ABSTRACT. Background: Branched-chain amino acids (BCAA; valine, leucine, and isoleucine) have a regulatory effect on protein metabolism and are the main donor for synthesis of alanine and glutamine in the skeletal muscle. This study was performed to investigate whether exogenous alanine or glutamine would affect leucine and protein metabolism in intact and endotoxemic rats. Methods: Rats were injected with endotoxin of Salmonella enteritidis or saline. Thirty minutes later, the effects of endotoxemia and L-alanyl-L-glutamine (AG) on leucine and protein metabolism were evaluated using a primed constant infusion of [1-14C]leucine, endotoxin, and AG (200 mg/mL) solution or an infusion of [1-^sup 14^C]leucine without endotoxin or AG. The specificity of the effect of exogenous alanine and glutamine was evaluated by a single infusion of alanine, glutamine, and glycine in a separate study. Results: Endotoxin treatment induced
more negative net protein balance caused mainly by an increase in whole-body proteolysis. Protein synthesis increased in kidneys, colon, and spleen, while a decrease was observed in skeletal muscle. The impressive effects of AG were the decrease in plasma branched-chain amino acid (BCAA) levels, decrease in leucine oxidized fraction, and improvement of protein balance associated with a decrease in whole-body proteolysis. Similar changes in leucine and protein metabolism were induced by infusion of alanine or glutamine but not by infusion of glycine. Conclusions: IV administration of alanine or glutamine improves protein balance and decreases leucine oxidized fraction in postabsorptive state and in endotoxemia. Decreased proteolysis is the main cause of decreased plasma BCAA levels after AG treatment. (Journal of Parenteral and Enteral Nutrition 24:215-222, 2000)
The systemic inflammatory response syndrome (SIRS), which is a result of the host response to severe infection, trauma, cancer, or thermal injury, is associated with skeletal muscle proteolysis and an increased release of amino acids into the bloodstream.1 The principal mediators are cytokines, primarily tumor necrosis factor-alpha (TNF-alpha), interleukin-1, and interleukin-6, synthesized by various cells of the body.2 The increased release of amino acids from skeletal muscle in SIRS appears to be a response that enables stimulated cell division, (eg, white blood cells, fibroblasts, and enterocytes) and a prompt production of acute phase proteins, immunoglobulins and other biologically active compounds. This response is often essential for survival. However, the activated proteolysis of muscle tissue may be disastrous if it is excessive or continues for a long time.
Alanine and glutamine are amino acids released from skeletal muscle in much higher quantities than other amino acids. They provide a number of essential functions particularly in stress situations. Alanine is an important substrate for gluconeogenesis. In addition to its role in acid-base homeostasis and in gluconeogenesis, glutamine is an important energy source and precursor for nucleotide synthesis in the gut mucosa and the immune system.3 The activated utilization of glutamine in SIRS often exceeds its synthesis in skeletal muscle resulting in a decrease of glutamine levels in plasma and tissues.4
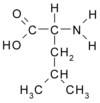
The main nitrogen donor for the synthesis of both glutamine and alanine in skeletal muscle is branched-chain amino acids (BCAA; valine, leucine, and isoleucine) (Fig. 1), which are known to have a regulatory effect on protein turnover.5,6 The increased demands for BCAA caused by SIRS are met by the activated breakdown of proteins in skeletal muscle, and it can be proposed that alanine or glutamine supplementation significantly affects both BCAA and protein metabolism.
The aim of the present studies was, therefore, to investigate whether exogenous alanine and glutamine would affect leucine and protein metabolism in intact and endotoxemic rats. Because glutamine is unstable and its solubility is poor, the stabile dipeptide L-alanyl-- L-glutamine (AG) is used in clinical practice. IV supplied AG is rapidly and efficiently hydrolyzed to alanine and glutamine.7 Hence, the fundamental part of our experiments was performed by using AG. To clarify the specificity of the effect of exogenous alanine and glutamine, we evaluated the effects of a single infusion of alanine, glutamine, and glycine in a separate study.
