eliminate lymphatic filariasis
Ultrasonography, circulating filarial antigen detection, and lymphoscintigraphy have refined clinical definitions and approach to treatment in lymphatic filariasis
Despite major obstacles and no vaccine, recent clinical progress in diagnosis, treatment, chemoprophylaxis and control provides guarded optimism in malaria
Host genetics determine susceptibility to schistosome infection, organ dysfunction, and disease
Useful websites
WHO special programme for research and training in tropical diseases (www.who.int/tdr/)
WHO division of control of tropical diseases (www.who.int/ctd/)
Malaria Foundation (www. malaria.org/)
[1] Karp CI, Neva FA. Tropical infectious diseases in human immuno-deficiency virus-infected patients. Clin Infect Dis 1999;28:947-65.
[2] Trouiller PT, Olliaro PL. Drug development output from 1975 to 19913: what proportion tot tropical diseases? Int. J Infect Dis 1999;3:61-3.
[3] Gilles HM, Lucas AO. Tropical medicine: 100 years of progress. Br Med Bull 1998;54:269-80.
[4] Weatherall D. The future role of molecular and cell biology in medical practice in the tropical countries. Br Med Bull 1998;34:489-501.
[5] Ekwanzala M, Pepin J, Khonde N, Molisho S, Bruneel H, De Wals P. In the heart of darkness: sleeping sickness in Zaire. Lancet 1996;3-48:1427-30.
[6] Schofield CJ, Dias JC The southern cone initiative against Chagas' disease. A&, Parasitol 1999;42: 1-27.
[7] Bronner U, Doua I, Ericsson O, Gustafsson, Miezan TW, Rais M, et al. Pentamidine concentrations in plasma, whole blood and cerebrospinal fluid during treatment of Trypanosoma gambiense infection in Cote d'Ivoire. Trans R Soc Trop Med Hyg 1991;85:608-11.
[8] Burri C, Baltz C. Giroud C, Doua F, Welker HA, Brun R. Pharmacokinetic properties of the trypanocidal drug melarsoprol. Chemotherapy 1993;39:225-34.
[9] Pepin J, Khonde N, Maiso F, Doua F, Jaffar S, Ngampo S, et al. Short-course eflornitine in Gambian sleeping sickness: a multicentre randomised controlled trial. Bull World Health Org (in press).
[10] Bailey JW, Smith DH. The quantitative buffy coat for the diagnosis of trypanosomes. Tropical Doctor 1994;24:54-6.
[11] Alvar J, Canavate C, Gutierrez-Solar B, Jiminez M, Laguna F, Lopez-Velez R, et al. Leishmania and human immunodeficiency virus coinfection: the first 10 years. Clin Microbiol Rev 1997;10:298-319.
[12] Sundar S, Reed SG, Singh VP, Kumar PCK, Murray HW. Rapid accurate field diagnosis of Indian visceral leishmaniasis. Lancet 1998;351:563-5.
[13] Herwaldt BL. Leishmaniasis. Lancet 1999;354:1191.
[14] Lopez-Jaramillo P, Ruano C, Rivera J, Teran E, Salazar-Irigoyen R, Esplugues JV, et al. Treatment of cutaneous leishmaniasis with nitric-oxide donor. Lancet 1998;351:1176-7.
[15] Sundar S, Gupta LB, Makaria MK, Singh MK, Voss A, Rosenkaimer F, et al. Oral treatment of visceral leishmaniasis with miltefosine. Ann Trop Med Parasitol 1999;93:589-97.
[16] Sharifi I, FeKri AR, Aflatonian M-R, Khamesipour A, Nadim A, Mousavi M-RA, et al. Randomised vaccine trial of single dose of killed Leishmania major plus BCG against anthroponotic cutaneous leishmaniasis in Barn, Iran. Lancet 1998;351:1540-3.
[17] Dreyer G, Medeiros Z, Netto MJ, Leal NC, de Castro LG, Piessens WF. Acute attacks in the extremities of persons living in an area endemic for bancroftian filariasis: differentiation of two syndromes. Trans R Soc Trop Med Hyg 1999;93:413-7.
