We evaluated a 63-year-old woman who developed dyspnea with a sensation of chest tightness that was temporally associated with discharges from a vagus nerve stimulator that had been implanted for the control of intractable seizures. Spirometry demonstrated the development of significant airflow obstruction associated with the firing of the stimulator. Adjustment of the stimulator settings resolved the discharge-associated bronchoconstrictive phenomenon. These findings highlight an important association between vagus nerve stimulators and dyspnea that should be considered in the differential diagnosis of patients with these devices who present with dyspnea and/or chest tightness. The relative importance of vagal stimulation to bronchoconstriction is suggested by the findings.
Key words: bronchoconstriction; dyspnea; seizure; vagus nerve stimulator
**********
Vagus nerve stimulators are relatively new devices that are finding increased use in the nonpharmacologic management of seizure disorders. They are implanted in the subcutaneous tissues of the chest, with a wire lead inserted into the vagus nerve to deliver regularly timed cycles of electrical pulses that suppress epileptogenic foci. (1) We report a case in which a vagus nerve stimulator had the unintended effect of inducing dyspnea that was associated with the activation of the device, which was found to temporally correlate with bronchoconstriction as demonstrated by serial pulmonary function assessments. Nerve stimulator setting adjustments were found to alleviate the bronchoconstriction and associated dyspnea.
CASE PRESENTATION
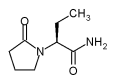
A 63-year-old, right-handed white woman with a 20-year history of psychomotor seizures with intractable features, despite management with levetiracetam and carbamazepine, underwent implantation of a vagus nerve stimulator (NeuroCybernetic Prosthesis System; Cyberonics, Inc; Houston, TX) on the left side in an uncomplicated procedure in October 2001. The unit was set to a frequency of 20 Hz, to 0.5 mA, to a 250-ms pulse width, and to a cycle of 30 s on, then 5 min off. She experienced an immediate reduction in the frequency and severity of her seizures. The patient had no history of asthma or other lung or cardiac diseases. Almost immediately after the device was turned on after implantation, she began to notice dyspnea at rest that was associated with central chest tightness that occurred in conjunction with the firing of the vagus nerve stimulator. She was referred for a pulmonary consultation for the evaluation of dyspnea. Her examination findings were unremarkable at baseline. A chest radiograph demonstrated clear lung fields and a normal cardiomediastinal silhouette. However, shortly after the firing of the nerve stimulator, wheezing and an increase in the expiratory phase of the respiratory cycle were noted on examination. Spirometry was performed several times during the asymptomatic phase between stimulator discharges and during the dyspneic phases coinciding with nerve stimulation, demonstrating normal baseline spirometry with subsequent significant and consistent transient impairment of expiratory airflow, particularly in the small airways (as reflected in the significant fall in the forced expiratory flow measured during expiration of 25 to 75% of the vital capacity), coinciding with nerve stimulator discharge. Separate pretreatments of the patient with either inhaled albuterol or ipratropium bromide failed to attenuate the patient's sensation of dyspnea or the increased airflow obstruction associated with the nerve stimulator discharge. Representative findings are shown in Table 1.
A neurology consultation was obtained with regard to altering the settings of the stimulator to see whether this would result in any improvement in her symptoms and the concomitant airflow reduction. The stimulator was reprogrammed to run at 10 Hz, a 500-ms pulse width, and at 0.75 mA, with other settings remaining unchanged. With this change in settings, the patient had complete resolution of the dyspnea and chest tightness associated with stimulator discharge, and spirometry performed during discharge no longer demonstrated any obstruction or decrement in airflow on repeated assessments (data not shown). She experienced breakthrough seizure symptoms on the new settings approximately 3 months later while still receiving the same dose of levetiracetam in conjunction with a lower dose of carbamazepine. The vagal stimulator then was adjusted to 1 mA with all other settings remaining unchanged. With this change in settings, dyspnea and chest tightness did not recur, and 9 months after adjustment of the settings of her nerve stimulator seizures remain well-controlled with a minor modification of the carbamazepine dose, which remains at a lower dose than that employed prior to the implantation of the vagus nerve stimulator.
DISCUSSION
We believe this to be the first report of dyspnea attributable to airflow obstruction that is temporally associated with a discharge of a vagus nerve stimulator. Reports of the unintended consequences of vagus nerve stimulators have included descriptions of voice change secondary to stimulation of the laryngeal nerve, (2) and dyspnea has been reported in up to 25.3% of patients with higher (ie, 30 Hz) vagus nerve stimulation compared with 10.7% of patients receiving lower (ie, 1 Hz) stimulation, (3) although previously this has not been linked specifically to bronchoconstriction and airflow obstruction. Our findings suggest an important role for the vagus nerve in determining airway constriction independent of other factors. Prior studies (4) have suggested the selective importance of vagus stimulation in the parasympathetic regulation of airway tone in humans. It is noteworthy that pretreatment with inhaled ipratropium bromide did not attenuate the fall in airflow with nerve stimulator discharge in our patient, suggesting that factors other than acetylcholine may be mediating the bronchoconstriction seen with vagus nerve stimulation. The identification of such factors may provide important insights into new pathways for the treatment of vagus nerve-mediated bronchoconstriction. Although further studies are needed to define these new pathways, an intriguing report (5) has indicated that vagally mediated nonadrenergic, noneholinergic excitatory innervation plays a role in allergen-induced bronchoconstriction. Neuroldnin-2 receptors were involved in this bronchoconstrictive process, which was blocked by specific inhibitors. (5)
CONCLUSIONS
Our findings confirm that vagus nerve stimulator-associated dyspnea may be corrected by reprogramming the settings of the stimulator, which in the case of our patient resolved the bronchoconstriction. As vagus nerve stimulators become more commonplace in the management of seizure disorders, an awareness of the association between their use and the presence of dyspnea with bronchoconstriction, as well as the potentially simple correction of this problem with stimulator reprogramming is needed. The unintended, but relatively pure, demonstration of significant airflow obstruction induced by vagal stimulation provides evidence of an important contribution of this nerve to airway tone.
REFERENCES
(1) McLachlan RS. Vagus nerve stimulation for intractable epilepsy: a review. J Clin Neurophysiol 1997; 14:358-368
(2) Ben-Menachem E. Vagus nerve stimulation, side effects, and long-term safety. J Clin Neurophysiol 2001; 18:415-418
(3) Schacter S. Vagus nerve stimulation therapy summary: five years after FDA approval. Neurology 2002; 59(suppl):S15-S20.
(4) Coleridge JCG, Coleridge HM. Afferent vagal C fibre innervation of the lungs and airways and its functional significance. Rev Physiol Biochem Pharmaeol 1984; 99:2-110
(5) Krishnakumar S, Holmes EP, Moore RM, et al. Non-adrenergic non-cholinergic excitatory innervation in the airways: role of neurokinin-2 receptors. Auton Autacoid Pharmacol 2002; 22:215-224
Jagdeep S. Bijwadia, MD, FCCP; Robert C. Hoch, MD, FCCP; and Donn D. Dexter, MD
* From the Departments of Pulmonary and Critical Care Medicine (Drs. Bijwadia and Hoeh) and Neurology (Dr. Dexter), Luther Midelfort/Mayo Health System, Eau Claire, WI. Manuscript received March 18, 2004; revision accepted July 13, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Jagdeep Bijwadia, MD, FCCP, Regions Hospital, 640 Jackson St, St. Paul, MN 55101; e-mail: jagdeep.s.bijwadia@healthpartners.com
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group