MATERIALS AND METHODS
Animals
Male Wistar rats (Velaz, Prague, CZ) weighing 200 to 235 g were housed in standardized cages in quarter with controlled temperature and a 12-hour light-dark cycle and received Velaz-Altromin 1320 laboratory chow and drinking water ad libitum. All procedures involving animals were performed according to guidelines set by the Institutional Animal Use and Care Committee of Charles University.
Materials
L-[1-^sup 14^C]leucine was purchased from Amersham (Buckinghamshire, United Kingdom), [^sup 14^C]bicarbonate was obtained from Du Pont-NEN (Bad Homburg, Germany). Leucine, alanine, glutamine, glycine, and lipopolysaccharide (LPS) from Salmonella enteritidis, Folin-Ciocalteu phenol reagent, and albumin were purchased from Sigma (St. Louis, MO). Hyamine hydroxide was obtained from Packard Instrument (Meriden, CT). AG was obtained from Ajinomoto (Tokyo, Japan). The remaining chemicals were from Lachema (Brno, CZ).
Experimental Design
A polyethylene cannula was inserted into the jugular vein under light diethyl ether narcosis 24 hours before the beginning of the experiment to exclude the effect of stress from surgery. To exclude nutritional effects, all rats were fasted overnight before the experiment. Two separate studies were performed.
Study 1. The experiments were started by injecting LPS (2 mg/kg body weight intraperitoneally) or saline (control) between 7 and 8 nM. Each animal was then placed in a glass metabolic cage. After 30 minutes, rats were infused with L-[1-^sup 14^C]leucine (1.9 (mu)Ci/mL), LPS (0.1 mg/mL), and AG (200 mg/mL) solution or L-[1-^sup 14^C]leucine solution without LPS or AG. Thus, we had four groups of animals as follows: (1) control; (2) control plus AG; (3) LPS, and (4) LPS plus AG. The solutions were not supplemented by amino acids so as to be isonitrogenous because the supply of different amounts of particular amino acids would significantly influence both leucine and protein turnover and amino acid concentrations in body fluids. A priming dose of 0.7 mL (ie, 1.33 (mu)Ci of L-[1- ^sup 14^C]leucine) was followed by a constant infusion at a rate of 0.36 mL/h for 200 minutes. The rats were killed by exsanguination via the abdominal aorta exactly at the 201st min from the beginning of the infusion. Afterwards, the liver, gastrocnemius muscle, spleen, kidney, small intestine, colon, lungs, and heart were quickly removed and immediately frozen in liquid nitrogen. The dose of endotoxin and the time of death were based on data from Nawabi et al,8 who observed marked activation of branched-chain keto acid dehydrogenase (BCKAD) in rats treated with this dose of endotoxin at 4 and 6 hours postinjection. The dose of AG used in this study showed the maximal effect on changes in proteolysis in our preliminary dose-response studies.
Study 2. Rats were infused with L-[1-^sup 14^C]leucine (1.9 (mu)Ci/mL) and L-alanine (0.5 mmol) solution, [1-^sup 14^C]leucine and L-glutamine (0.5 mmol) solution, [1-^sup 14^C]leucine and glycine (0.5 mmol) solution, or [1-^sup 14^C]leucine in saline. A priming dose of 0.7 mL [1-^sup 14^C]leucine was followed by a constant infusion at a rate of 0.36 mL/h as in study 1. The rats were killed by exsanguination at the 201st min of the infusion.
Parameters of Leucine Metabolism
Whole-body leucine metabolism was considered to take place within a common metabolic pool, represented by free plasma leucine. Due to the fact that exogenous leucine intake (E) was zero in our protocol, Q estimates the leucine released from protein, ie, the protein breakdown (B), and D estimates net protein balance as described by the equation: Q = In + D = B + E. Using this formula, rates of leucine incorporation into protein (In) and the oxidized fraction of leucine (OF = D 100/Q) were calculated.
It has been suggested that the plasma enrichment of alpha-keto-isocaproic acid reflects intracellular leucine enrichment and may be more relevant for measurement of protein metabolism than plasma leucine enrichment.11 However, it has been shown that plasma KIC enrichment to leucine enrichment was constant (0.75-0.85) after a number of experimental maneuvers and no qualitative differences were observed, whether the ^sup 14^C-KIC or ^sup 14^C-Leu enrichments were used to calculate parameters of leucine turnover.12 Hence, either leucine or KIC enrichment can be used for measurement of leucine turnover.
