Objective: Surgical indication was determined by lung biopsy in 91 patients with secundum atrial septal defect (ASD) and severe pulmonary hypertension > 70 mm Hg of pulmonary arterial peak pressure and/or pulmonary vascular resistance of > 8 U/[m.sup.2].
Methods and results: Pulmonary vascular disease (PVD) in ASD was classified into four types: (1) Muscuioelastosis consisting of longitudinal muscle bundles and elastic fibers; surgery is indicated no matter how severely the peripheral small pulmonary arteries are occluded. Surgery was performed in all of the 20 patients, and the postoperative course was uneventful. (2) Plexogenie pulmonary arteriopathy: surgery is indicated for a PVD index [less than or equal to] 2.3. Surgery was performed in 25 of the 32 patients. The remaining seven patients for whom surgery was not indicated are under follow-up observation. No deaths have occurred among the 32 patients. (3) Thromboembolism of small pulmonary arteries: Surgery is indicated for all such cases. Surgery was indicated in all of the five patients. (4) Mixed type of plexogenic pulmonary arteriopathy and musculoelastosis: Surgery is indicated if the collateral is not observed. Surgery was performed in 15 of the 25 patients. The remaining 10 patients for whom surgery was not indicated are under follow-up observation. Nine of these 91 patients associated with primary pulmonary hypertension were eliminated from this study.
Conclusion: No deaths due to PVD occurred among the 82 patients who underwent lung biopsy diagnosis. Lung biopsy diagnosis is concluded to be very effective.
(CHEST 2004; 126:1042-1047)
Key words: atrial septal defect; lung biopsy diagnosis; pulmonary hypertension; pulmonary, vascular disease
Abbreviations: ASD = secundum atrial septal defect; IPVD = index of pulmonary/vascular disease PVD = pulmonary vascular disease: PVR = pulmonary, vascular resistance
**********
In a previous study, (1) we reported the indications for surgery in patients with secundum atrial septal defect (ASD) and severe pulmonary hypertension on the basis of lung biopsy diagnosis. Subsequently, operative indications were mainly determined by the criteria reported in that study. However, in some patients in whom lung biopsy was performed during surgery, operative indications were expanded because of successful surgery and uneventful late postoperative course. In this article, new operative indications, the surgical results, and late postoperative results are presented on the basis of lung biopsy diagnosis in 91 patients. Characteristic patients who showed the most severe pathologic findings and survived after surgery or without surgery are also introduced fur four types of pulmonary vascular disease (PVD).
MATERIALS AND METHODS
Lung biopsy specimens of 91 patients with ASD and severe pulmonary hypertension that were sent to the senior author from 32 hospitals in Japan for consultation between 1981 and 2000 were used as materials. Lung biopsy was performed when surgical indications were not determined by cardiac catheterization alone, that is, the patients had a pulmonary arterial peak pressure of > 70 mm Hg and/or pulmonary vascular resistance (PVR) of > 8 U/[m.sup.2]. They ranged in age from 45 days to 71 years with a mean of 29 years. In 9 of the 91 patients, lung biopsy was performed during surgery. Lung tissue was obtained mainly from the right median lobe and was fixed in 10% formalin. Thirty semiserial histologic sections were obtained from each case at intervals of 50 [micro]m and were stained with Elastica-Goldner stain. (2) Nine of these 91 patients with abnormally thickened media of the small pulmonary arteries received a diagnosis of primary pulmonary hypertension and were eliminated from this study. (3) In our previous study, (4) PVD in ASD was classified into four types: musculoelastosis (intimal proliferatioil of longitudinal muscle bundles and elastic fibers), plexogenic arteriopathy, thromboembolism of the small pulmonary arteries, and mixed-type lesions consisting of plexogenic arteriopathy and musculoelastosis or thromboembolism of the small pulmonary arteries. Criteria for operative indications were determined for each group. In this study, criteria for operative indications were reconsidered and expanded to take into account the patients who survived after surgery and had more severe PVD than that previously reported.
