Background: A randomized trial was performed comparing azithromyein and levofloxacin for treating moderately to severely iii patients hospitalized with community-acquired pneumonia. This is a cost-minimization analysis comparing those regimens.
Methods: The cost-minimization analysis compares 81 patients receiving sequential therapy with IV azithromycin plus IV ceftriaxone followed by oral azithromycin with 82 patients receiving IV levofloxacin followed by oral levofloxacin, all with complete economic data over approximately 30 days, including information about hospitalization, study medications, home care, postdischarge utilization, and lost productivity. Units of utilization were multiplied by unit prices in order to estimate cost per patient. These total costs were compared using a two-sample t test.
Results: Direct medical costs of the azithromycin group were $2,481 less than the corresponding costs in the levofloxacin group (p = 0.03; 95% confidence interval, $238 to $4,724). Most of the cost difference ($2,300) is attributable to hospital days, with the majority of these days being spent on the general medicine wards. The precise magnitude of the cost advantage attributable to azithromycin, if any, depends on both the reduction in length of hospital stay and its associated daily cost.
Conclusions: Azithromycin was no more costly than levofloxacin, and perhaps less so. Cost is but one of many factors that should be considered by clinicians in decisions involving any individual patient.
Key words: azithromycin; community-acquired pneumonia; cost-minimization analysis; levofloxacin; randomized controlled trial
Abbreviations: CAP community-acquired pneumonia; CAP-IN = randomized trial comparing azithromycin and levofloxacin for treating moderately to severely ill patients hospitalized with community-acquired pneumonia; CPI = consumer price index; ED = emergency department; ICD-9-CM = Internatinal Classifications of Diseases, Ninth Revision, Clinical Modification: IQR = interquartile range: LOS = length of stay; OCCR operating cost-to-charge ratio
**********
Community-acquired pneumonia (CAP) is a serious public health problem accounting for 600,000 hospitalizations and $23 billion per year in the United States alone. (1) Treatment is usually empiric and directed against common pathogens such as Streptococcus pneumoniae and Haemophilus influenzae. Atypical pathogens, such as Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila, are not susceptible in vitro to [beta]-lactams and may account for 33% of CAP infections. (2)
Consistent with recommendations from professional societies, two of the most common approaches to empiric CAP therapy are as follows: (1) a [beta]-lactam/[beta]-lactamase inhibitor or second- or third-generation cephalosporin plus a macrolide; and (2) members of the fluoroquinolone class. The tradeoff is that while members of the quinolone class provide very broad coverage and have excellent oral bioavailability, these agents may also increase the risk that resistant organisms may develop. (3,4) The potential costs (in terms of morbidity, mortality, and economies) of an outbreak involving resistant organisms are extremely high.
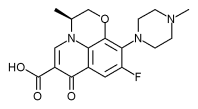
A randomized trial was completed comparing azithromycin and levofloxacin for treating moderately to severely ill patients hospitalized with community-acquired pneumonia (CAP-IN) (5) representing the strategies described above. In particular, CAP-IN compared the clinical efficacy of the following: (1) sequential therapy with IV azithromyein plus IV ceftriaxone followed by oral azithromycin, and (2) IV levofloxacin followed by oral levofloxacin in moderate to severely ill subjects with CAP requiring hospitalization and IV therapy. We present here a cost-minimization study comparing the two regimens, based on results from CAP-IN.
MATERIALS AND METHODS
CAP-IN
More specific details regarding CAP-IN study design and efficacy results are presented elsewhere. (5) Briefly, CAP-IN was an open-label, randomized trial comparing two regimens: azithromycin and levofloxacin. The azithromycin protocol specified IV azithromycin (500 mg qd) plus IV ceftriaxone (1 g qd) for 2 to 5 days followed by oral azithromycin (two 250-mg tablets qd) to complete a total of 7 to 10 days. The levofloxacin protocol specified IV levofloxacin (500 mg qd) for a minimum of 2 days followed by oral levofloxacin (500 mg qd) to complete a total of 7 to 14 days of therapy. For both regimens, the precise point at which IV therapy was shifted to oral therapy was based on clinical judgment, in particular on an assessment of the improvement in the patients' signs and symptoms (eg, temperature < 37.8[degrees]C for at least 8 h, cough and shortness of breath improving, oral intake and GI absorption adequate, and WBC count normalizing). The decision to discharge patients was similarly based on clinical judgment.
