Asthma accounts for nearly 500,000 hospitalizations, 2 million emergency department visits, and 5,000 deaths in the United States each year. (1) Despite an increased understanding of pathophysiology and treatment options, the disease remains undertreated. Asthma guidelines have been established to address the disparity between scientific knowledge and actual management, and these guidelines have been updated recently to answer several key clinical questions. Part I of this two-part article reviews the updated guidelines, examines the supporting evidence behind the changes, and discusses the clinical implications of diagnosing and treating asthma in children and adults. Part II (2) will discuss the medical management of asthma.
The Updated Guidelines
The National Asthma Education and Prevention Program (NAEPP) Expert Panel, organized by the National Institutes of Health's National Heart, Lung, and Blood Institute, was convened in 1989 to improve asthma care in the United States. The panel published its first set of asthma guidelines in 1991; six years later it released a second set of guidelines. (3)
Clinical guidelines are most valuable if they are based on the most current research. This is especially important for asthma, given some of the recently available medications and the vast number of studies published in recent years. The NAEPP decided that an efficient approach would be to update the guidelines on a periodic basis, and to focus on key clinical questions rather than rewrite the entire guideline. These position statements will be published as NAEPP Expert Report Updates. The most recent update (4) was published in 2002, and future updates will be incorporated into a Web-based version of the existing guidelines (http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm).
Diagnosis and Classification
Aspects of asthma management that remain unchanged in the updated guidelines are the diagnosis of asthma and the use of a classification system to determine severity of the disease. Unlike diseases in which objective numeric values are used to establish a diagnosis (e.g., hypertension, diabetes), asthma is a clinical diagnosis that incorporates genetic predisposition and clinical symptoms with objective measures of lung function (Table 1). (3)
Before making the diagnosis of asthma, physicians should determine whether other conditions could be causing a patient's symptoms (Table 2). (3) Spirometry, not just the use of peak expiratory flow (PEF) meters, is critical for diagnosing and managing asthma. The NAEPP recommends the use of spirometry for initial assessment, evaluation of response to treatment, and assessment of airway function at least every one to two years. (3) However, physicians should note that patients with asthma can have normal lung function.
Disease severity is determined by pulmonary function measurements, asthma symptoms, and the need for rescue medication (Table 3). (3) Several factors can complicate the assessment of asthma severity. First, disease classification is based on the symptoms the patient had before starting treatment. Once treatment has begun, classification becomes more difficult. Second, asthma is a variable disease. Studies have shown that patients with asthma rarely remain in the same category over time, (5) and that patients themselves often underestimate their symptoms and thus are classified incorrectly. (6) Furthermore, the current classification system does not take activity level into consideration. One study (7) found that asthma initially classified as mild was much more severe when patients' activity levels were considered. When activity level was included in the classification system, 93 percent of the patients had persistent asthma, and 77 percent had moderate to severe asthma. (7)
Finally, objective measures of pulmonary function, such as PEF and forced expiratory volume in one second (FE[V.sub.1]), do not always correlate with the severity or frequency of asthma symptoms.8 For example, one study9 found that although a decrease in FE[V.sub.1] was predictive of an asthma attack in the following year, more than 25 percent of study participants with normal lung function had a subsequent asthma attack.
The previous NAEPP guidelines noted that underdiagnosis and inappropriate therapy contribute substantially to asthma morbidity and mortality. (3) Despite the recent updates to the guidelines, the diagnosis of asthma and classification of its severity (an essential consideration in selecting asthma medications) remain challenging.
Monitoring
The updated guidelines address two key clinical questions about the monitoring of patients with asthma: whether written asthma action plans improve outcomes compared with medical management alone, and whether written action plans based on PEF monitoring improve outcomes more than plans based on symptoms. However, the data to support the use of action plans with and without PEF monitoring were inconclusive.
Written action plans and PEF monitoring have been considered essential components of asthma self-management education. (10) Written action plans tell patients how to adjust medications and control their environment to manage their asthma on normal days and during attacks, and encourage them to seek care before an attack begins. PEF monitoring often is included in these plans, and numeric values serve as indicators that patients should take certain actions.
Busy physicians, however, often use written asthma plans independent of specific asthma education, such as videos and handouts. For this reason, the NAEPP panel (4) reviewed several studies of medical management with or without written action plans. All of these studies had significant limitations: most included limited or no asthma education, only one included children, and many lacked power to show significant differences between study groups.