Lung biopsy diagnosis clinically consists of the following five grades (A-E grading) (5): A, no operative or hospital death, and cure of pulmonary hypertension; B, no operative or hospital death; remission of pulmonary hypertension; C, no operative or hospital death, but slight possibility of late death; D, no operative death, but strong possibility of hospital death or late death; and E, operative or hospital death. Patients with grades A, B, and C are operable, but D and E are not.
RESULTS
Musculoelastosis
In our previous article, (1) in cases of musculoelastosis, intimal proliferation of longitudinal muscle bundles, and elastic fibers, surgery was indicated when the vascular lumina of the small pulmonary arteries and arterioles are not completely occluded. However, the following case necessitated the expansion of operative indications.
Patient 1, a 41-Year-Old Woman: Cardiac catheterization performed at the age of 21 years contradicted ASD closure because of severe pulmonary hypertension. In 1988, when the patient was 41 years old, she was hospitalized due to respiratory infection. Even after recovery, cyanosis of the lips and fingernails and orthopnea due to respiratory distress were observed. Cardiac catheterization showed severe pulmonary hypertension suggesting inoperability (Table 1). Since she strongly desired surgical treatment, ASD closure and lung biopsy were performed. The postoperative course was unexpectedly uneventful. At postoperative year 10, she is enjoying her life without cyanosis and shortness of breath. The postoperative results of cardiac catheterization at 1 month and 1 year are shown in Table 1.
Lung biopsy findings showed medial hypertrophy and complete occlusion of almost all of the small pulmonary arteries in the biopsied lung tissue < 100 [micro]m in diameter dim to musculoelastosis. The even smaller peripheral pulmonary arteries showed not only complete occlusion of the lumen but also destruction and fibrosis of the media due to necrosis of the smooth muscle cells (Fig 1, top). A characteristic finding was extensive networks of capillaries that proliferated around the small pulmonary arteries just proximal to the completely occluded lumena (Fig 1, bottom). It was suggested that pulmonary blood flowed directly from the patent small pulmonary arteries to the capillaries. Successful surgery was performed for another 38-year-old female patient in whom all of the small pulmonary arteries in the biopsy specimen seemed to be occluded by longitudinal smooth-muscle cells encircled by many capillaries. She is doing well 5 years after surgery. Therefore, we concluded that in isolated musculoelastosis, no matter how severely the peripheral small pulmonary arteries are occluded, ASD closure is worthwhile. We thus revised the criteria for surgical indications to indicate that patients with isolated musculoelastosis are operable in ASD.
[FIGURE 1 OMITTED]
A new A-E grading is defined as follows by the above-mentioned evidence in musculoelastosis: A, the lumina of small pulmonary arteries are not completely obstructed by musculoelastosis; B, less than half of the lumina are obstructed; and C, more than half of the lumina of peripheral small pulmonary arteries are completely obstructed by musculoelastosis, even if all of the peripheral small arteries are obstructed with extensive net work of capillaries just proximal to the occluded lumina. There are no patients with grades D or E in this type of PVD.
In this series, isolated musculoelastosis was seen in 20 patients. Grades A, B, and C were seen in four, seven, and nine patients, respectively. There were no patients with grades D or E. Surgery was performed in all of the 20 patients, and the postoperative course was uneventful. There have been no operative deaths or late deaths to date.
Plexogenic Arteriopathy
In plexogenic pulmonary arteriopathy, the criterion for operative indication was based on an index of PVD (IPVD). (6) In our previous study, the IPVD of [less than or equal to] 2.2 was indicated for ASD closure. (1) However, successful ASD closure was performed for two patients whose IPVD was 2.3. Therefore, we revised so that an IPVD of [less than or equal to] 2.3 indicates surgical operation. Here we introduce a patient with plexogenie arteriopathy in whom a new type of pulmonary circulation was completed.