Assuming that the two regimes are equally efficacious, one would expect to see similar lengths of W therapy and of total hospital stay. Recognizing that this was an unblinded study, interpretation of data on the duration of these events critically depends on the assumption that physicians applied the above criteria identically for the two study groups.
All subjects were moderately to severely ill with CAP requiring hospitalization and IV therapy. Inclusion criteria included CAP with a Fine pneumonia severity index of at least 71 and at least one from a list of pneumonia signs and symptoms. Exclusion criteria included various serious illnesses, pregnancy, and intolerance to any of the main study medications.
The sample size for CAP-IN was based on demonstrating clinical equivalency between the two regimens. The trial was stopped early, width 110 patients in the azithromycin group and 102 patients in the levofloxacin group, at the point when clinical equivalency was demonstrated.
The inputs to the economic analysis utilized details about the hospitalization and information collected via interview at approximately 30 days after hospital admission. This latter interview included brief questions about symptom severity and functional status, as well as work days lost and self-reported medical utilization after the initial hospitalization. No information was available on recrudescent or residual pneumonias treated in either a hospital or outpatient setting after the conclusion of follow-up; the economic analysis assumes that the study groups are clinically similar at this point.
The number of patients available for the economic analysis (essentially, for whom a final 30-day interview was present) was 163:81 patients from the azithromycin group and 82 patients from the levofloxacin group. The status of the 49 patients not included in the economic analysis was as follows: 4 died; 7 were withdrawn from the study due to an insufficient clinical response; 11 were withdrawn from the study due to adverse events; 4 were withdrawn from the study due to laboratory abnormalities; 7 had protocol violations; 6 were unavailable for follow-up; 3 withdrew consent; and 7 were dropped for other reasons. The distribution of these subjects by treatment group was comparable.
Economic Analysis
Data available for the economic analysis are as follows: (1) dosage of the various drugs; (2) hospital days and location (general medical ward, ICU, other) during the hospital stay; (3) number of work days lost; (4) home care (number of days, provider); and (5) postdischarge utilization (outpatient visit, emergency department [ED], physician office), the latter three items being based on patient report at the final interview. The intent of collecting these data elements was not necessarily to impose on the trial participants the burden of obtaining every possible component of cost during the mouth following hospital admission for CAP, but instead was to focus on those elements that might either be associated with large costs or be differentially distributed across the groups. For example, no attempt was made to record details of individual hospital stays in sufficient detail to support a microcosting exercise.
The primary outcome variable is the estimated direct medical cost during the (approximately) 30-day follow-up period of CAP-IN. In addition, indirect costs were estimated based on reported work days missed. The main analysis is based on recording relevant aspects of health-care utilization during this 30-day period; assigning prices to each of these elements of utilization in order to obtain estimated costs by category: summing these estimated costs for each patient; and then using these patient-level costs as the inputs into a comparison between azithromycin and levofloxacin. This approach is intended to approximate the societal perspective.
Table 1 presents the unit prices assigned to each of the above elements of utilization. Details regarding the derivation of these unit prices are provided in the Appendix. Briefly, in generating the above unit prices, drug costs included cost per dose plus the cost for preparation and administration, these latter costs being based on averaging results from various microcosting studies. Costs per hospital day, disaggregated by location within the hospital, were based on a study of a group of patients with CAP similar to the current trial, in conjunction with information from Medicare. Lost productivity was based on an average national wage rate. Home care costs for skilled nursing care and home health aids were based on Medicare reimbursement rates, and housekeeping costs were based on national wage rates, home oxygen was based on Medicare reimbursement. Postdischarge utilization costs were based on Medicare reimbursement.