Tissue Protein Synthesis and Protein Content
The samples for measurement of protein synthesis were processed as described elsewhere.10 The fractional protein synthesis rates were calculated by using the equation derived by Garlick et al13 and expressed as the fraction of protein mass renewed each day, in percent per day (Ks). Protein content was measured according to Lowry et al.14
Amino Acids
Amino acid concentrations in deproteinized samples of blood plasma or tissues were determined with highperformance liquid chromatography (Waters, Milford, MA) after precolumn derivatization with omicron-phthaldialdehyde. The radioactivity of the samples was measured with the liquid scintillation radioactivity counter LS 6000 (Beckman Instruments, Fullerton, CA).
Statistical Analysis
Results are expressed as the mean +/- SE. An analysis of variance was used for analysis of data (approximate F-tests using the method of unweighted means). The control group was compared with all of the other means ([k-1] comparisons for k groups) by Bonferroni (vs control) multiple comparison procedure at 0.05 significant level. Statistical software NCSS60 was used for the analysis.
RESULTS
LPS-treated rats showed symptoms of acute illness such as lethargy, piloerection, and diarrhea within 2 hours after LPS injection. This model of endotoxemia is associated with the significant increase in TNF-alpha and triglyceride concentrations and a decrease in platelet numbers in blood.10,15 There were no differences in body weights or in weights of liver, jejunum, and heart between particular groups of animals. However, in LPS-treated animals, significantly higher weights of kidneys, spleen, and lungs were observed.
Whole-Body Leucine and Protein Metabolism
Significantly more negative net protein balance in LPS-treated animals was caused mainly by a significant increase in proteolysis and not a decrease in protein synthesis (Table I). In LPS-treated animals, AG treatment caused a significant decrease both in proteolysis and protein synthesis, an improvement of protein balance, and a decrease in leucine oxidized fraction. The decrease in proteolysis after AG was also observed in the intact animals. A significant decrease was found in all the estimated parameters of leucine and protein metabolism after AG treatment, when all AG-treated rats were analyzed as one group regardless of LPS treatment.
Protein Synthesis in Specific Tissues
LPS treatment caused a significant decrease in protein synthesis in skeletal muscle while an increase was observed in the fractional rates of protein synthesis in the kidneys and colon (Table II). AG treatment had no effect on protein synthesis in control animals. However, AG caused a significant increase in protein synthesis in the lungs of endotoxemic rats. Comparison of LPS- and AG-treated rats with the appropriate groups showed that LPS also activated protein synthesis in the spleen and AG treatment caused a decrease in the synthesis of blood plasma proteins.
Amino Acids in Blood Plasma
We did not observe a significant effect of LPS on the plasma amino acid levels in this study (Table III). AG treatment caused a significant increase in alanine and glutamine levels and a marked decrease in the concentration of most individual amino acids.
Amino Acids in Tissues
We did not observe an obvious effect of LPS treatment on the tissue levels of individual amino acids with the exception of the jejunum, where a significant decrease in glutamine (Gln) concentration was detected (Table IV). AG treatment corrected the decreased Gln levels in the jejunum of LPS animals and caused an increase in alanine or glutamine concentrations in several tissues of both intact and endotoxemic rats.
Effect of Glycine, Alanine, and Glutamine on Leucine and Protein Metabolism
Alanine or glutamine infusion caused a decrease in proteolysis, protein synthesis, and an improvement in protein balance (Table V). The decrease in leucine oxidized fraction and plasma leucine concentration was insignificant. The changes in estimated parameters of leucine metabolism demonstrated in alanine or glutamine infused animals were not observed in animals infused with glycine.
DISCUSSION
There are differences in distribution in BCAA transaminase and BCKAD in rat and humans and the results should be interpreted cautiously. The main dif ference is in the activity of BCKAD. Human muscle contains 60% of the total body BCKAD, while rat muscle contains 10% to 30%. However, this is mainly because the activity of BCKAD in human liver is low, not because that in muscle is high and BCKAD are released in significant amount to the bloodstream both from human and rat muscle.4 We believe that there are no qualitative differences in BCAA catabolism in humans and rats and that the results obtained using the rat model provide a valid idea about the changes in BCAA and protein metabolism in humans. The most important data obtained are summarized in a hypothetical scheme (Fig. 3). Because the metabolic functions and initial steps in catabolism of BCAA are similar, the changes in leucine turnover also estimate the fate of the other BCAA.
