Practice recommendations
* Become familiar with the strains, concentrations, and preparations of probiotics most likely to be effective.
* Because a given individual may respond well to probiotics, suggest a trial of a probiotic supplement-perhaps conducting an n-of-1 trial for an objective assessment.
* If a trial of probiotic does not achieve desired results, advise the patient of the many other options to treat lactose intolerance.
Abstract
Purpose To assess the efficacy of oral probiotics in adults with lactose intolerance through a systematic review of its effects on symptoms and breath hydrogen tests, and whether adding probiotics to nonfermented dairy products decreases lactose intolerance at that meal.
Methods We searched randomized controlled trials published between 1966 and December 2002. Databases in the search strategy included Medline and AMED. We reviewed references of clinical trials and contacted authors of major articles and manufacturers of probiotic commercial products. Quality assessment was based on the McMaster guides and was performed by 5 independent reviewers. Data extraction was performed by 2 reviewers.
Results A master list of 90 articles was compiled. Ten articles met inclusion and exclusion criteria and were consistent with our clinical question. Of the 9 studies that measured breath hydrogen, 3 were positive, 3 were negative, and 3 had both positive and negative results. Of the 7 studies that measured symptoms, 1 yielded positive results, 5 were negative, and 1 had both positive and negative outcomes.
Conclusions Probiotic supplementation in general did not alleviate the symptoms and signs of lactose intolerance in adults in this review. Some evidence suggests that specific strains, concentrations, and preparations are effective. Further clinical trials of specific strains and concentrations are necessary to delineate this potential therapeutic relationship.
Judging from our systematic review of the literature, probiotic supplementation is not effective universally for lactose intolerance in adults. However, some evidence suggests that specific strains, concentrations, and preparations of probiotics can be effective.
Discuss probiotic supplementation with lactose-intolerant patients. "Try it" is a reasonable suggestion, given additional evidence that there are individuals whose symptoms of lactose intolerance will, for unknown reasons, respond to probiotics.
For those who find no benefit in probiotics, several other therapeutic options can be recommended.
* Prevailing wisdom about lactose intolerance
Lactose intolerant persons suffer such symptoms as abdominal cramping, bloating, and diarrhea after ingesting lactose-containing foods, including nonfermented dairy products. (1) This intolerance to dairy products may result in a person receiving less than the recommended intake of calcium and protein, especially in developing countries.
Primary lactase deficiency is the most common form of lactose intolerance? In the US, 15% of Caucasians, over 50% of Mexican Americans, and over 80% of African Americans have lactose intolerance. (2)
Treatment options for lactase deficiency
Lactose-intolerant persons digest yogurt, which is fermented, more easily than milk. (2) Nonfermented lactose-containing foods can be consumed in small quantities or with proteins and fats to delay gastric emptying. Nonfermented dairy products are generally tolerated if they are prehydrolyzed to reduce levels of lactose (such as reduced-lactose or lactose-free milk). Finally, synthetic enzyme (lactase) tablets can be taken with lactose-containing dairy foods in an attempt to alleviate symptoms. (2)
What are probiotics?
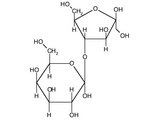
Probiotics are live microorganisms that, when ingested, have beneficial effects on the prevention or treatment of disease. (3) Some probiotics, such as Lactobacillus, contain [beta]galactosidase or lactase intracellularly so that ingestion of lactase-containing probiotics might be beneficial for lactose-intolerant individuals, either consumed with food or taken separately as a supplement.
Theoretically, probiotics ingested as supplements would adhere to the intestinal lining and digest dietary lactose, thereby alleviating malabsorptive symptoms from excessive lactose. Probiotics have other positive effects: treating and preventing diarrhea (infectious and antibiotic induced), relieving symptoms of irritable bowel syndrome, alleviating inflammatory bowel disease, and decreasing atopic disease. (4, 5) The Food and Agriculture Organization of the United Nations and the World Health Organization have reported that there is adequate scientific evidence of the potential for probiotic foods to provide health benefits, and that specific strains are safe for human use. (6)
Purported advantages of probiotics.