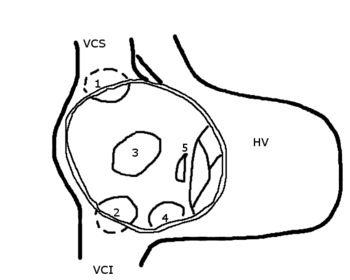
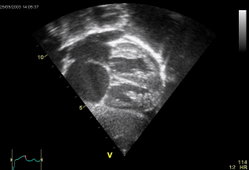
Patient 2, a 38-Year-Old Woman: The patient complained of shortness of breath with exertion commencing 3 years previously. She was hospitalized with dyspnea due to pneumonia, and ASD was detected in 1984. Cardiac catheterization demonstrated severe pulmonary hypertension. The pulmonary arterial pressure and PVR were 100/38 (63) mm Hg and 16.4 U/[m.sup.2], respectively, in room air. These values did not decrease after oxygen inhalation or tolazoline administration. Open lung biopsy was performed to determine operability. A lung biopsy specimen showed advanced plexogenic arteriopathy with bypass circulation of the occluded lumina in the small pulmonary arteries (Fig 2), as well as plexiform lesions and dilatation lesions. The IPVD was 3.0, and the patient was deemed inoperable. Sixteen years later, the patient is now doing well, and is class 2 of the New York Heart Association classification.
[FIGURE 2 OMITTED]
A new A-E grading is defined as follows in plexogenic arteriopathy: A, small pulmonary arteries with or without cellular proliferation of intima; B, the lumina of a few small pulmonary arteries are partially obstructed by fibrous proliferation of intima; C, the IPVD value is < 2.3, although slight collateral circulation with plexiform lesions or other pathologic morphology is observed; D, the IPVD value is > 2.4 with moderate collateral circulation; and E, collateral circulation is completed with plexiform lesions or other pathologic morphology.
Plexogenic arteriopathy was observed in 32 patients in whom preoperative open lung biopsy diagnosis was performed. Grades A, B, and C were seen in 3 patients, 14 patients, and 8 patients, respectively. However, grades D and E contraindicative of surgery were seen in three patients and four patients, respectively. Surgery was performed in 'all patients classified as A, B, and C, a total of 25 of the 32 patients. All of these patients who underwent operation are still surviving. The remaining seven patients for whom surgery was not indicated are under follow-up observation. No deaths have occurred among these seven patients.
Thromboembolism of the Small Pulmonary Arteries.
As we stated in the previous article, (1) surgery is indicated for all cases of throanboeanbolism of the small pulmonary arteries. We now introduce a patient with thromboembolism and severe pulmonary hypertension.
Patient 3, a 52-Year-Old Woman: In this patient, the symptom of palpitation had appeared 10 years previously. The cardiac catheterization data showed that the pulmonary arterial pressure and PVt/were 100/45 (72) mm Hg and 1,672 dyne.s.[cm.sup.-5], respectively, in room air and 80/34 (48) mm Hg and 775 dyne*s*[cm.sup.-5], respectively, during pure oxygen inhalation. The results indicated the effectiveness of the oxygen inhalation test. Lung biopsy and ASD closure were successfully performed. The postoperative outcome was favorable with significant reduction of pulmonary arterial pressure. Postoperative cardiac catheterization after 4 months of ASD closure showed pulmonary arterial pressure of 42/27 (33) mm Hg. Lung biopsy showed thrombi of the lumina of the small pulmonary 'arteries (Fig 3).
[FIGURE 3 OMITTED]
A-E grading is defined as follows in thromboembolism: A, lumina of small pulmonary arteries are not obstructed by the eccentric, Cushon-like, organized thrombi; and B, lumina are obstructed completely by old or recent embolus with or without recanalization. There are no patients with grades C, D, or E in thromboembolism.
There were five patients who had thromboelnbolism of the small pulmonary arteries. Grades A and B were seen in one patient and four patients, respectively. Surgery was indicated in all five patients, and all have survived in good health up to the present.
Mixed-Type Lesions
In our previous article, (1) we reported that in the patients with plexogenic puhnonary arteriopathy and musculoelastosis, surgery is not indicated if severe concentric laminar intimal fibrosis, plexiform lesions, or dilatation lesions are clearly in evidence. However, since the following patient has survived 10 years since ASD closure, we expanded the operative indications to include patients with mixed-type of plexogenic pulmonary arteriopathy and musculoelastosis in whom bypass circulation of the occluded lumen of the small pulmonary arteries such as plexiform lesions are not observed or are incomplete.