The observed changes in leucine and protein metabolism induced by LPS administration, particularly an increase in leucine appearance from protein breakdown and oxidation, ie, increased proteolysis and impaired protein balance, are consistent with our previous studies.10,16 The main cause of increased leucine oxidation in endotoxemia is undoubtedly the increased activity in muscle BCKAD, the rate-limiting enzyme in the pathway of BCAA catabolism in skeletal muscles Increased activity of BCKAD after LPS or cytokine treatment was demonstrated in skeletal muscle in several studies.8,16 However, a decrease in BCKAD activity was observed in the liver after LPS or TNF-alpha treatment.10 It may be suggested that the marked increase of BCAA oxidation in skeletal muscle and release of amino acids into the bloodstream in endotoxemia are related both to the increased proteolysis and decreased synthesis of skeletal muscle proteins. Enhanced mobilization of amino acids from the protein mass enables the body to cover the increased demands of several tissues in which protein synthesis is activated. A significant increase in protein synthesis after LPS treatment was observed in the kidneys, colon and spleen in this study. In other studies, an increase in protein synthesis after LPS treatments was also observed in liver, small intestine, and blood plasma.10,17 Although enhanced synthesis of acute phase proteins in SIRS is activated,18 the unaffected hepatic synthesis of plasma proteins was observed in the present study. This is probably caused by decreased synthesis of albumin.19 Because the time course of our experiment was short, the absence of an overall effect of LPS on plasma protein synthesis may also be explained by a lag period necessary for transport of proteins from hepatic tissue to the blood.
The needs of the body for BCAA are, particularly in the postabsorptive state, covered by activated proteolysis.5 This phenomenon makes it difficult to demonstrate the lack of BCAA in organisms with SIRS. We assume the opinion that there is no lack of BCAA in stress states, which is usually based on unchanged tissue BCAA levels, is misleading. The ratio between BCAA input from proteolysis and output by utilization in protein synthesis and oxidation can be easily affected. For this reason the data describing changes in the concentrations of BCAA in body fluids in sepsis, trauma, or after endotoxin treatment are inconsistent, and decreased, unchanged, and increased levels are demonstrated.8,10,20
Alanine and glutamine have important physiologic functions and their activated synthesis and utilization is a characteristic of SIRS. Several studies have demonstrated that the main source of nitrogen for synthesis of alanine and glutamine are BCAA.5,6,21,22 Above all, the BCAA are the main source of nitrogen for synthesis of glutamate from cx-ketoglutarate and the carbon chain of glutamine can be derived from BCAA.23 However, increased demands for glutamine and alanine in SIRS cause mainly lack of glutamine while alanine level in body fluids is usually maintained in physiologic ranges. Nevertheless, considering that the synthesis of both alanine and glutamine requires nitrogen of BCAA and that increased synthesis of alanine and glutamine in SIRS is closely related to the activated breakdown of lean muscle tissue,24 it can be suggested that simultaneous administration of alanine or glutamine is a rational method preventing accelerated BCAA catabolism and muscle wasting in SIRS.
The results of this study clearly demonstrate that exogenous AG can prevent loss of body proteins and that this effect is caused mainly by decreased proteolysis that is associated with decreased oxidation of BCAA. Similar changes in leucine and protein metabolism were also induced, although in lesser degree, by the infusion of glutamine or by alanine, but not by the infusion of glycine. Thus, the observed effect of AG infusion seems to be specific for alanine and glutamine although similar effect of other amino acids cannot be excluded. The observed inhibitory effect of AG on protein breakdown may be the explanation for the beneficial effect of AG or exogenous glutamine on nitrogen balance and the outcome of disease in stressed patients.3,24,25-27
The unchanged glutamine levels in several tissues after AG infusion are undoubtedly caused by the decrease in glutamine synthesis after AG administration.24 This negative feedback regulating de novo glutamine synthesis is further evidence that changes in BCAA and protein metabolism induced by AG infusion are related to changes in endogenous synthesis of glutamine and alanine.