Probiotic supplementation may be preferred over lactose-free products due to the inability to monitor and control all dairy products consumed. The varied efficacy of lactase enzymes in different individuals may render probiotics the favored supplement. Also, the option of a natural treatment may appeal to many people.
Testing for lactose intolerance
The hydrogen breath test is the gold standard for diagnosing lactose intolerance. Intestinal bacteria metabolize carbohydrate to generate hydrogen that is rapidly absorbed into the blood perfusing the gut and cleared during a single passage through the lungs.
A lactose dose of 25 to 50 g is given after an overnight fast. A rise in the hydrogen level of more than 20 parts per million (ppm) over baseline suggests hypolactasia. (7) At a cutoff of 20 ppm, the test has a specificity of 90%. False positives may occur secondary to severe bacterial overgrowth of the small bowel, smoking, and aspirin use. False negative results are seen in persons receiving oral antibiotics or high colonic enemas, suffering severe diarrhea, or lacking bacterial flora. (8)
Another use of the breath hydrogen test is to measure the quantity of lactose malabsorbed. This theory was based on a study of lactulose in which ingested doses of 5, 10, or 20 g resulted in a linear increase in breath hydrogen along with the similar malabsorption patterns of lactulose and lactose. (9)
The purpose of our systematic review was to determine if probiotics have a positive effect in patients with lactose intolerance. We found no systematic reviews or meta-analyses in the Cochrane Database of Systematic Reviews or the Database of Reviews of Effectiveness (DARE).
* Methods
Inclusion criteria
The clinical question researched was "Does the addition of probiotics to nonfermented dairy products decrease lactose intolerance at a single meal?" Inclusion criteria for review were studies that were randomized placebo-controlled clinical trials, that involved adults diagnosed with lactose intolerance via breath hydrogen >20 ppm above baseline after lactose consumption, that used probiotic supplementation in any form as the intervention, and that included the outcomes of symptoms or breath hydrogen test results.
Search strategy and assessment
Four authors (MD, KK, KL, JM) independently searched Medline and Allied and Complementary Medicine Database (AMED) for studies published between 1966 and December 2002. Four authors performed individual searches using the Medical Subject Heading (MESH) terms 1) "lactose intolerance" and "Lactobacillus"; 2) "lactose intolerance" and "probiotics"; 3) "lactose intolerance" and "yogurt"; and 4) "diarrhea, bloating, abdominal pain" and "yogurt." The search strategies for each member were documented, and the resulting published listings were combined.
The initial set of articles was pulled and references from those studies were searched. In addition, manufacturers of Lactobacillus supplements and authors identified with expertise in lactose intolerance were contacted by phone or e-mail in an effort to look for any unpublished or ongoing trials possibly missed in the initial search.
Each author independently assessed each of the selected articles for validity using the recommendations made by the Evidence-Based Medicine Working Group at McMaster University. (10) These validity criteria included patient similarity, evidence of controls, randomization, allocation concealment, blinding, completion of follow-up, use of intention-to-treat, and similarity of intervention and control groups. The authors then met to discuss their assessment and clarify any article concerns. General agreement was reached, and there were no dissenting views.
Data extraction
A standardized data extraction form was developed by 1 author (FD) and each paper's information was extracted by 1 of the other authors (KL) and verified by the final author (FD). The following data were extracted: number of treatment arms, types of treatment arms (including forms of probiotics), number of subjects per treatment arm, study design, data presentation, and results obtained.
No formal statistical procedures or tests were performed. Authors hoped that appropriate data could be collected from each paper so that a meta-analysis could be performed. However, the lack of standardized data presentation for breath hydrogen and symptom results made data pooling impossible.
