One Woman's Experience with Intractable Nonmalignant Chronic Pain
-An Interview with Patient Karen Balzer
One prescription for the proper compounded medicine turned everything around...
Of all the challenges that have shaped the work of artist Karen Balzer, none is greater than her victory over chronic debilitating pain. Since 1991, Karen has suffered from total-body regional sympathetic dystrophy syndrome (RSDS), a burning paresthesia that developed after surgery to relieve long-undiagnosed spinal stenosis. When her symptoms began, she was 47 years of age. Her refusal to accept what proved to be a misdiagnosis, her rejection of physicians who ignored or dismissed her symptoms, and her persistence in seeking effective treatment are a tribute to her life and her art.
RSDS is an elusive entity. Its pathogenesis is unknown, and diagnosis and treatment are difficult.1 The disorder may involve a genetic component.2 Karen's mother was afflicted with a similar painful condition accompanied by paralysis, which, at the time of her death at the age of 68 years, had progressed to quadriplegia.
For years, Karen's efforts to obtain relief from the chronic pain, which progressed slowly from her feet to the top of her head, were met with reserve and skepticism from physicians who denied her analgesia. Compounding pharmacy eventually yielded the most effective solution. In the following interview, Karen Balzer conveys a powerful message about the views of the United States medical establishment on providing narcotic drugs to relieve severe nonmalignant pain. She describes her ultimately successful quest for effective treatment as "a journey through doctor-hop hell." Her experience is a cautionary tale for all healthcare professionals treating patients whose relentless pain has no relief. -The Editor
How did your RSDS evolve?
In 1991, I began to experience the symptoms of restless legs syndrome, which soon evolved into a burning sensation in my toes (primarily my big toes). Most of the time, my feet, which felt as if they were about three times larger than they actually were, seemed painfully sensitive to touch, but occasionally they were numb. I felt as if I were walking barefoot over rocks. Eventually, I could not wear shoes with heels, and often I could not walk at all. Those conditions have never completely resolved.
When I consulted my primary care physician, he didn't believe that my discomfort was as bad as it truly was. The tests he ordered revealed no disorder, and he prescribed no treatment. Finally, I began to experience a stabbing pain in my legs. I could hardly walk because the pain was so bad, and I fell frequently. In addition to allopathic treatment, I tried chiropractic medicine. Nothing helped. I knew that something was terribly wrong.
Finally, after I'd experienced this progressive pain for about a year, I underwent magnetic resonance imaging of the spine, which was misread as revealing a herniated disc. Exercise, including hatha yoga and swimming, was prescribed as treatment, but nothing relieved my discomfort. For 4 years, I had received no therapy for the pain I'd been experiencing, and my symptoms continued to intensify. The burning sensation and painful sensitivity progressed from my feet to my head, and I was in such pain that I could not function. I finally sought help from a pain management specialist in Oregon, who performed his own tests and diagnosed long-standing severe spinal stenosis. He confirmed that my original diagnosis was incorrect. I underwent immediate decompression laminectomy, but permanent damage to my spinal cord had already occurred. I noticed some pain relief after the surgery, but the burning sensation actually increased. My surgeon suggested that I contact a pain management clinic for follow-up care.
Which did you receive for pain after the surgery?
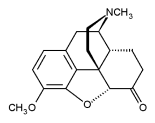
The pain management specialist to whom I was referred prescribed OxyContin (oxycodone hydrochloride), Vicodin (hydrocodone/acetaminophen), and Neurontin (gabapentin). Those drugs reduced the generalized pain, but nothing was effective in relieving the unremitting burning sensation and occasional stabbing pain. At that point, my pain rating on a scale of 1 to 10 was approaching a score of 10. My only alternative was morphine, which my specialist prescribed in oral tablet form. Most physicians, though, are reluctant to prescribe the volume of oral morphine that I have required to maintain relief. Unfortunately, my pain management specialist left the practice, and another doctor was assigned to my case.
Did your new physician prescribe different treatment?
Yes. He decided to taper my morphine treatment and refused to believe that the pain and burning sensation recurred with full intensity throughout my body as the drug was withdrawn. I began to feel as if my internal organs were on fire. My physician finally withdrew all analgesic treatment except for Tylenol 3 (acetaminophen with codeine). My life became unbearable because of the unremitting burning and pain. My doctor did not believe me when I asked again for help. Eventually, I became very depressed and decided to seek treatment with another physician.