Patient 4, a 31-Year-Old Man: Congenital heart disease was first detected when the patient was 31 years old. Although cyanosis was absent, polycythemia was found: 550 X [10.sup.4]/[micro]L of RBC, and 17.0 g/dL of hemoglobin. Cardiac catheterization revealed severe pulmonary hypertension as shown in Table 2. In 1990, ASD closure and lung biopsy were performed. The postoperative course was uneventful, and postoperative catheterization showed some improvement of hemodynamics (Table 2). Presently, 10 years later, the patient is enjoying his job and social life without any loss of capacity for locomotion. Lung biopsy findings showed severe pulmonary vascular disease. Intimal fibrous thickening with musculoelastosis or concentric lamina intimal fibrosis completely occluded the lumina of some small pulmonary arteries.
Partial destruction and protrusion of the media were also observed (Fig 4). However, recanalization with collateral circulation of the occluded lumen was not found. These findings indicated that in mixed-type lesions, even if there are complete occlusion of the lumina and destruction of the media, closure of ASD is recommended if there are no findings of bypass circulation of the occluded portion or recanalized portion.
[FIGURE 4 OMITTED]
A new A-E grading is defined as follows in mixed-type lesions: A, musculoelastosis and cellular proliferation of intima, at least in part, are observed iii a few small pulmonary arteries; B, the lumina of a few small pulmonary arteries is partially obstructed by musculoelastosis or fibrous proliferation of intima; C, although the lumina of small pulmonary arteries are completely obstructed, there are no findings of collateral circulation of the occluded portion; D, some of the lumina of small pulmonary arteries are completely obstructed and collateral circulation is observed; and E, collateral circulation is completed in all small pulmonary arteries.
In this series, mixed-type PVD was seen in 25 patients. Grades A, B, and C were seen in 0 patients, 5 patients, and 10 patients, respectively. Grades D and E were seen in 8 patients and 2 patients, respectively. Surgery was performed in 15 of the 9.5 patients who deemed operable, and their postoperative course was uneventful. There have been no operative deaths or late deaths to date. Thus, no deaths occurred after ASD closure among the 82 patients who underwent lung biopsy diagnosis.
DISCUSSION
In 1986, we reported PVD in patients with ASD and pulmonary hypertension (4); PVD was classified into four groups: plexogenic pulmonary arteriopathy, musculoelastosis, thromboembolism of the small pulmonary arteries, and mixed-type lesions. Subsequently, in 1987, we detailed lung biopsy of ASD with severe pulmonary hypertension1; open lung biopsy diagnosis of operative indications was discussed, and operative criteria were determined for each group. In this article, these operative criteria are reconsidered, especially in the groups of musculoelastosis and mixed-type PVD. The musculoelastosis initially reported in 1985 was intimal proliferation of longitudinal smooth-muscle cells and elastic fibers, and was especially seen in older patients with ASD. (7) In that report, (1) we concluded that in musculoelastosis, if the vascular lumina of the small pulmonary arteries and arterioles are not completely occluded, closure of ASD is recommended. However, we later noticed that museuloelastosis often results in complete occlusion of the vascular lumina of the small pulmonary arteries and that a patient could survive even if closure of ASD was done. We have herein reported a ease in which successful ASD closure was done, although 70% of all small pulmonary arterial lumina were completely occluded. (8) In this article, we have also presented a patient in whom all of the lumina of the small pulmonary arteries seemed to be completely occluded. In this patient, closure of ASD was done, and the postoperative course was uneventful. The ability of motion was improved and cyanosis disappeared. Pathologic findings clarified the extensive propagation of capillaries around the small pulmonary arteries just proximal to the occluded vascular lumina. This fact suggests that pulmonary blood flows from the small pulmonary arteries to these capillaries directly and that sufficient pulmonary blood flow is maintained. Therefore, we recommend ASD closure for all patients with a diagnosis of simple musculoelastosis, even if all of the small pulmonary arteries seem to be occluded in the biopsied lung sections. Actually, in this series, surgery was performed in all 20 patients with simple musculoelastosis, and there have been no operative deaths or late deaths to date.
