Study objectives: Levofloxacin is a fluoroquinolone antimicrobial agent for which pharmacodynamic relationships between the maximum serum antibiotic concentration (Cmax)/minimum inhibitory concentration (MIC) ratio and/or the area under the serum concentration-time curve during a 24-h dosing period ([AUC.sub.0-24])/MIC ratio and clinical and/or microbiological outcomes have been developed. In this study we examined the relationship between the in vitro bacterial susceptibility to levofloxacin, the achieved levofloxacin serum and sputum concentrations, and the in vivo bacterial eradication in patients with acute exacerbations of chronic bronchitis.
Patients and interventions: Thirty patients received levofloxacin, 500 mg/d po for 7 days. Samples of venous blood and sputum for the determination of levofloxacin concentrations were collected on day 1 immediately prior to dosing, and then at 1, 4, 8, 12, and 24 h.
Results: The mean peak concentration in serum (6.5 mg/L) was found 1 h after administration, and at 4 h after administration in sputum (5.1 mg/L). Levofloxacin was always detectable 24 h after administration from both samples. Successful treatment occurred in 90% (27 of 30 patients) when assessed both clinically and bacteriologically. Treatment was successful in eight patients when the [AUC.sub.0-24]/MIC ratio was > 40 for serum, and in nine patients when it was > 30 for sputum. Treatment was also successful in seven patients when the Cmax/MIC ratio was > 5.01 for serum, and in nine patients when the Cmax/MIC ratio was > 4.01 for sputum. Treatment was successful in 90% (27 of 30 patients) when the [AUC.sub.0-24]/MIC ratio was > 125 for serum and > 100 for sputum, and when Cmax/MIC was > 10.01 for serum and > 8.01 for sputum following the first dose.
Conclusions: The pharmacodynamics values that we have obtained in sputum with levofloxacin may be used as predictors of therapy outcomes.
Key words: acute exacerbations of chronic bronchitis; levofloxacin; pharmacodynamics; pharmacokinetics
Abbreviations: [AUC.sub.0-24] = area under the serum concentration-time curve during a 24-h dosing period; CI = confidence interval; Cmax = maximum serum antibiotic concentration; MIC = minimum inhibitory concentration
**********
The therapeutic significance of antibiotic concentrations is debatable. However, some studies (1) have suggested that an efficient antimicrobial penetration into potential sites of pulmonary infection and its protracted permanence in active form are advantageous.
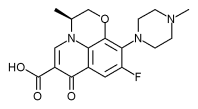
Levofloxacin, a fluoroquinolone antimicrobial agent with somewhat enhanced activity against Gram-positive cocci, penetrates extensively into various tissues and body fluids. Concentrations achieved in epithelial lining fluid, alveolar macrophages, bronchial mucosa, and lung tissues are often higher than those in plasma. (2-5)
Unfortunately, pulmonary penetration alone does not promote an understanding of the pharmacologic effects of a drug. In vivo bacteria are not exposed to constant, but to constantly changing, antibiotic concentrations, with peaks and troughs. (6) Therefore, also at the pulmonary site of infection, the pathogens are exposed to a gradient of antibiotic concentration according to its pharmacokinetics. (6) For this reason, the correlation between pulmonary disposition of the drug and its minimum inhibitory concentration (MIC) values for the infectious agent represents a more feasible calculation probably correlated to the clinical outcome. (7)
Fluoroquinolones have concentration-dependent bactericidal activity and a prolonged postantibiotic effect against Gram-positive and Gram-negative bacteria. (8,9) The pharmacodynamic parameters that correlate with successful clinical and microbiological outcomes and prevention the emergence of bacterial resistance are the ratio of maximum serum antibiotic concentration (Cmax) to the MIC, and the ratio of the area under the serum concentration-time curve during a 24-h dosing period ([AUC.sub.0-24]) to the MIC. (7)
The difficulty of measuring interrelationship between pulmonary pharmacokinetics and pharmacodynamics with the clinical and microbiological outcomes, however, is well recognized, mainly because it is more feasible and ethical to sample blood rather than repeated sputum, bronchial mucosa, or epithelial lining fluid. Nevertheless, studies looking at the impact of the pulmonary pharmacodynamics on clinical and microbiological outcomes are awaited. (10) In this study, we examine the relationship between the in vitro bacterial susceptibility to levofloxacin, the achieved levofloxacin serum and sputum concentrations, and in vivo eradication of the bacteria in patients with acute exacerbations of chronic bronchitis.
MATERIALS AND METHODS
Patients
This investigation involved 30 patients with a diagnosis of acute bacterial exacerbation of chronic bronchitis who had sufficient volumes of sputum to permit daily cultures. Table 1 shows the baseline demographics and characteristics of the enrolled patients. The diagnosis of chronic bronchitis was consistent with the criteria of the European Respiratory Society (11) and was established based on clinical history, physical findings, and positive culture results. Acute exacerbation was defined as an alteration in the quiescent state of the patient with an increase in frequency of cough, increase in quantity and/or purulence of the sputum, presence of pulmonary crackles or rhonchi, and isolation of pathogens. Patients were excluded if they had a history of hypersensitivity to fluoroquinolones; previous antimicrobial therapy within i week preceding study enrollment; significant hepatic, renal; or hematologic abnormalities; or underlying medication conditions that would interfere with assessment of clinical efficacy. Patients were also excluded if they had active tuberculosis, cystic fibrosis, primary or metastatic carcinoma involving the lung, AIDS, or known seropositivity for HIV antigen or antibody.
