Byline: I. Anand, J. Shah, S. Patel, C. Patel
Epilepsy is a neurological disorder characterized by excessive electrical discharge in brain, which causes seizures. The therapeutic strategy in countering epilepsy involves reducing neuronal excitability through different mechanistic pathways. Most therapeutics currently used in the treatment of epilepsy is either directed towards blocking voltage-gated sodium and calcium channels or potentiating gamma amino butyric acid (GABA)-mediated neurotransmission, with little focus on voltage-gated potassium ion channels, despite these channels having a major role in the control of all aspects of neuronal excitability. It is reported that functional impairment of potassium ion channels, either by mutation or inhibition, results in epilepsy.[1]
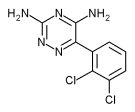
Retigabine (D23129), N-[2-amino-4-(4-fluorobenzylamino) phenyl] carbamic acid ethyl ester is a close structural analog of the centrally acting analgesic flupitrine. It is a purple colored compound with a molecular weight of 376.23, calc log P of 2.0 and a pKa of 10.8 (calculated as free base). Retigabine dihydrochloride appears to be hygroscopic, as medium to long-term storage at 18 [degrees]C (with presumed freeze-thawing) produces significant amounts of ring-closed product 5-(4-fluoro-benzylamino)-1,3-dihydro-benzimidazol-2-one and small amounts of uncharacterized oxidized products. Therefore, it is preferably stored as the free base, isolated from light.[2]
Retigabine has a novel mechanism of action that involves opening of neuronal Kv7.2-7.5 (formerly KCNQ2-5) voltage activated K+ channels. These channels (primarily Kv7.2/7.3) enable generation of the M-current, a sub-threshold K+ current that serves to stabilize the membrane potential and control neuronal excitability.[3] In addition to acting on potassium ion channels, retigabine also affects GABA neurotransmission in the GABAA receptor, which is a key inhibitory receptor in the central nervous system and is implicated in epilepsy.[4] Malfunctioning of the GABAA receptor leads to hyperexcitability in the brain, which causes seizures, making this receptor an important target for antiepileptic therapeutics. Apart from increasing the concentration of GABA in the brain (by either enhancing GABA synthesis or blocking GABA metabolism), retigabine allosterically potentiates GABA-induced current in rat cortical neurons in a concentration-dependent manner.[4] Numerous studies have demonstrated that retigabine is effective in a broad spectrum of in vivo epilepsy and seizure models. Retigabine was shown to be active (ED<sub>50</sub> range = 4.0-18.6 mg/kg, i.p.) against electrically induced seizures and against chemical seizures induced by pentylenetetrazole, picrotoxin and NMDA in mice.[5] Retigabine was also reported to attenuate sound-induced seizures in DBA/2 mice, a model of genetic epilepsy.[5] In the full amygdala-kindling model of complex partial seizures in rats, retigabine, at 0.01 to 5 mg/kg, i.p., has been reported to dose dependently increase the threshold current for induction of after discharges. Following stimulation with the after discharge threshold current, retigabine (5 mg/kg, i.p.) also reduced other seizure measures including seizure severity, seizure duration, total duration of behavioral changes and of changes after discharge.[6]
A number of recent studies have reported that retigabine can relieve pain-like behaviors in animal models of neuropathic pain. [7],[8],[9] Some animal experiments using mouse have shown that retigabine (1-10 mg/kg, i.p.) can dose dependently reduce anxiety-like behaviour.[10], [11]
Retigabine is rapidly absorbed and distributed, with an oral bioavailability of 60% and a high volume of distribution of approximately 6.2 L/kg.[12] Plasma protein binding of the drug is approximately 80%. The relatively high systemic bioavailability after oral administration suggests that retigabine is resistant to first-pass metabolism, a finding confirmed in multiple species. Retigabine is metabolized exclusively via phase II hepatic glucurodination and acetylation.[13], [14] In clinical multiple oral-dosing studies, it has been demonstrated that retigabine reaches steady state on the third day of dosing.[15] Relative exposure appears to be dependent upon the dose administered, but does not exhibit accumulation. Plasma retigabine rises following zero-order kinetics, and decays following first-order process. Gender differences in exposure have been noted with female subjects exhibiting higher plasma concentrations of the drug after single oral administration (200 mg) than male subjects.[12] Excretion of retigabine appears to be predominantly renal. In humans, 84% of an administered dose of [[14]C] retigabine is recovered in urine either as unchanged parent drug, N-glucuronides of retigabine, or in acetylated form.[16]
After oral administration in rats retigabine shows a therapeutic index of 28.8, which compares favorably with that reported for other antiepileptics, such as carbamazepine.[17] Only limited published data are available for retigabine in humans. Human studies suggest that retigabine is not associated with tolerance, dependence, or withdrawal liability. Tolerability was reported to be good when retigabine was titrated-up to its effective dose range (600-1200 mg/day).[16] In fixed-dose healthy volunteer studies, 500 mg appeared to be the maximum tolerated dose (MTD), although it is known that the MTD in epileptic patients is considerably higher. In up-titrated volunteers, 700 mg per day retigabine was tolerated without any dose-limiting adverse events.[15] Adverse events for both fixed-dose and up-titrated dosing of retigabine were found to be similar and included mild dizziness, headache, asthenia, nausea, and somnolence. At doses greater than the MTD, retigabine was associated with chills, pain, symptomatic hypotension, myalgia, sweating and vomiting.[15]
Retigabine has successfully completed Phase II clinical trial with the FDA for the treatment of epilepsy.[18]
As compared to other antiepileptic agents, retigabine is unique in that it selectively activates potassium ion channels Kv 7.2-Kv7.5 and not cardiac Kv 7.1, thereby avoiding cardiac side effects.[19] The antiepileptics, as a drug class, are routinely used in the treatment of a number of disease states in addition to epilepsy. Retigabine is highly efficacious in a broad-spectrum of in vivo epilepsy and seizure models. A comparison of antiepileptic form activity of retigabine with that of conventional anticonvulsants in in vitro models suggests that retigabine is especially likely to be useful in the treatment of pharmacoresistant epilepsy. Retigabine clearly attenuates pain-like behaviors in various animal models of neuropathic pain; it may also prove to be useful in treatment of clinical anxiety disorders. Clinical data obtained thus far indicate that retigabine is well tolerated in humans when titrated up to its therapeutic dose range. No tolerance, drug dependence, or withdrawal liability has been reported. Thus, retigabine may prove to be useful in the treatment of a diverse range of disease states in which neuronal hyperexcitability is a common underlying factor.