In the patients with plexogenic pulmonary arteriopathy, the critical limit of operative indications was IPVD of 2.3, a more severe value than previously determined. Seven patients were followed up without ASD closure because of severe PVD. Most of these patients showed bypass circulation of the occluded lumina of the small pulmonary arteries. Bypass circulation was generally characterized by wide lumina and a thin layer of fibrous tissue, originally part of the adventitia of small pulmonary arteries as shown in Figure 2, and suggested gentle blood flow without any pressure load. Nevertheless, the proximal small pulmonary arteries had a high pressure load. This finding suggests that the proximal small pulmonary arteries lower the pulmonary arterial pressure by vasoconstriction and protect the bypass circulation from destruction of the vascular wall that results in hemoptysis. If ASD closure is done in this condition, when pulmonary arterial pressure suddenly rises due to stress, rupture of the vascular wall will easily occur since there is no outlet through the right-to-left shunt. However, if ASD closure is not done, the patient will be able to live for a long time. The longest survivor among our patients without ASD closure who established complete bypass circulation of the lung is living 16 years after lung biopsy. Therefore, closure of ASD is contraindicated if bypass circulation is complete.
Wagenvoort and Mooi (9) reported a favorable postoperative course after ASD closure in patients with organized thrombi in the small pulmonary arteries. In our series, there were five patients who had thromboembolism in the small pulmonary arteries. Although all of them had severe pulmonary hypertension, ASD closure was done on the basis of the operative criteria introduced in our previous study. Pulmonary arterial pressure greatly decreased in all five patients after surgery, and the postoperative outcome was favorable. We also confirmed that no matter how high the hemodynamic values might be, patients with simple thromboembolism in the small pulmonary arteries are suitable for operation.
In the patients with mixed-type PVD, the IPVD score was not used for determination of operative indications for ASD closure, because musculoelastosis sometimes results in a high IPVD score of > 2.3 in spite of operability. In our experience, patient 3 confirmed the criteria of operative indications for mixed-type ASD, that even if there are complete occlusion of the lumen and destruction of the media, if there are no findings of bypass circulation of occluded portion or the recanalized portion, ASD closure should be done since it alleviates their clinical symptoms such as cyanosis, dyspnea, and difficulty of movement. According to our criteria, surgery was performed in 15 of the 25 patients. The remaining 10 patients for whom surgery was not indicated are under follow-up observation. In these 10 patients, no apparent aggravation of their clinical symptoms has been observed.
ACKNOWLEDGMENT: We acknowledge the following doctors for supplying us with material: Shigeo Nieda, MD, Akita University Hospital, Akita; Michitoshi Otsutomo, MD, Yoshiyuki Okada, MD, Yamagata Prefectural Central Hospital, Yamagata; Shigeo Tanaka, MD, Aomori Prefectural Central Hospital, Aomori; Osamu Kahata, MD, Mito National Hospital, Mito; Aldra Seki, MD, Okazaki City Hospital, Okazaki; Yoshiro Koiwa, MD, Susumu Nagamine, MD, Koji Akimoto, MD, Masato Endo, MD, Hitoshi Yokoyama, MD, Tohoku: University School of Medicine, Sendai; Hiroshi Ajiki, MD, Sapporo Medical University, Sapporo; Hiroshi Suzuki, MD, Yamagata University Hospital, Yamagata; Toshio Kikuchi, MD, Sakakibara Heart Institute, Tokyo; Kenichi Kosuga, MD, Kurume University Hospital, Kurume; Jiro Kondo, MD, Yokohama City University Hospital, Yokohama; Takashi Kudo, MD, Aomori Kosei