Another exciting observation is the decrease in blood plasma BCAA levels after AG treatment in the LPS-- treated animals. Considering that after AG administration a decrease in leucine oxidation and incorporation in proteins was observed, the main cause of the decreased BCAA and some other amino acids in blood plasma should be a lower rate of release of amino acids from protein breakdown. Another possibility is the influence of AG, or alanine or glutamine on amino acid transport across cell membranes. However, this explanation is unlikely as a significant increase in the BCAA concentration after AG treatment was observed only in the lungs of LPS-treated rats. We do not have a clear explanation for the marked decrease in the concentration of certain amino acids (particularly glycine, tyrosine, and lysine) in blood plasma after AG infusion. Several mechanisms including the influence of AG on catabolism, protein synthesis, and transport across the cell membrane can be involved.
The possible cause of the decreased rate of protein synthesis after AG administration is the observed decrease in plasma amino acid concentration, probably caused by decreased protein breakdown. It should be noted that the observed effects of AG on leucine and protein metabolism were demonstrated in the postabsorptive state. Thus, it can be suggested that the provision of AG together with other nutrients should significantly affect plasma amino acid levels, secretion of several hormones, and the effect of AG on protein turnover, particularly on protein synthesis. The stimulatory effect of the amino acid solution enriched with AG on protein synthesis has been demonstrated in several studies.25,27,28
In conclusion, the obtained results clearly demonstrate that IV administration of AG markedly improves protein balance in endotoxemic rats. The improvement of protein balance is associated with decreased protein breakdown and leucine oxidized fraction.
ACKNOWLEDGMENTS
The study was supported by a grant from the Internal Grant Agency of Ministry of Health of the Czech Republic (no. 3772-3). We are grateful for the technical support of I. Altmannova, J. Hofmanova, L. Kriesfalusyova, R. Rysava and I. Sprinarova. Many thanks to Connie Bennett, BSN (Anchorage, AK) for proof reading.
REFERENCES
1. Hasselgren, PO, Talamini M, James JH, et al: Fischer. Protein metabolism in different types of skeletal muscle during early and late sepsis in rats. Arch Surg 121:918-923, 1986
2. Goodman MN: Interleukin-6 induces skeletal muscle protein breakdown in rats. Proc Soc Exp Biol Med 205:182-185, 1994
3. Ziegler TR: Glutamine supplementation in catabolic illness. Am J Clin Nutr 64:645-647, 1996
4. Smith RJ, Wilmore WW: Glutamine nutrition and requirements. JPEN 14(Suppl ):94-99, 1990
5. Darmaun D, Dechelotte P: Role of leucine as a precursor of glutamine alpha-amino nitrogen in vivo in humans. Am J Physiol 260:E326-329. 1991
6. Harper AE, Miller RH, Block KP: Branched-chain amino acid metabolism. Annu Rev Nutr 4:409-454, 1984
7. Stehle P, Ratz I, Furst P: In vivo utilization of intravenously supplied L-alanyl-L-glutamine in various tissues of the rat. Nutrition 5:411-415, 1989
8. Nawabi MD, Block KP, Chakrabarti MC, et al: Administration of endotoxin, tumor necrosis factor, or interleukin 1 to rats activates skeletal muscle branched-chain a-keto acid dehydrogenase. J Clin Invest 85:256-263, 1990
9. Holecek M, Tiller I, Skopec F, et al: Leucine metabolism in rats with cirrhosis. J Hepatol 24:209-216, 1996
10. Holecek M, Sprongl L, Skopec F, et al: Leucine metabolism in TNF-alpha- and endotoxin-treated rats: Contribution of hepatic tissue. Am J Physiol 273:E1052-1058, 1997