For the primary analysis, mean per-patient costs were calculated for the azithrolmycin and levotloxacin groups separately, and then compared using a difference score and a two-sample t test. For a sensitivity analysis, we formed 100 bootstrap samples (original data and 99 replications). For each of the replications, we took a random sample, with replacement, of the 163 patients from the trial. Because these samples were taken with replacement, some patients will not appear in any particular sample, while others will appear multiple times. In aggregate, the replicate samples provide a synthetic estimate of the amount of variability in the cost estimates that would be observed were in CAP-IN to be repeated multiple times. Accordingly, the robustness of the conclusions can be described by calculating the difference in the average cost of the azithromycin and levofloxacin groups for each replication, and then summarizing this distribution (n = 100) using statistics such as the mean, SD, and percentage of replications for which the total cost of azithromycin exceeds that of levotloxacin. (6)
RESULTS
The study population is described in more detail elsewhere. (5) Briefly, for those patients included in the economic analysis from the levofloxacin group, 57% were male, 86% were white, and the mean age was 72.8 years (SD, 13.5). The azithromycin group was demographically similar: 57% were male, 86% were white, and mean age was 71.4 years (SD, 13.0). Symptom severity at baseline was also similar: 40% of patients from both groups had the most severe possible classification (on a 1 to 4 scale) of symptoms.
Table 1 summarizes the results of the economic analysis. The large majority of costs were associated with hospitalization. The mean hospital length of stay (LOS) was 8.8 days (SD, 7.0) in the levofloxacin group vs 7.0 days (SD, 3.7) in the azithromycin group (p = 0.03). Almost all this difference can be attributable to time in general medical wards: 7.4 days in the levofloxacin group vs 5.7 days for azithromycin. These and other figures on total utilization can be derived from Table 1 by recognizing that mean utilization per patient equals mean per patient cost divided by the unit price (these latter two quantities being presented).
The difference in total cost between the azithromycin and levofloxacin groups is estimated to be $2,481 per patient, with an SE of $1,136 (p = 0.03, 95% confidence interval, $238 to $4,724). Of the 100 bootstrapped samples, 98 showed the total costs in the levofloxacin group exceeding those of the azithromycin group (p = 0.02), the range of the bootstrapped confidence interval being consistent with the confidence interval derived from the inputs to the t test above.
Considering individual cost categories, except for drug costs ($243 vs $189) and a few categories having little net impact, the results were consistently in favor of azithromycin, and most of the cost difference is attributable to hospital days, the large majority of these days, in turn, being spent on the general medicine wards. Indeed, of the 82,481 difference in cost, $2,300 is attributable to hospitalization, 82,124 of which is attributable to stays on general medicine wards. Thus, the precise estimate of the cost benefit attributable to azithromycin (if any) depends in large part on the cost assigned to a hospital day. This estimate also depends, of course, on the difference in the mean LOS when comparing the levofloxacin and azithromycin regimens.
DISCUSSION
Treatment regimens that include atypical coverage for hospitalized patients with CAP, specifically macrolides (in combination with a cephalosporin) or levofloxacin, have been shown to reduce hospital LOS and mortality. (7-11) Due to concerns about the potential for resistance, the Centers for Disease Control and Prevention recommend reserving fluoroquinolones in CAP for patients at risk for resistant pneumococcal infections. (12) This is the first prospective study that we are aware of reporting the economic outcomes of azithromycin plus ceftriaxone vs levofloxacin monotherapy.
We found that the direct medical costs of the azithromycin group were $2,481 less than the corresponding costs in the levofloxacin group. The difference in total cost was statistically significant using both a traditional t test and a more sophisticated bootstrapping. Thus, while the precise estimate of the cost benefit attributable to the azithromycin group depends in large part on the cost assigned to a hospital day, the overall conclusion of our primary analysis in favor of azithromycin can be considered to be statistically robust.