* Results
Medline and AMED searches yielded 75 clinical trials. The reference search from these studies gave an additional 15 trials. No studies were identified through manufacturer or expert author inquiries. From the master list of 90 studies, 22 met inclusion and exclusion criteria. Of the 22, 10 were consistent with our clinical question. Of these 10 articles used in the study, 8 were obtained from the Medline and AMED searches, and 2 were obtained from the references.
Of the 10 randomized placebo-controlled trials, sample sizes for probiotic treatment arms ranged from 5 (Dehkordi) to 20 (Lin & Yen). Probiotic arms varied in subtype, strain, and concentration. Most of the studies (9) used the Lactobacillus acidophilus subtype as the intervention. Four trials examined probiotics other than, or in addition to, L acidophilus (Dehkordi, Jiang, Lin & Yen, Lin & Savaiano). Dehkordi performed 2 experiments. The first experiment examined the additive of effect of Lactobacillus and Bifidobacterium longum. The second compared only Lactobacillus strains with control milk.
Lin & Savaiano in 1990 compared 3 Lactobacillus strains, each with 2 different concentrations, as well as the combination probiotic subtypes of Streptococcus thermophilus/Lactobacillus bulgaricus at 2 concentrations with the control milk.
In 1998, Lin & Yen compared 2 concentrations of an L acidophilus strain and 2 concentrations of an L bulgaricus strain with placebo. McDonough examined the effects of sonicated (intracellular lactase release) acidophilus milk in addition to acidophilus milk on breath hydrogen results.
Four of the 10 randomized controlled trials were performed in a crossover design (Newcomer, Lin & Savaiano, Lin & Yen, and Savaiano) while the remaining 6 varied in randomized designs.
TABLE 1 shows the validity characteristics for the 10 clinical trials published between 1981 and 1998 that met inclusion and exclusion criteria. While all were randomized controlled trials with similar patients, interventions, and controls, none of the 10 concealed the allocation of the interventions. Lin & Yen's 1998 study failed to mention the percentage of subjects followed-up and, thus, intention-to-treat did not figure into the analysis. Three of the 10 (Dehkordi, Onwulata, McDonough) did not specify if their studies involved double-blinding.
Descriptors of each trial's treatment arms, subjects, design, data presentation, and results are shown in TABLE W1 (available online at www.jfponline.com). Of the 9 studies that measured the disease-oriented outcome of breath hydrogen, 3 were positive, 3 were negative, and 3 had both positive and negative (mixed) results. Of the 7 studies that measured the patient-oriented outcome of symptoms, 1 yielded positive results, 5 were negative, and 1 had mixed outcomes (TABLE 2).
* Discussion
This review of controlled clinical trials produced a negative answer to the question: "Do probiotics decrease lactose intolerance at a single meal including nonfermented dairy products?" We reviewed articles that involved the simultaneous combination of probiotics and non-fermented dairy products in objectively identified lactose-intolerant individuals.
Strengths of this review
All review studies selected patients who had both gastrointestinal symptoms and positive breath hydrogen test results. All studies used appropriate methodology of randomized design (LOE: 1b). All studies involved a control group or a crossover design in which intervention patients served as their own controls. Further strengths of this review are an adequate number of studies with strong methodology, most (7 of 10) measured the patient-oriented outcome of symptoms, and reports of no adverse effects of probiotic treatments.
Weaknesses of the review
The variations in probiotic subtype, strain, and concentration are weaknesses in this review. Probiotic subtypes and strains vary with regard to [beta]-galactosidase activity, intestinal adherence, cell wall thickness, and other characteristics that may affect clinical efficacy. Jiang showed significant breath hydrogen results with B longum B6 grown in lactose-containing media, while the same strain grown in glucose- and lactose-containing media was not effective. He also found the former strain significantly reduced the symptom of flatulence but not pain, meteorism, borborygmi, or diarrhea.