[18] McCarthy JS. Diagnosis of lymphatic filariasis. In: Nutman TB, ed. Lymphatic filariasis. London: Imperial College Press, 1999:127-49.
[19] Noroes J, Addiss D, Amaral F, Coutinho A, Medeiros Z, Dreyer G. Occurrence of living adult Wuchereria bancrofti in the scrotal area of men with microfilaraemia. Trans R Soc Trop Med Hyg 1996;90:55-6.
[20] Addiss, DA, Dreyer G. Treatment of lymphatic filariasis. In: Nutman TB, ed. Lymphatic filariasis. London: Imperial College Press, 1999:151-99.
[21] Ottesen EA, Duke BOL, Karam M, Behbehani K. Strategies and tools for the control elimination of lymphatic filariasis. Bull WHO 1997;75:491-503.
[22] Ottesen EA, Ismail MM, Horton J. The role of albendazole in programmes to eliminate lymphatic filariasis. Parasitol Today 1999;15:382-6.
[23] White NJ, Nosten F, Looareesuwan S, Watkins WM, Marsh K, Snow RW, et al. Averting a malaria disaster. Lancet 1999;353:1965-7.
[24] Beadle C, Long W, Weiss W, McElroy P, Maret S, Oloo A, et al. Diagnosis of malaria by detection of Plasmodium falciparum HRP-2 antigen with a rapid dipstick antigen-capture assay. Lancet 1994;343:564-8.
[25] Hoffman SL. Artemether in severe malaria: still too many deaths. N Engl J Med 1996;335:124-6.
[26] Baird JK, Hoffman SL. Prevention of malaria in travelers. Med Clin N Amer 1999;83:923-44.
[27] Stoute JA, Saaoui M, Heppner DG, Momin P, Kester KE, Desmons P, et al. A preliminary evaluation of a recombinant circumsporozoite protein vaccine against Plasmodium falciparum malaria. N Engl J Med 1997;336:86-91.
[28] Miller LH, Hoffman SL. Research toward vaccines against malaria. Nature Med 1998;4:520-4.
[29] Gardner MJ, Tetteli H, Carucci DJ, Cummings LM, Adams MD, Smith HO, et al. Chromosome 2 sequence of the human malaria parasite Plasmodium falciparum. Science 1998;282:1126-32.
[30] Nabarro DN, Tayler EM. The "roll back malaria" campaign. Science 1998;280:2067-8.
[31] Mahmoud AAF. Schistosomiasis from the bench to the field. In: Mahmoud AAF, ed. Tropical medicine: science and practice. London: Imperial College Press (in press).
[32] Marquet S, Abel L, Hillaire D, Dessein H, Kalil J, Feingold J, et al. Genetic localization of a locus controlling the intensity of infection in Schistosoma mansoni on chromosome 5q31-q33. Nat Genet 1996;14: 181-4.
[33] Dessein AJ, Hillaire D, Eldin N, Elwali A, Marquet S, Mohamed-Ali Q, et al. Severe hepatic fibrosis in Schistosoma mansoni infection is controlled by a major locus that is closely linked to the interferon-gamma receptor gene. Am J Hum Genet 1999;65:709-21.
[34] Dochring-Schwerdtfeger E, Kardorff R. Ultrasonography in schistosomiasis in Africa. Mem Inst Oswaldo Cruz 1995;90:141-5.
[35] Tsang VCW, Wilkins PP. Immunodiagnosis of schistosomiasis. Immunol Invest 1997;26:175-88.
Department of Medicine, Weill Medical College of Cornell University, New York, NY 10021, USA
Henry W Murray professor
Centre for International Health, University of Sherbrooke, Sherbrooke, Quebec J1H 5N4, Canada
Jacques Pepin associate professor of medicine
Helminth Immunology Section and Clinical Parasitology Unit, Laboratory of Parasitic Diseases, National Institutes of Health, Bethesda, MD 20892, USA
Thomas B Nutman head
Naval Medical Research Center, Rockville, MD 20852, USA Stephen L Hoffman director, malaria programme
Merck Vaccines, Whitehouse Station, NJ 08889, USA Adel A F Mahmoud president
Correspondence to: H W Murray hwmurray@mail.med.cornell.edu
BMJ 2000;320:490-4
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2000 Gale Group