A number of technical issues are pertinent to this economic analysis. The first is the choice of patients. As is typical of randomized trials, some patients completed the entire 30-day data collection protocol while others did not. We made the a priori decision to include only those patients having completed all measurements, the primary advantage being that this reduces the number of assumptions that must be made in order to count all components of cost for every patient. The primary disadvantage is the potential for bias; that is, if the utilization for those excluded patients in the azithromycin group differed markedly from the utilization for those excluded patients receiving levofloxacin. In order to assess this potential for bias, we repeated the economic analysis for the 141 of these 161 patients that were also included in the primary analysis of efficacy. (5) The mean difference in cost was $1,546 (SE, $1,082), with 95 of the 100 bootstrapped samples favoring azithromycin (p = 0.15 by t test, p = 0.05 by bootstrapping). Including the four deceased patients (equally divided between azithromycin and levofloxacin groups, with identical total survival times) has no material effect on the conclusions.
In interpreting the above, it may be noted that the point estimate of the mean difference in cost between azithromycin and levofloxacin favored azithromycin in both analyses, falling within the range of $1,500 to $2,500. The evidence supporting the statistical significance of this finding was stronger in the 161 patients used in the primary economic analysis than in the 141 patients also included in the analysis of clinical efficacy. Yet other point estimates could be anticipated were other subgroups of patients to be considered. Moreover, the presence of high-cost outliers can make estimates of mean cost relatively unstable. In each of the above analyses, the confidence interval for the cost benefit attributable to azithromycin included both numbers that were practically unimportant (ie, near $0) as well as those that were quite noteworthy (ie, in the range of $2,000 to $4,000). Overall, a conservative interpretation of the findings would seem to be that azithromycin is no more costly than levofloxacin, and that there is some evidence that it is less so, this evidence being suggestive but not definitive.
The second issue involved the selection of the outcome measure. As previously discussed, there was no reason to believe that costs would differ beyond the 30-day follow-up period of the trial, and thus the analysis was limited to the period of time for which direct observations were available. Also, we chose to compare the two treatments on cost alone rather then cost and quality of life, since the clinical response of the patients suggests that there was no difference in quality of life after 30 days, and any differences in quality of life during the follow-up period of the trial would likely have at most a modest impact on the conclusions of the analysis.
A related issue involves the choice of cost categories to be included in the comparison between the groups. At the design stage, the decision was made to limit respondent burden by focusing data collection on only those elements that might either be associated with large costs, or be differentially distributed across the groups. Within this set of potential cost categories (ie, the rows of Table 1), we included all available elements of cost, regardless of their statistical significance, in order to have as much information as possible regarding the pattern of cost difference, if any. Such an approach seems particularly reasonable in cases such as this one, in which the ultimate focus of the analysis is on total cost.
A final technical issue is the choice of unit prices, the derivation of which required various assumptions (as detailed in Appendix 1), and thus could quite plausibly have used different estimates. Often, sensitivity analyses are performed in order to determine the robustness of the conclusions to changes in these assumptions. As an example of such a sensitivity analysis, the calculations in Appendix 1 resulted in an estimate of the cost of a ward day that appears consistent with experience, and a cost of an ICU day that might be considered to be low in comparison with the cost of a ward day. Increasing the unit price of an ICU day would have little impact on the overall conclusion, other than to increase the difference in cost between azithromycin and levofloxacin. Performing a comprehensive set of sensitivity analyses did not appear to be necessary in this case, however, since the observation that most cost categories were small and involved greater utilization in the levofloxacin group implies that the final estimate will be sensitive to little other than the cost attached to a hospital day in general, and a hospital day spent in a general medicine ward in particular. The precise value for the unit cost associated with such a day will affect the absolute estimate of the savings associated with azithromycin but will have less impact on the statistical testing or the overall conclusion.
