EVIDENCE-BASED ANSWER For patients whose echocardiograms show advanced calcification of the aortic valves, a jet velocity of > 4.0 m/s, or a progression in jet velocity of 0.3m/s/year; and for patients who have an abnormal exercise response or an impaired functional status, consider referral for valve replacement prior to the onset of symptoms (Grade of Recommendation: C).
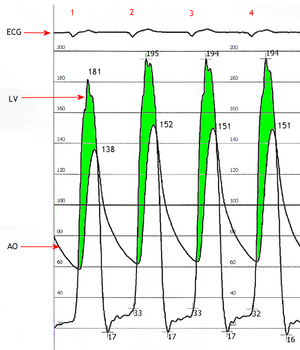
EVIDENCE SUMMARY Aortic stenosis is a narrowing of the aortic valve. Degree of severity is judged by vane area: mild (1.5-2.0 [cm.sup.2]), moderate (1.0-1.5 [cm.sup.2]), severe (< 1.0 [cm.sup.2]). Alternatively, stenosis may be classified by transvalvular gradient or jet velocity, the latter being the easier quantity to measure by echocardiogram. Prevalence of aortic stenosis increases with age; one series of 1243 elderly women (mean age of 82) found mild stenosis in 10%, moderate stenosis in 6%, and severe stenosis in 2%. (1) Natural history studies show that once classic symptoms develop, average survival decreases to 5 years with the onset of angina, 3 years after cardiac syncope, and 2 years after heart failure. (2) The incidence of sudden death increases from < 1% annually among asymptomatic patients to 15% to 20% among symptomatic patients. (3,4)
Aortic stenosis is suggested by such findings as a harsh systolic murmur at the right upper sternal border, pulsus parvus et tardus, and a sustained point of maximal impulse. Exercise stress testing may provide additional information. In one prospective study of 123 patients, those who had a greater increase in valve area, cardiac output, and blood pressure and a smaller decrease in stroke volume on stress echocardiogram were more likely to remain asymptomatic for the entire length of their time in the study, an average of 2.5 year. (5)
Asymptomatic patients with aortic stenosis who undergo coronary artery bypass grafting (CABG) often have their aortic valve replaced at the same time; the timing of aortic valve replacement in patients nor requiring CABG is controversial. One prospective study found the severity of stenosis at baseline to be the strongest prognostic predictor. Patients with a jet velocity, of < 3.0 m/s were unlikely to develop symptoms within 5 years; those with a jet velocity of [greater than or equal to] 4.0 m/s had a > 50% likelihood of developing symptoms or dying within 2 years. (5) Another study followed 128 patients for 4 years and found that moderate to severe valvular calcification and an increase in jet velocity of [greater than or equal to] 0.3 m/s/year were the best prognostic predictors. (6) Almost 80% of those with both calcification and a rapid change in jet velocity underwent surgery or died within 2 years (6) (Table).
RECOMMENDATIONS FROM OTHERS The American College of Cardiology/American Heart Association Task Force on Practice Guidelines recommends echocardiograms every 5 years for mild stenosis, every 2 years for moderate stenosis, and annually for severe stenosis. (4) There is no guideline for exercise testing. Aortic valve replacement is recommended for symptomatic patients and patients with severe stenosis undergoing CABG or other valvular or aortic surgery.
REFERENCES
(1.) Aronow WS, Ahn C, Kronzon I. Am J Cardiol 1997; 79:379-80.
(2.) Ross J Jr., Braunwald E., Circulation 1968; 38(1 Suppl):61-7.
(3.) Balentine J, Eisenhart A. Aortic Stenosis EMedicine Journal 2002; 3:1.
(4.) Bonow RO, Carabello B, deLeon AC Jr., et al. Circulation 1998; 98:1949-84.
(5.) Otto CM, Burwash IG, Legget ME, et al Circulation 1997; 93:2262-70
(6.) Rosenhek R, Binder T. Porenta G, et al. N Engl J Med 2000; 343:611-7
Members of the Family Practice Inquiries Network answer clinical questions with the best available evidence in a concise, reader-friendly format. Each peer-reviewed answer is based on a standard search of resources, including MEDLINE, the Cochrane Library, and InfoRetriever, and is graded for level of evidence (http://cebm.jr2.ox.ac.uk/docs/levels.html). The collected Clinical Inquiries can be found at http://www.jfponline.com and http://www.fpin.org; the latter site also includes the search strategy used for each answer.
Clinical Commentary by Ken Grauer, MD; and search strategy, at www.fpin.org.
COPYRIGHT 2002 Dowden Health Media, Inc.
COPYRIGHT 2002 Gale Group