Did your new clinician prescribe effective analgesia?
No. I was treated next by the staff of another pain management and rehabilitation clinic based at a local university. A clinical psychologist there identified severe chronic pain as the cause of my depression. However, the physician specialist who examined me disagreed. In front of a group of students, he called me a liar, attributed my symptoms to an allergic skin reaction, and suggested that I was only seeking prescriptions for narcotics. He prescribed Ultram (tramadol) for pain, Neurontin for the burning sensation, imipramine for depression, and cyclobenzaprine for muscle cramps, which I was also experiencing. For a while, those drugs were effective in relieving the symptoms for which they were prescribed, but they didn't relieve the burning, which doubled in intensity after about 1 month of therapy.
At that point, I decided to stop treatment with all the drugs prescribed, because they only partially relieved pain, did not relieve the burning sensation, and caused adverse effects. I moved away from allopathic medicine and again tried naturopathic treatments, which were ultimately ineffective. At that point, I felt as if I had poured a strong liniment over every cell of my body and into every orifice. My skin was red and hot to the touch. I was on fire, 24 hours a day. My naturopathic physician referred me to another pain specialist experienced in nerve stimulation techniques, which unfortunately were also ineffective. That specialist referred me to a doctor who implanted a pump in my abdomen and prescribed a compounded morphine solution for infusion.
Was the infusion pump an effective modality?
The result was miraculous! The compounded morphine stopped the constant severe burning and caused no side effects. It saved my life. I began to feel like a normal person. At some point, however, the medication in the infusion was changed without my knowledge, and treatment became ineffective. I began to feel very ill, to the point at which I could not function. My physician suggested supplementing the infusion with oral morphine tablets, which did not make sense to me. I began to suspect that my feeling ill was caused by an error in the compounded solution with which I was treated, and I decided to ask the manufacturer of my infusion pump for referral to another pain management physician. That was exactly the right thing to do. The doctor suggested by the infusion pump manufacturer was excellent. He refilled my pump with a fresh solution of morphine that was immediately effective, and he has treated my chronic pain ever since.
After 3 years of treatment with infused morphine, I've been able to function reasonably well and have experienced no side effects. If I had not been able to obtain the infusion pump, I know that I'd be dead now. I am never completely pain free, but my discomfort remains at a level of about 3 or 4 instead of 10-plus. My limbs still often feel as if they are "asleep," and sometimes I have great difficulty in staying awake. I still have severe pain that often makes walking difficult or impossible. But treatment with compounded morphine by infusion, antidepressants, and various other analgesics enables me to find relief.
If you were to comment on life with severe chronic pain, what would you say?
Living with chronic pain is hell. I feel very sorry for people who suffer from severe pain and can't get the help they need. If you look better than you feel, most doctors dismiss your chronic pain symptoms; they don't believe you.
Doctors must listen to and believe their patients. But even physicians who do take you seriously often refuse to negotiate the regulatory roadblocks that make prescribing drugs like morphine so difficult. In my case, treatment with an infusion pump somehow legitimizes treatment with narcotics. I feel very fortunate; I know that the relief the morphine pump provides saved my life.
My compounding pharmacist is of great help. He alerts me about possible drug interactions and helps me in so many ways! I truly believe that doctors should learn more about the drugs they prescribe by consulting with a compounding pharmacist. A qualified compounder can help physicians break away from the rigid treatment paradigms supplied by pharmaceutical manufacturers and solve elusive medical problems creatively, safely, and effectively. The medical profession would be greatly improved if pharmacists were more involved in day-to-day medical practice.
To others with chronic pain, I'd say 'Don't give up! If you find a passion and lose yourself in pursuing it, life is worth living; you won't feel your discomfort and your pain as much. Don't be afraid to do the doctor hop until you find a caring physician who will truly help you.'
Address correspondence to Karen Balzer. E-mail: al_balzer@evl.net
References
1. Veldman PH, Reynen HM, Arntz IE et al. Signs and symptoms of reflex sympathetic dystrophy: Prospective study of 829 patients. Lancet 1993; 342(8878):1012-1016.
2. Mailis A, Wade J. Profile of Caucasian women with possible genetic predisposition to reflex sympathetic dystrophy: A pilot study. Clin J Pain 1994; 10(3):210-217.
Copyright International Journal of Pharmaceutical Compounding Sep/Oct 2005
Provided by ProQuest Information and Learning Company. All rights Reserved