How might the conclusion that the azithromycin regimen is no more and perhaps less costly than levofloxacin be placed into perspective? From the clinical perspective, CAP-IN was designed as an equivalency study and, indeed, demonstrated similar clinical success (ie, cure) rates at approximately day 30 for azithromycin (86.2%) compared with the levofloxacin group (83.7%).5 This was consistent with a multicenter, randomized, open-label study by Frank et al (13) (sponsored by Ortho-McNeil), which showed that azithromycin plus ceftriaxone was comparable to levofloxacin monotherapy with clinical success (defined as cured and improved) rates of 92.3% vs 94.1% and microbiological eradication rates of 92.3% vs 89.5% for respective regimens at 2 to 7 days after completing therapy. However, in the efficacy analysis for CAP-IN, the azithromycin group appeared to have an advantage in the percentage of patients considered cured (68.2% for azithromycin vs 53.0% for levofloxacin groups) at the end of therapy (day 14 [+ or -] 2). (5) Similar results were obtained using the patients included in this cost analysis (66.7% vs 53.1%, respectively). Perhaps the azithromycin group experienced faster symptom resolution resulting in a shorter hospitalization. This shorter hospitalization was not obtained at the cost of greater subsequent utilization among patients receiving azithromycin; indeed, the azithromycin group was associated with somewhat lower postdischarge resource use and an estimated posthospitalization cost savings of approximately $233 per patient.
The pharmacologic rationale for these findings is unclear. One study (14) reported azithromycin having superior in vitro activity vs levofloxacin against M pneumoniae and C pneumoniae. In CAP-IN, a total of 66 patients had an atypical pathogen at baseline (54.5% had M pnenmoniae, 42.4% had C pneumoniae, and 3.1% had L pneumophila) in the efficacy analysis. However, clinical success rates were higher at the end of levofloxacin therapy for M pneumoniae (94.1% vs 78.9%). In contrast, clinical success rates were higher for the azithromycin group in patients with C pneumoniae (90.9% vs 87.5%) as well as S pneumoniae (100% vs 55.6%). (5) Since the number of patients with isolates was relatively small, it is difficult to draw conclusions from these findings. In addition to the antimicrobial effort, the potential inflammatory modulation attributed to macrolides may contribute to symptomatic improvement, although this has not been demonstrated. (7,15)
In conclusion, our primary analysis found that the direct medical costs of the azithromycin group were $2,481 less than the corresponding costs in the levofloxacin group, this difference resulting from a 1.8-day reduction in the average LOS. Conservatively, the azithromycin regimen is certainly no more, and quite possibly less costly than the levofloxacin regimen. The precise estimate of the cost benefit, if any, attributable to azithromycin depends on both its role in reducing LOS and in the cost assigned to a hospital day. Cost is but one of many considerations in determining the most appropriate course of action for any individual patient.
APPENDIX: ESTIMATION OF UNIT COSTS FOR INPATIENT CAP
The following lists, by resource type, the data sources and processing used to estimate unit costs.
A. Hospitalization Per Diem Costs
Estimating per diem costs for ICU and ward care for base case and sensitivity analysis was based on a study by Dresser et al, (1) the Health Care Utilization Project data, (2) and the Healthcare Cost Report Information System. (3)
Step 1. Derive Per Diem Costs: The report by Dresser et al (1) provides aggregate estimates of hospital costs and LOS. From data on proportion of patients with severe disease, LOS in ICU and ward settings for patients with severe disease, and with the assumption that patients with nonsevere CAP did not spend time in the ICU, it is possible to infer the cost of an ICU and ward day as follows:
1. The study by Dresser et al (1) study provides the following for a group of patients with CAP similar to the current trial (Table 2).
2. From these, one can estimate ward and ICU LOS (Table 3).
Further, from these data, we can back-calculate to derive the cost of an ICU day and the cost of a ward day by noting the following:
Total cost (a) = cost per ICU day x days in ICU (a) + cost per ward day x days on ward (a)
and
Total cost (b) = cost per ICU day x days in ICU (b) + cost per a ward day x days of ward (b)
For both treatments, we assume the per diem cost for the ICU or ward are unrelated to the treatment arm. The result is two simultaneous equations with two unknowns: cost per ICU day and cost per ward day. The result of this in 2000 dollars (unadjusted) and adjusted to 2002 (based on medical cost-of-living inflators of 104.1% for 2000 to 2001 and 104.7% for 2001 to 2002) is given in Table 4.