Hospital, Aomori; Hitoshi Yamauchi, MD, Shigeo Tanaka, MD, Nippon Medical University, Tokyo; Yuichiro Nakamura, MD, Hideaki Kado, MD, Fukuoka City Children Hospital, Fukuoka; Shigekazu Sato, MD, Tohoku Kosai Hospital, Sendai; Kyo Shunei, MD, Saitama Medical University, Moroyama; Hiroshi Matsuzaki, MD, Shigeki Morita, MD, Hisataka Yasui, Kyushu University Hospital, Fukuoka; Kazuhiro Hashimoto, MD, Kei Tanaka, MD, Hiromi Kurosawa, MD, Jikei University Hospital, Tokyo; Shinnichi Nomoto, MD, Toshihiko Ban, MD. Kyoto University Hospital, Kyoto; Eiji Ishizawa, MD, Iwate Prefectural Central Hopital, Morioka; Mitsunori Otubo, MD, Hokkaido University Hospital, Sapporo; Fmnio Iwaya, MD, Fukushima Medical University, Fukushima; Hiroyuki Tanaka, MD, Fujigaoka Hospital of Showa University, Yokohama; Masanobu Maeda, MD, Chukyo Hospital, Nagoya; Tomohiko Watanabe, MD, Nagoya City University Hospital, Nagoya; Sciichi Watanabe, MD, Tsuchiura Kyodo Hospital, Tuchiura; Miwako Kado, MD, Mitio Yokota, MD, Shizuoka Children Hospital, Shizuoka; Kunitaka Shiroo, MD, Akira Seze, MD, Kyushu Koseinenkin Hospital, Kitakyushu; Masaaki Kawada, MD, Shunji Sano, MD, Okayama University Hospital, Okayama; Tomonori Yamamoto, MD, Nihon University Hospital, Tokyo; Yoshikazu Tsuruhara, MD, Kagawa Medical University, Kagawa Pref.; Takahiko Nakame, MD, Semine Prefectural Hospital, Miyagi Pref.; Shu Oosaki, MD, Tsuchiya Hospital, Hiroshima; Kazunobu Ban, MD, Tokai University Hospital, Isehara. We also wish to thank the following technical assistants: Mrs. Takako Kato, Mr. Mitsuru Sasaki, Mrs. Junko Watanabe and Mrs. Miyuki Abe, Sendai City, Medical Center, Sendai.
REFERENCES
(1) Yamaki S, Horiuchi T, Miura M, et al. Secundum atrial septal defect with severe pulmonary hypertension: open lung biopsy diagnosis of operative indication. Chest 1987; 91:33-38
(2) Goldner J. A modification of the Masson trichrome technique for the routine laboratory purposes. Am J Pathol 1938; 14:237-243
(3) Yamaki S, Abe I, Endo M, et al. Surgical indication fur congenital heart disease with extremely thickened media of small pulmonary arteries. Ann Thorac Surg 1998; 66:1560-1564
(4) Yamaki S, Horiuchi T, Miura M, et al. Pulmonary vascular disease in secundum atrial septal defect with pulmonary hypertension. Chest 1986; 89:694-698
(5) Yamaki S. Lung biopsy diagnosis of pulmonary vascular disease. Tokyo, Japan: Medical Review, 2000, 89-92
(6) Yamaki S, Tezuka F. Quantitative analysis of pulmonary vascular disease in complete transposition of the great arteries. Circulation 1976; 54:805-809
(7) Yamaki S, Horiuchi T, Miura M, et al. Musculeelastosis: a change of small pulmonary arteries found in a case with atrial septal defect and pulmonary hypertension. Tohoku J Exp Med 1985; 145:455-463
(8) Yamauchi S, Yamaki S. Fujii M, et al. Reduction in recalcitrant pulmonary, hypertension after operation for atrial septal defect. Ann Thorac Surg 2001; 72:905-907
(9) Wagenvoort CA, Mooi WJ. Biopsy pathology of the pulmonary vasculature. New York, NY: Chapman and Hall, 1989; 128-147
* From the Japanese Research Institution of Pulmonary Vasculature (Dr. Yamaki), Shiroishi; Department of Cardiovascular Surgery (Dr. Kumate), St. Maria Hospital, Kurume; Department of Pediatrics (Dr. Yonesaka), Hirosaki University School of Health Science, Hirosaki; Department of Cardiothoracic Surgery (Dr. Maeda), Tokyo University, Tokyo; and Department of Cardiovascular Surgery (Drs. Endo and Tabayashi), Tohoku University Hospital, Sendai, Japan.
Manuscript received December 19, 2003; revision accepted April 26, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Shigeo Yamaki, MD, Japanese Research Institution of Pulmonary Vasculature, 40-1 Usagisaku, Shiroishi, Miyagi Pref., Japan 989-0228; e-mail: syamaki@ff.iij4u.or.jp
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group