A Cochrane review (11) of 25 studies of asthma educational interventions found that patients who self-managed their asthma with written action plans derived significant benefit compared with patients who did not, as measured by decreased emergency department visits, fewer hospitalizations, and improved lung function. In addition, the results of a well-conducted study, (10) which was mentioned in the updated guidelines but not included in the Cochrane review because it was not randomized, showed that written action plans were associated with a 70 percent reduction in mortality in asthmatic patients acutely presenting to a hospital.
PEF monitoring has been considered adjunctive to a written action plan because it was thought that objective measures would help patients make decisions about managing their asthma. However, the addition of PEF monitoring to written action plans provided no clear evidence of benefit. Few studies of the use of PEF meters were available for review, and these studies had limitations similar to those in the studies of written action plans. Despite lack of evidence for the use of PEF monitoring, factors such as a patient's inability to recognize signs of worsening asthma may indicate that such monitoring is necessary.
Although evidence for written action plans and PEF monitoring is inconclusive, the NAEPP panel continues to recommend written action plans as part of an overall effort to educate patients in self-management of asthma. It also recommends consideration of PEF monitoring in patients with moderate or severe persistent asthma. These management techniques have few risks and low costs, and they may improve communication between the patient and physician.
Prevention of Disease Progression
The NAEPP panel also studied the effects of early treatment on the progression of asthma, specifically whether earlier intervention with long-term therapy (i.e., inhaled corticosteroids) prevented disease progression in patients with mild or moderate persistent asthma. The findings were inconclusive but intriguing.
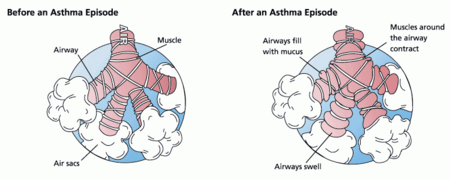
Airway remodeling has a significant role in the pathogenesis of asthma. (12) The prolonged inflammation that asthma triggers in the small airways can lead to structural changes in the airway wall that may cause additional airflow limitation (Table 4). This remodeling has been found even in patients with mild asthma. (13) Although asthma generally is a reversible disease, these changes in the airways are permanent.
It has been proposed that if airway remodeling could be halted in the early stages of asthma by reducing inflammation, inhaled corticosteroids might have disease-modifying properties in addition to their known clinical benefits. The NAEPP panel reviewed four studies (14-17) examining the effects of the use of inhaled corticosteroids soon after the diagnosis of asthma. All four studies found that corticosteroid use improved lung function in patients with asthma, and that a delay in the initiation of therapy was associated with decreased benefit. However, the panel found several methodologic flaws with each of the studies, including a lack of statistical significance testing, (15) a high dropout rate, (16) a high proportion of smokers compared with nonsmokers, (17) and a lack of statistical significance between groups. (14) Therefore, no conclusion could be made about the effect of inhaled corticosteroids on disease modification.
The panel also reviewed the Childhood Asthma Management Program (CAMP) study, (18) a large, prospective trial of more than 1,000 children with mild asthma. The CAMP study, which compared the inhaled corticosteroid budesonide, the mast-cell stabilizer nedocromil, and placebo, found that patients who received budesonide had improved outcomes compared with the other groups. The study also firmly established the safety of inhaled corticosteroid use in children. However, there was no evidence of a progressive decline in lung function in children with asthma, whether they received active treatment or not. Nor was there evidence that corticosteroid use prevented the worsening of asthma. When treatment was discontinued, symptoms and airway hyperresponsiveness returned. The CAMP study proved that inhaled corticosteroids are safe in children and provide excellent control of asthma, but the study was unable to prove that they modify the underlying disease.
There are several explanations for the failure of the CAMP study (18) to demonstrate a change in asthma progression. First, the study may not have lasted long enough. Also, changes in the children's lungs may have occurred before randomization. In fact, there is evidence that if asthma symptoms begin before the age of three years, lung function progressively declines later in life, but that this decline does not occur in children whose symptoms begin after the age of three years. (19) Evidence also shows a progressive decline in lung function in asthmatic adults. (20,21)
As a result of the CAMP study, (18) the NAEPP panel concluded that evidence is insufficient to support the assumption that early intervention with asthma therapy prevents a progressive decline in lung function. However, the efficacy and safety of inhaled corticosteroids, particularly in children, cannot be overstated. Early use of inhaled corticosteroids is recommended in all patients with persistent asthma and is also recommended in infants and children in whom the diagnosis of asthma is suspected.