The resulting 2002 medical consumer price index (CPI)-adjusted costs are used for baseline analysis.
Step 2. Estimate a Plausible Range of Values for Per Diem Cost of ICU and Ward Care for Sensitivity Analysis:
1. Based on the Health Care Utilization Project data set, identify a range of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes that are likely to be used for CAP. Of the 44 codes corresponding to pneumonia, delete the codes clearly not corresponding to CAP, such as codes related to tuberculosis, fungal infection, or viral infection. Of the remaining, include codes with frequencies > 1% of all pneumonia hospital admissions.
2. From the Healthcare Cost Report Information System data set for 2002, extract the operating cost-to-charge ratios (OCCRs) for each state. Calculate the average, median, and interquartile range (IQR) for OCCRs. Estimate per diem costs for each pneumonia diagnosis, for the average, median, and low and high IQR values.
3. As a check of the estimated total cost for CAP based on the study by Dresser et al, (1) each estimated per diem value from step 2, above, is multiplied by the total LOS in the study by Dresser et al. (1) The resulting range of values extends from $4,328 to $9,124. Notably, the mean estimates of Dresser et al (1) for all patients ($6,143) [adjusted to 2002 dollars] is within this range (Table 5). From Table 5, we see that if the total cost was based on ICD-9-CM diagnosis code 482-1 high IQR OCCR-adjusted per diem Medicare costs, the total cost estimate from Dresser et al (1) would have been $9,292 (high IQR total cost); if the total cost was based on ICD-9-CM diagnosis code 495 low IQR OCCR-adjusted per diem Medicare costs, the total estimate from Dresser et al (1) would have been $4,328 (low IQR total cost).
4. For the sensitivity analysis, we consider that the per diem values from Dresser et all were either underestimated or overestimated, compared to cost estimates from Medicare. The high per diem ICU and ward costs are derived by multiplying the base per diem estimates (from Dresser et al (1)) by an "underestimate adjustment factor" (high total cost/ Dresser et al (1) total cost = $9,124/$6,143 = 1.5); the low per diem ICU and ward costs are derived by multiplying the base per diem estimates by an "overestimate adjustment factor" (low IQR total cost/ Dresser et al (1) total cost = $4,328/$6,143 = 0.7). Thus, the high estimate for per diem ICU cost is $1,348 x 1.5 and ward cost is $1,260 x 0.7. The results are shown in Table 6.
B. Drug Unit Costs
Treatment A: Azithromycin IV Plus Ceftriaxone IV (With or Without Cefuoxime) Followed by Oral Azithromycin: Based on the study protocol (Pfizer protocol No. A0661035), (4) IV azithromycin, 500 mg, was administered qd for 2 to 5 days with ceftriaxone, 1 g qd, for at least 2 days (up to 5 days at the discretion of the site investigator) followed by oral azithromycin, 2 x 250 mg qd, to complete a total of 7 to 10 days of therapy. Subjects randomized to azithromycin plus ceftriaxone could also receive cefuroxime axetil oral therapy concomitantly with azithromyein oral therapy if a macrolide-resistant S pneumoniae is confirmed or suspected. Oral cefuroxime axetil may be administered at the discretion of the investigator. Cefuroxime axetil, as optional add-on oral therapy, was not provided by the sponsor; for purposes of economic analysis, its cost is included in the estimate of total antibiotic cost.
Azithromycin for injection was supplied as a lyophilized powder under vacuum in a 10-mL vial equivalent to 500 mg of azithromycin for IV administration. The concentrated powder was diluted in 250 mL (2 mg/mL) in a compatible diluted and infused over 1 h. Oral azithromycin was supplied as 250-mg tablets. Ceftriaxone was supplied as a sterile crystalline powder in vials containing 1-g equivalent of ceftriaxone. IV ceftriaxone was diluted in 100 mL (10 mg/mL) of compatible diluent and infused over 30 min.
