INTRODUCTION: The American College of Chest Physicians is leading the charge to integrate the skills of pain management and palliative care into ICU practice. This case poignantly illustrates how opiate mismanagement can threaten patient safety. We describe how suboptimal care transformed an otherwise successful laminectomy into a protracted ICU stay complicated by acute respiratory distress syndrome (ARDS).
CASE PRESENTATION: A 50 year-old man who was failing conservative management for longstanding backpain was hospitalized for a laminectomy under spinal anesthesia. He had used controlled-release oral morphine at a dose of 100mg three times a day for several years. Post-operative pain management included only an epidural catheter with bupivicaine infusion and oral codeine for break through pain. By the end of post-operative day one, increasing doses of codeine were ineffective at relieving pain and intravenous morphine was administered. The patient complained of nausea which was treated per a standing order with 1 cc intravenous droperidol. Thirty minutes later he was noted to be somnolent, hypopneic, and hypoxic. Again following a standing order, 1 nag intravenous naloxone was administered. The patient screamed, had paroxysms of emesis, pulled out his intravenous line, experienced explosive diarrhea, and aspirated. His symptoms subsided over the ensuing thirty minutes, but he became increasingly somnolent and hypoxic despite receiving no additional medications; eventually an endotracheal tube was placed. He was diagnosed with ARDS and required mechanical ventilation for 14 days; he also manifested acute tubular necrosis with a peak serum creatinine of 3.4. As his pulmonary and renal processes began to reverse, he was noted to be persistently unresponsive, leading to a head CT (negative). Sedative (propofol) and opiate medications (intravenous morphine) were stopped; two days later he was noted to have a pulse of 148 with irregularity, a blood pressure of 180/100, and a temperature of 100.1 F. He experienced ventilator dyssynchrony, tachypnea at over 40 breaths per minute, and agitated delirium. Hydromorphone 1.5 mg intravenous resulted in stabilization within 10 minutes and epidural medications and opiates were restarted. Four days later he emerged from his coma and was liberated from the ventilator; he complained of diffuse abdominal pain and bloating. Review of nursing notes revealed no bowel movement since the explosive diarrhea 22 days ago, despite nasogastric feeding. Aggressive therapy for obstipation was initiated, and after a four week hospital stay, the patient was discharged to a rehabilitation facility. Although differential diagnoses are broad for many of the manifestations in this case, opiate mismanagement was implicated for the complications reviewed in this presentation.
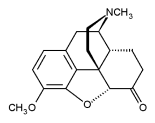
DISCUSSIONS. Multiple opportunities for improved quality of care for pain and symptom management exist in this case. Chronic opiate use and physiologic dependence led to withdrawal on multiple occassions due to insufficient weaning of opiates. Over-medication with sedatives can increase opiate respiratory depression. Use of naloxone in dose range 0.04-0.1mg every five minutes can avoid the acute reaction that precipitated aspiration and serious lung injury in this patient. Codeine was likely ineffective, whereas hydrocodone and morphine produced expected clinical responses, likely due a polymorphism in debrisoquin hydroxylase which is required to convert codeine to its active metabolite, morphine (6-10 % of Caucasians). Morphine generally has a half life of 2-4 hours; however central nervous effects can be markedly prolonged by an active metabolite, morphine-6-glucoronide, especially in renal insufficiency. Bowel prophylaxis is essential in all patients on opiate medications and should include both a stimulant agent and a stool softener.
CONCLUSION: Integration of palliative care and pain management skills into ICU medical care can lead to improvements in patients' symptom experience and, as demonstrated in this case, may help improve patient safety and overall quality of care.
DISCLOSURE: Richard Mularski, Grant monies (from sources other than industry) AHRQ, NINR, CMS, NCI, National Quality Forum, American Lung Association of Oregon, & Northwest Health Foundation
Richard A. Mularski MD * Karen S. Mularski MD Steven M. Asch MD VA Greater Los Angeles Healthcare System, Los Angeles, CA
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group