References
1. Rundfeldt C. The new anticonvulsant retigabine (D-23129) acts as an opener of K+ channels in neuronal cells. Eur J Clin Pharmacol 1997;336:243-249.
2. Meisel P, Landgraf K-F, Schafer J, Thiel W, Rischer W, Olbrich A, et al . US Patent (5,914,425) 1999.
3. Wuttke T, Seebohm G, Bail S, Maljevic S, Lerche H. The new anticonvulsant Retigabine favors voltage-dependent opening of Kv7.2(KCNQ2) channel by binding to its activation gate. Mol Pharmacol 2005;67:1009-17.
4. Rundfelt C, Netzer R. Investigations into mechanism of action of new anticonvulsant. Interaction with GABAergic and glutamatergic neurotransmission and with voltage gated ion channels. Arzneimittelforschung 2000;50:1063-70.
5. Rostock A, Tober C, Rundfeldt C, Bartsch R, Engel J, Emanuele E, et al . D-23129: a new anticonvulsant with a broad spectrum activity in animal models of epileptic seizures. Epilepsy Res 1996;23:211-23.
6. Tober C, Rostock A, Rundfeldt C, Bartsh R. D-23129: A potent anticonvulsant in the amygdala kindling model of complex partial seizures. Eur J Pharmacol 1996;303:163-9.
7. Blackburn-Munro G, Skaning Jensen B. The anticonvulsant retigabine attenuates nociceptive behaviours in animal models of persistent and neuropathic pain. Eur J Pharmacol 2003;460:109-16.
8. Dost R, Rostock A, Rundfeldt C. The anti-hyperalgesic activity of retigabine is mediated by KCNQ potassium channel activation. Naunyn Schmiedeberds Arch Pharmacol 2004;369:382-90.
9. Nielsen AN, Mathiesen C, Blackburn-Munro G. Pharmacological characterization of acid-induced muscle allodynia in rats. Eur J Pharmacol 2004;487:93-103.
10. Njung'e K, Handley SL. Evaluation of marble-burying behaviour as a model of anxiety. Pharmacol Biochem Behav 1991;38:63-7.
11. Shepherd JK, Grewal SS, Fletcher A, Bill DJ, Dourish CT. Behavioural and pharmacological characterization of the elevated 'zero-maze' as an animal model of anxiety. Psychopharmacology 1994;116:56-64.
12. Hermann R, Ferron GM, Erb K, Knebel N, Ruus P, Paul J, et al . Effects of age and sex on the disposition of retigabine. Clin Pharmacol Ther 2003;73:61-70.
13. Hempel R, Schupke H, McNeilly PJ, Heinecke K, Kronbach C, Grunwald C, et al . Metabolism of retigabine (D-23129), a novel anticonvulsant. Drug Metab Dispos 1999;27:613-22.
14. McNrilly PJ, Torchin CD, Anderson LW, Kapetanovic IM, Kupferberg JH, Strong JM. In vitro glucuronidation of D-2319, a new anticonvulsant, by human liver microsomes and liver slices. Xenobiotica 1997;27:431-41.
15. Friedel HA, Fitton A. Flupitrine. A review of its pharmacological properties and therapeutic efficacy in pain states. Drugs 1993;45:548-69.
16. Hermann R, Knebel NG, Neibch G, Richards L, Borlak J, Locher M. Pharmacokinetic interaction between retigabine and lamotrigine in healthy subjects. Eur J Clin Pharmacol 2003;58:795-802.
17. De Sarro G, Di Paola ED, Conte G, Pasculli MP, De Sarro A. Influence of retigabine on the anticonvulsant activity of some antiepileptic drugs against audiogenic seizures in DBA/2 mice. Naunyn Schmiedebergs Arch Pharmacol 2001;363:330-6.
18. Ferron GM, Paul J, Fruncillo R, Richards L, Knebel N, Gesty J, et al . Multiple-dose, linear, dose-proportional pharmacokinetics of retigabine in healthy volunteers. J Clin Pharmacol 2002;42:175-182.
19. Wuttke T, Seebohm G, Bail S, Maljevic S, Lerche H. The new anticonvulsant retigabine favors voltage-dependent opening of Kv7.2(KCNQ2) channel by binding to its activation gate. Mol Pharmacol 2005;67:1009-17.
COPYRIGHT 2005 Medknow Publications
COPYRIGHT 2005 Gale Group