Treatment B: Levofloxacin IV Followed by Oral Levofloxacin: IV Levofloxacin, 500 nag qd, was administered for a minimum of 2 days followed by oral Levofloxacin, 500 mg qd, to complete a total of 7 to 14 days of therapy. Levofloxacin injection was supplied as a single-use vial containing a concentrated solution with the equivalent of 500 mg of levofloxacin. Levofloxacin tablets for oral administration were supplied as 500-mg, rectangular, film-coated tablets. For patients with renal insufficiency (creatinine clearance < 50 mL/min), levofloxacin dosage adjustment was required. These patients received IV levofloxacin at a dose of 500 mg qd for the initial dose, followed by 250 mg qd for all subsequent IV and oral doses, to complete a total of 7 to 14 days of therapy.
The Federal Supply Schedule is a multiple award, multiyear federal contract that is available for use by any federal government agency and is used here as a surrogate for true cost. Based on Federal Supply Schedule (5) prices in force from January 2001 to January 2002, we estimate the following prices per dose (Table 7):
Preparation and Administration: Costs for preparation and administration were obtained from Dresser et al, (1) who used averaged estimates from microcosting studies, (6-9)) and adjusted to 2000 dollars ($8 for an IV dose and $2 for an oral dose). Reinflated to 2002 dollars, these translate to $8.71 and $2.18 for IV and oral dosing, respectively.
C. Services and Equipment
Unit costs for home-care services and equipment were derived from the Medicare schedule for the Healthcare Common Procedure Coding System code applied to the relevant service, or, in the ease of non-Medicare-reimbursed housekeeper services, from estimates for the Bureau of Labor Statistics. Physician and ED visits were based on typical common procedural terminology code (Table 8).
D. Productivity Unit Costs
Productivity cost of $23.36/h was estimated as total hourly employer cost for compensating all civilian workers in 2002 (http://www.stats.bls.gov/.)
APPENDIX REFERENCES
(1) Dresser LD, Niederman MS, Paladiuo JA. Cost-effectiveness of gatifloxacin vs ceftriaxone with a macrolide for the treatment of community-acquired pneumonia. Chest 2001; 119: 1439-1448
(2) Healthcare Cost Report Information System (HCRIS) Dataset. Available at: www.cms.hhs.gov/data/download/beris_hha/ Readme_09_30_03.asp. Accessed September 30, 2004
(3) Healthcare Cost and Utilization Study HCUPnet. Availal)le at: www.ahrq.gov/data/heup/heupnet.htnl. Accessed September 28, 2003
(4) Zervos M, Mandell LA, Vrooman PS, et al. Comparative efficacies and tolerabilities of intravenous azithromycin plus ceftriaxone and intravenous levofloxacin with step-down oral therapy for hospitalized patients with moderate to severe community-acquired pneumonia. Treat Respir Med 2004; 3:329-336
(5) Federal supply schedule for pharmaceuticals. Available at: www.vapbm.org/PBM/prices.htm. Accessed September 28, 2003
(6) Smith CF, Amen RJ. Comparison of seven methods of preparing and administering small-volume injections. Am J Hosp Pharm 1988; 45:1896-1901
(7) Foran RM, Brett JL, Wulf PH. Evaluating the cost impact of IV antibiotic dosing frequencies. DICP 1991; 25:546-552
(8) Cunha BA. IV-to-oral antibiotic switch therapy. Postgrad Med 1997; 101:111-128
(9) Hatoum HT. Mierocost analysis of inpatient dispensing and administration of oral solids. Am J Hosp Pharm 1990:47:800-805
(10) Federal Register. Vol 66. No 126. June 29, 2001, pp 34691
(11) Bureau of Labor Statistics. Available at: www.stats.bls.gov/. Accessed September 28, 2003
(12) Centers for Medicare and Medicaid Durable Medical Equipment, Prosthetics, Ortholics and Supplies. Available at: www.ems. hhs.providers.pufdownload/default.asp#dme. Accessed September 28, 2003.