11. Matthews DE, Schwarz HP, Yang RD, et al: Relationship of plasma leucine and alpha-ketoisocaproate during a L-[1-13C]leucine infusion in man: A method for measuring human intracellular leucine tracer enrichment. Metab Clin Exp 31:1105-1112, 1982
12. Petrides AS, Luzi L, DeFronzo RA: Time-dependent regulation by insulin of leucine metabolism in young healthy adults. Am J Physiol 267:E361-368, 1994
13. Garlick PJ, Millward DJ, James WPT: The diurnal response of muscle and liver protein synthesis in vivo in meal-fed rats. Biochem J 136:935-945, 1973
14. Lowry OH, Rosebrough NJ, Farr AL, et al: Protein measurement with the Folin phenol reagent. J Biol Chem 193:265-275, 1951
15. Holecek M, Sprongl L, Tichy M, et al: Leucine metabolism in rat liver after a bolus injection of endotoxin. Metabolism 47:681-- 685, 1998
16. Holecek M: Leucine metabolism in fasted and tumor necrosis factor treated rats. Clin Nutr 15:91-93, 1996
17. Wang Q, Fischer JE, Hasselgren PO: Treatment of endotoxemic mice with anti-interleukin-6 antibody paradoxically increases interleukin-6 levels and stimulates mucosal protein synthesis. Arch Surg 132:82-88, 1997
18. Rosenblatt S, Clowes GHA, George BC, et al: Exchange of amino acids by muscle and liver in sepsis. Arch Surg 118:167-175, 1983
19. Pepys MB, Baltz MI: Acute phase protein with special reference to C-reactive protein and related proteins (Pentaxins) and serum amyloid A protein. Adv Immunol 34:141-212, 1983
20. Holecek M, Skopec F, Sprongl L; et al: Protein metabolism in specific tissues of endotoxin-treated rats. Physiol Res 44:399-- 406, 1995
21. Ardawi MS, Newsholme EA: Metabolism in lymphocytes and its importance in the immune response. Essays Biochem 21:1-44, 1985
22. Snell K: Muscle alanine synthesis and hepatic gluconeogenesis. Biochem Soc Trans 8:205-213, 1980
23. Yoshida S, Lanza-Jacoby S, Stein TP: Leucine and glutamine metabolism in septic rats. Biochem J 276:405-409, 1991
24. Hickson RC, Wegrzyn LE, Osborne DF, et al: Alanyl-glutamine prevents muscle atrophy and glutamine synthetase induction by glucocorticoids. Am J Physiol 271:81165-1172, 1996
25. Hammarqvist, F, Wernerman J, Ali R, et al: Addition of glutamine to total parenteral nutrition (TPN) after elective abdominal surgery spares free glutamine in muscle, counteracts the fall in muscle protein synthesis, and improves nitrogen balance. Ann Sure 209:455-461. 1989
26. Morlion BJ, Stehle P, Wachtler P, et al: TPN with glutamine dipeptide after major abdominal surgery: A randomized, doubleblind, controlled study. Ann Surg 227:302-308, 1998
27. Ziegler TR, Szeszycki EE, Estivariz CF, et al: Glutamine: from basic science to clinical applications. Nutrition 12:568-- 70, 1996
28. Vinnars E, Hammarqvist F, von der Decken A, et al: Role of glutamine and its analogs in posttraumatic muscle protein and amino acid metabolism. JPEN 14(suppl 4):125-129, 1990
Milan Holecek, MD*; Frantisek Skopec, PhD^; Hana Skalska, PhD^^; and Ludek Sprongl, PhD(sec)
From the *Department of Physiology and ^Radioisotope Laboratory, Charles University, School of Medicine, ^^Faculty of Management and Information Technology, and (sec)University Hospital Motol, Prague, Czech Republic
Received for publication, July 6, 1999.
Accepted for publication, November 16, 1999.
Correspondence and reprint requests: Milan Holecek, MD, Department of Physiology, Charles University School of Medicine, Simkova 870, 500 Ol Hradec Kralove, Czech Republic. Electronic mail may be sent to holecek@lfhk.cuni.cz
Copyright American Society for Parenteral and Enteral Nutrition Jul/Aug 2000
Provided by ProQuest Information and Learning Company. All rights Reserved


![Leucine Formula (Older Version [Note the diferences in the order of the elements in a molecule]) Leucine Formula (Older Version [Note the diferences in the order of the elements in a molecule])](pics/Leucine_3.png)