Only 2 of the 9 L acidophilus studies reported use of similar strains of L acidophilus B (Mustapha, Lin and Yen). Six of the 9 L acidophilus studies accounted for the probiotic subtype and concentration but not its strain. Instead the L acidophilus intervention was expressed as L acidophilus milk or sweet acidophilus milk (Dehkordi, Newcomer, Onwulata, Savaiano, McDonough, Kim). A potential strain outcome association may exist with L acidophilus B. Both Mustapha and Lin and Yen showed positive outcomes with this treatment arm in breath hydrogen and symptom results (TABLE W1, available online at www.jfponline.com).
Trials using L bulgaricus (Lin, Savaiano, and Lin and Yen) may have isolated a therapeutic subtype other than acidophilus. Lin, Savaiano found that 1 of 2 L bulgaricus/S thermophilus combinations significantly reduced symptoms. Whether this difference may be attributed to 1 of the 2 subtypes or their combination can only be speculated.
Additionally, Lin and Yen found that both strains of L bulgaricus 449 at concentrations of [10.sup.8] and [10.sup.9] significantly improved breath hydrogen and symptom scores. This positive association may be related to any or all of its subtype, strain, or concentration. Also in that study, both probiotic subtypes of L acidophilus and L bulgaricus at concentrations of [10.sup.9] significantly reduce symptoms. Unfortunately, there was not enough specific information on strain characteristics to draw any firm conclusions. In future studies, careful attention to bacterial characteristics may provide a definitive answer to our questions.
The lack of standardized data presentation for breath hydrogen and symptoms in these 10 trials was a limitation. Some papers had only graphs of mean breath hydrogen, some showed differences from baseline, and some showed various summary statistics of breath hydrogen over different time periods. There was no standard objective measure of symptoms such as a Likert scale. Instead, symptoms were expressed in various ways (number of instances, scoring systems, or sole mention in text format). For these reasons, a meta-analysis could not be performed. This review could be further criticized because authors were not directly contacted for raw data for a potential meta-analysis.
Recommendations from this review
Several recommendations can be extracted from the results of this review.
First, probiotics in general do not reduce lactose intolerance (SOR: A). However, some evidence suggests that specific strains and concentrations are effective (SOR: B).
Second, there were enough positive treatment arms to suggest that some individuals will, for unknown reasons, have their symptoms eliminated or reduced with probiotics (SOR: B). It is reasonable, therefore, for clinicians to simply tell patients to "try it." For a more objective analysis, an n-of-1 trial could be used. (21) Clinicians will have to keep in mind that many people presumed to have lactose intolerance do not meet standard diagnostic criteria when objectively assessed.
Third, several strategies are available to lactose-intolerant persons (SOR: C). Yogurt, lactase enzymes, lactose-free or lactose-reduced products, specific foods, and probiotics selective for strain, concentration, and preparation are all supported by evidence. Onwulata compared results of probiotic milk, lactase tablets plus milk, hydrolyzed lactose milk, and yogurt with that of whole milk. Only yogurt and hydrolyzed lactose milk yielded significantly lower breath hydrogen results. Six of 10 patients reported symptoms with probiotic milk, 3 of 10 with lactase tablets, 1 of 10 with hydrolyzed milk, and no symptoms were reported with yogurt.
Dehkordi showed that probiotic milk had no effect on breath hydrogen results, but his treatment arm of cornflakes with whole milk did significantly affect results. McDonough found that when sweet acidophilus milk was sonicated to release intracellular lactase from the bacterial cells, a significant change in breath hydrogen resulted. Unfortunately, neither Dehkordi nor McDonough measured symptoms in their studies to specify patient-oriented outcomes.
Fourth, many individuals with symptoms of lactose intolerance do not meet the definition of diagnosis as measured by breath hydrogen testing (SOR: B). All clinical trials in this review declined subject enrollment if lactose intolerance symptoms were unconfirmed by breath hydrogen testing, thereby accepting only true positives.