(13) Medicare physician fee schedule. Available at: www.cms. hhs.gov/physicians/pfs/. Accessed October 31, 2005
REFERENCES
(1) Marrie TJ, Peeling RW, Fine MJ, et al. Ambulatory patients with community-acquired pneumonia: the frequency of atypical agents and clinical course. Am J Med 1996; 101:508-515
(2) Vergis EN, Indorf A, File TM Jr, et al. Azithromycin vs. cefuroxime plus erythromycin for empirical treatment of community-acquired pneumonia in hospitalized patients. Arch Intern Med 2000; 160:1294-1300
(3) Staid JE, Barza MD, Desfardin J, et al. Effect of macrolides as part of initial empiric therapy on length of stay in patients hospitalized with community-acquired pneumonia. Arch Intern Med 1999; 159:2576-2580
(4) Mandell LA, Bartlett JG, Dowell SF, et al. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis 2003; 37:1405-1433
(5) Zervos M, Mandell LA, Vrooman PS, et al. Efficacy and safety of intravenous azithrolmycin plus ceftriaxone versus intravenous levofloxacin with step down oral therapy for the treatment of hospitalized patients with moderate to severe community acquired pneumonia. Respir Med 2005 (in press)
(6) Good PI. Resampling methods: a practical guide to data analysis. Boston MA: Birkhauser Publishers, 1999
(7) Brown RB, Iannini P, Gross P, et al. Impact of initial antibiotic choice on clinical outcomes in community-acquired pneumonia: analysis of a hospital claims-made database. Chest 2003; 125:1503-1511
(8) Dudas V, Hopefl A, Jaeobs R, et al. Antimicrobial selection for hospitalized patients with presumed community-acquired pneumonia: a survey of nonteaching US community hospitals. Ann Pharnmcother 2000; 34:446-452
(9) Houck PM, MacLehose RF, Niederman MS, et al. Empiric antibiotic therapy and mortality among Medicare pneumonia inpatients in 10 western states. Chest 2001; 119:1420-1426
(10) Stahl JE, Barza M, DesJardin J, et al. Effect of macrolides as part of initial empiric therapy on length of stay in patients hospitalized with community-acquired pneumonia. Arch Intern Med 1999; 159:2576-2580
(11) Gleason PP, Meehan TP, Fine JM, et al. Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia. Arch Intern Med 1999; 159:2562-2572
(12) Heffelfinger JD, Dowell SF, Jorgensen JH, et al. Management of community-acquired pneumonia in the era of pneumococcal resistance: a report from the Drug-Resistant Streptococcus pneumoniae Therapeutic Working Group. Arch Intern Med 2000; 160:1399-1408
(13) Frank E, Liu J, Kinasewitz G, et al. A multicenter, open-label, randomized comparison of levofloxacin and azithromycin plus ceftriaxone in hospitalized adults with moderate to severe community-acquired pneumonia. Clin Ther 2002: 24:1292-1308: erratum Clin Ther 2003; 25:1039
(14) Critchley IA, Jones ME, Heinze PD, et al. In vitro activity of levofloxacin against contemporary clinical isolates of Legionella pneumophila, Mycoplasma pneumoniae, and Chlamydia pneumoniae from North America and Europe. Clin Microbiol Infect 2002; 8:214-221
(15) Sanchez F, Mensa J, Martinez JA, et al. Is azithromycin the first choice macrolide for treatment of community-acquired pneumonia. Clin Infect Dis 2003; 36:12.39-1245
* From the Center for Clinical Health Policy Research, Department of Biostatistics and Bioinformatics (Dr. Samsa), and Department of Medicine (Dr. Matchar), Duke University; and Pfizer Pharmaceuticals (Drs. Harnett and Wilson), New York, NY.
Funding for this study was provided by Pfizer Pharmaceuticals, which set no limitations on content.
Manuscript received April 26, 2004; revision accepted April 11, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Gregory P. Samsa, PhD, Center for Clinical Health Policy Research, Duke University, Wachovia Plaza, 2200 West Main St, Durham, NC 27705: e-mail samson001@mc. duke.edu
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group