The author indicates that he does not have any conflicts of interest. Dr. Mintz is a member of the advisory board for GlaxoSmithKline and the speaker's bureaus for GlaxoSmithKline, Aventis Pharmaceuticals Inc., and AstraZeneca Pharmaceuticals LP.
REFERENCES
(1.) Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma--1980-1999. MMWR Surveill Summ 2002;51:1-13.
(2.) Mintz M. Asthma update: Part II. Medical management. Am Fam Physician 2004. In press.
(3.) National Asthma Education and Prevention Program. Guidelines for the diagnosis and management of asthma: expert panel report 2. Bethesda, Md.: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute, 1997; NIH publication no. 97-4051.
(4.) National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma update on selected topics--2002. Bethesda, Md.: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute, 2003; NIH publication no. 02-5074.
(5.) Calhoun WJ, Sutton LB, Emmett A, Dorinsky PM. Asthma variability in patients previously treated with [beta]-agonists alone. J Allergy Clin Immunol 2003;112: 1088-94.
(6.) Asthma in America. Asthma statistics. Accessed online June 3, 2004, at: http://www.asthmainamerica.com/statistics.htm.
(7.) Fuhlbrigge AL, Adams RJ, Guilbert TW, Grant E, Lozano P, Janson SL, et al. The burden of asthma in the United States: level and distribution are dependent on interpretation of the National Asthma Education and Prevention Program guidelines. Am J Respir Crit Care Med 2002;166:1044-9.
(8.) Management of chronic asthma. Rockville, Md.: Agency for Healthcare Research and Quality; File inventory, Evidence report/technology assessment no. 44; AHRQ publication no. 01-E044, September 2001. Accessed online June 3, 2004, at: http://www.ahcpr.gov/clinic/astmainv.htm.
(9.) Fuhlbrigge AL, Kitch BT, Paltiel AD, Kuntz KM, Neumann PJ, Dockery DW, et al. FEV1 is associated with risk of asthma attacks in a pediatric population. J Allergy Clin Immunol 2001;107:61-7.
(10.) Abramson MJ, Bailey MJ, Couper FJ, Driver JS, Drummer OH, Forbes AB, et al. Are asthma medications and management related to deaths from asthma? Am J Respir Crit Care Med 2001;163:12-8.
(11.) Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, Haywood P, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2004;(1):CD001117.
(12.) Elias JA, Zhu Z, Chupp G, Homer RJ. Airway remodeling in asthma. J Clin Invest 1999;104:1001-6.
(13.) Chetta A, Foresi A, Del Donno M, Bertorelli G, Pesci A, Olivieri D. Airways remodeling is a distinctive feature of asthma and is related to severity of disease. Chest 1997;111:852-7.
(14.) Agertoft L, Pedersen S. Effects of long-term treatment with an inhaled corticosteroid on growth and pulmonary function in asthmatic children. Respir Med 1994;88:373-81.
(15.) Haahtela T, Jarvinen M, Kava T, Kiviranta K, Koskinen S, Lehtonen K, et al. Effects of reducing or discontinuing inhaled budesonide in patients with mild asthma. N Engl J Med 1994;331:700-5.
(16.) Overbeck SE, Kerstjens HA, Bogaard JM, Mulder PG, Postma DS. Is delayed introduction of inhaled corticosteroids harmful in patients with obstructive airways disease (asthma and COPD)? The Dutch Chronic Nonspecific Lung Disease Study Group. Chest 1996;110:35-41.
(17.) Selroos O, Pietinalho A, Lofroos AB, Riska H. Effect of early vs late intervention with inhaled corticosteroids in asthma. Chest 1995;108:1228-34.
(18.) Long-term effects of budesonide or nedocromil in children with asthma. The Childhood Asthma Management Program Research Group. N Engl J Med 2000;343:1054-63.
(19.) Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med 1995;332:133-8.
(20.) Peat JK, Woolcock AJ, Cullen K. Rate of decline of lung function in subjects with asthma. Eur J Respir Dis 1987;70:171-9.
(21.) Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med 1998;339:1194-200.
MATTHEW MINTZ, M.D., is associate professor of medicine and director of the primary care clerkship at The George Washington University School of Medicine and Health Sciences, Washington, D.C., where he also received his medical degree and completed residency training in primary care and internal medicine.
Address correspondence to Matthew Mintz, M.D., ACC 2-105B, 2150 Pennsylvania Ave. NW, Washington, DC 20037 (e-mail: mmintz@mfa.gwu.edu). Reprints are not available from the author.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group