There are several reasons why probiotic supplementation may be superior to commercial lactase supplementation. Patients have varied responses to lactase supplementation with meals, and different preparations may be more or less effective for the same quantity of lactose ingested. (22) Also, as mentioned earlier, other research supports the role of probiotics in preventing diarrheal illness, treating irritable bowel syndrome and inflammatory bowel disease, and possibly benefiting persons with atopic disease. Finally, if lactase-producing probiotics are clinically effective and can also adhere to the intestinal lining, patients may experience prolonged reduction or remission of symptoms without the need to ingest any tablets with meals.
Two of the 10 studies (Newcomer, Kim) examined long-term probiotic use for 1 and 2 weeks, respectively. Newcomer measured only symptoms, showing no significant difference between L acidophilus milk and unaltered milk. Kim found that 2 of 3 L acidophilus concentrations significantly decreased breath hydrogen results, but the study did not measure symptoms. We can infer a negative patient-oriented outcome of long-term probiotic intervention based on these 2 trials. However, this domain of chronic probiotic use to reduce lactose intolerance would benefit from additional studies for comparison.
In conclusion, probiotic supplementation in general was not effective at reducing lactose intolerance of adults. Some evidence suggests that certain strains, concentrations, and preparations are effective. Clinicians could discuss probiotic supplementation with patients as an alternative treatment. There were enough positive treatment arms to suggest there may be individuals who respond to probiotics. Further studies are needed to determine specific probiotic relationships. The best studies would be those using crossover randomized double-blind design of selected probiotic strains and concentrations and objectively measuring breath hydrogen and symptoms with a long enough wash-out period to eliminate the chance of gut colonization.
ACKNOWLEDGMENTS
Material in this article has been previously presented at the following: "Probiotic Supplementation as Treatment for Lactose Intolerance: a Systematic Review," Fellows works-in-progress poster presentation at the STFM 36th Annual Conference, Atlanta, GA, September 2003, Kara M. Levri, Kari Ketvertis, Mark Deramo, Joel H. Merenstein, Frank D'Amico; "Probiotic Supplementation as Treatment for Lactose Intolerance: A Systematic Review," Grand Professor Rounds, UPMC St. Margaret, Pittsburgh, Pa, June 2003, Kara M. Levri, Kari Ketvertis, Mark Deramo; "Probiotic Supplementation as Treatment for Lactose Intolerance: a Systematic Review," Pennsylvania Academy of Family Physicians Research Day, Philadelphia, Pa, April 2003, Kara M. Levri.
CONFLICTS OF INTEREST
The authors of this article have no conflicts of interest to declare.
REFERENCES
(1.) Haubrich WS, Schaffner F, Berk JE. Gastroenterology. Philadelphia, Pa: W.B. Saunders; 1995.
(2.) Vesa TH, Marteau P, Korpeia R. Lactose intolerance. J Am Col Nutr 2000; 19:165S-175S.
(3.) McFarland LV, Elmer GW. Biotherapeutic agents: past, present and future. Microecol Ther 1995; 23:46-73.
(4.) Kopp-Hoolihan L. Prophylactic and therapeutic uses of probiotics: a review. J Am Diet Assoc 2001; 101:229-241.
(5.) Drisko J, Giles C, Bischoff B. Probiotics in health maintenance and disease prevention. AIt Med Rev 2003; 8:143-155.
(6.) Food and Agriculture Organization of the United Nations and World Health Organization. Regulatory and clinical aspects of dairy probiotics. Food and Agriculture Organization of the United Nations and World Health Organization Expert Consultation Report. Food and Agriculture Organization of the United Nations and World Health Organization Working Group Report; 2001. Available at: www.isapp.net/probio_report.pdf.
(7.) Newcomer AD, McGill DB, Thomas PJ, Hofman AF. Prospective comparison of indirect methods for detecting lactase deficiency. N Engl J Med 1975; 293:1232.
(8.) Kerlin P, Wong L. Breath hydrogen testing in bacterial overgrowth of the small intestine. Gastroenterology 1988; 95:982.
(9.) Florent C, Flourie B, Leblond A, Rautureau M, Bernier JJ, Rambaud JC. Influence of chronic lactulose ingestion on the colonic metabolism of lactulose in man (an in vivo study). J Clin Invest 1985; 75:608-613.
(10.) Slawson DC, Shaughnessy AF. Teaching information mastery: Creating informed consumers of medical information. JABFP 1999; 12:444-449.
(11.) Dehkordi N, Rao DR, Warren AP, Chawan CB. Lactose malabsorption as influenced by chocolate milk, skim milk, sucrose, whole milk, and lactic cultures. J Am Dietetic Assoc 1995; 95:484-486.
(12.) Jiang T, Mustapha A, Savaiano D. Improvement of lactose digestion in humans by ingestion of unfermented milk containing bifidobacterium Iongum. J Dairy Sci 1996; 79:750-757.
(13.) Mustapha A, Jiang T, Savaiano DA. Improvement of lactose digestion by humans following ingestion of unfermented acidophilus milk: influence of bile sensitivity, lactose transport, and acid tolerance of lactobacillus acidophilus. J Dairy Sci 1997; 80:1537-1545.
(14.) Newcomer AD, Park HS, O'Brien PC, McGill DB. Response of patients with irritable bowel syndrome and lactase deficiency using unfermented acidophilus milk. Am J Clin Nutrition 1983; 38:257-263.
(15.) Onwulata CI, Rao DR, Vankineni. Relative efficiency of yogurt, sweet acidophilus milk, hydrolyzed-lactose milk, and a commercial lactase tablet in alleviating lactose maldigestion. Am J Clin Nutrition 1989; 49:1233-1237.
(16.) Lin MY, Savaiano D, Harlander S. Influence of nonfermented dairy products containing bacterial starter cultures on lactose maldigestion in humans. J Dairy Sci 1991; 74:87-95.
(17.) Lin MY, Yen CL, Chen SH. Management of lactose maldigestion by consuming milk containing lactobacilli. Digestive Diseases & Sciences 1998; 43:133-137.
(18.) Savaiano DA, AbouEIAnouar A, Smith DE, Levitt MD. Lactose malabsorption from yogurt, pasteurized yogurt, sweet acidophilus milk and cultured milk in lactase-deficient individuals. Am J Clin Nut 1984; 40:1219-1223.
(19.) McDonough FE, Hitchins AD, Wrong NP, Wells P, Bodwell CE. Modification of Sweet acidophilus milk to improve utilization by lactose-intolerant persons. Am J Clin Nut 1987; 45:570-574.
(20.) Kim HS, Gilland SE. Lactobacillus acidophilus as a dietary adjunct to aid lactose digestion in humans. J Dairy Science 1983; 66:959-966.
(21.) Guyatt G, Sackett D, Adachi J, et al. A clinicians guide for conducting randomised trials in individual patients. CMAJ 1988; 139:497.
(22.) Ramirez FC, Lee K, Graham DY. All lactase preparations are not the same: results of a prospective, randomized, placebo-controlled trial. Am J Gastroenterol 1994; 89:566-570.
FAST TRACK
Other strategies are available for lactose-intolerant persons: yogurt, lactase enzymes, and lactose-free products are all supported by evidence
FAST TRACK
Probiotics taken as supplements should adhere to the intestinal lining and digest dietary lactose, alleviating malabsorptive symptons
FAST TRACK
The hydrodgen breath test is the gold standard for diagnosing lactose intolerance
CORRESPONDING AUTHOR
Kara M. Levri, MD, MPH, UPMC St. Margaret, 3937 Butler Street, Pittsburgh, PA 15201. E-mail: k155882@aol.com.
Kara M. Levri, MD, MPH, Kari Ketvertis, MD, Mark Deramo, MD, Joel H. Merenstein, MD, and Frank D'Amico, PhD
University of Pittsburgh Medical Center/St. Margaret, Pittsburgh, Pa
COPYRIGHT 2005 Dowden Health Media, Inc.
COPYRIGHT 2005 Gale Group