Diagnosis of the condition was based on patient history (fever, increased cough, sputum, and shortness of breath) and physical examination (tales, purulence of sputum, radiograph, spirometry). All bacteriology was performed at local hospital laboratory. Bacterial flora of the sputum were determined by use a wet preparation and a Gram stain. Acceptable sputum specimen contained < 10 epithelial cells and > 25 WBCs per low-power field (x 100). The finding in sputum of a predominance of polymorphonuclear eosinophils or the presence of swollen bronchial epithelial cells with inclusion bodies excluded patients from the study. Pathogenic microorganisms were only regarded as significant in case of reaching [greater than or equal to] [10.sup.6] cfu/mL, except for Streptococcus pneumoniae, in which growth of > [10.sup.5] cfu/mL was deemed sufficient. In vitro susceptibility tests for the study drug were performed on all isolates by disk diffusion and broth microdilution methods following the National Committee for Clinical Laboratory Standards guidelines. (12) Approval for this study was obtained from an institutional ethics committee, and informed consent was obtained for all patients prior to study participation.
Antibiotic Treatment
The patients received 500 mg/d po of levofloxacin for 7 days. Patients were instructed to refrain from using systemic antibiotics other than the studied medication. Concomitant use of other drugs was recorded during the trial.
Clinical and Microbiological Assessment
Clinical and microbiological assessments ([+ or -] ME) were performed at hospital admission (pretherapy visit), after 8 [+ or -] 2 days (posttherapy visit), and after 28 [+ or -] 4 days (late posttherapy visit). The effectiveness of the treatment was determined on the clinical and bacteriologic response of the patients.
Clinical signs and symptoms of cough, sputum production, and dyspnea were graded at each study visit as absent, mild, moderate, or severe. Sputum was graded as absent, mucoid, mucopurulent/blood streaked, or purulent. Rales, rhonchi, wheezing, and pleura/ rub were graded as absent or present. Fremitus was graded as increased, normal, or decreased. Temperature was recorded. Sputum was collected for culture at the hospital admission visit and, if available, at subsequent visits. Clinical response was graded by the investigators as follows: (1) cure: elimination of signs and symptoms with no recurrence at the late posttherapy visit; (2) improvement: a marked or moderate reduction in the severity and/or numbers of clinical signs and symptoms of infection and no further antibiotic treatment indicated; (3) relapse: reappearance of clinical signs and symptoms of the initial infection up to 28 [+ or -] 4 days after treatment after the initial cure; and (5) failure: no improvement of clinical signs and symptoms. Patients were designated as "unappreciable" if they could not be assigned to a category and were disqualified for efficacy analysis.
The bacteriologic response was based on the results of culture samples obtained before and after therapy and was assessed as one of nine possible categories: (1) cure: initial pathogen eradicated during or at completion of therapy; (2) presumed bacteriologic cure: clinical cure or improvement as defined above but where an appropriate sputum specimen could not be obtained or cultured at the during treatment or posttreatment visits); (3) bacteriologic cure with superinfection: bacteriological cure as defined above plus the isolation of one or more new pathogens; (4) bacteriological cure with colonization: bacteriologic cure as defined above plus the isolation of one or more new organisms not considered pathogenic; (5) bacteriologic recurrence: bacteriologic cure as defined above plus the isolation of the original pathogen at follow-up; (6) bacteriologic failure: initial pathogen not eradicated from cultures after at least 3 days of therapy, requiring additional or alternative treatment; (7) presumed bacteriologic failure: clinical failure or recurrence as defined above but where a sputum specimen could not be obtained or cultured; (8) bacteriologic failure with superinfection: bacteriologic failure as defined above plus the isolation of one or more new pathogens; and (9) bacteriologic failure with resistance: bacteriologic failure as defined above with initial pathogen(s) developing resistance to the study drug during the course of therapy. Patients were instructed to contact the investigator if any adverse event occurred. All adverse events were recorded. Each event was classified as mild, moderate, or severe based on the investigator's clinical assessment of the patient's condition and evaluated for their relationship to drug administration. Patients were withdrawn from the study because of clinical failure, relapse, a significant adverse event, or at the request of the patient or physician.
Pharmacokinetic and Pharmacodynamic Parameters
Samples of venous blood and sputum for the determination of levofloxacin concentrations were collected on day 1 immediately prior to the dose and then at the following times after dosing: 1, 4, 8, 12, and 24 h from each patient. Sputum samples were sent to a local laboratory for Gram stain, culture, and susceptibility testing. The MICs of levofloxacin for the isolates were determined by the National Committee for Clinical Laboratory Standards broth microdilution method. (12)
On the contrary, blood and sputum samples for the pharmacokinetic evaluation were stored at -70 [degrees]C within 1 h of sampling. Defrosted sputum was sonicated in a circulating water bath (4 [degrees]C for 2 min at 100 W) and then centrifuged (12,000g for 3 min). Assays were performed on superuatant. An Escherichia coli American Type Culture Collection 25922 bioassay was used to determine the levofloxacin concentration in each sample. (12) The standard curve was performed in Hanks balanced salt solution containing 40% decomplemented pooled serum. The curve was linear between 0.07 [micro]g/mL and 20 [micro]g/mL. The limit of sensitivity of the assay was 0.05 [micro]g/mL in serum and 0.1 [micro]g/mL in sputum. The mean intra-assay and interassay coefficients of variation were < 5%.
The Cmax of the antimicrobial agent relative to the MIC value (Cmax/MIC ratio), and the ratio of the [AUC.sub.0-24] to the MIC were determined from concentration-time data, and the initial MIC for each isolate pathogen was calculated. Since the conventionally reported MIC is biased upwards, the MIC used on the analysis was transformed to the MIC midpoint. This was computed as the midpoint between the reported MIC and the next lower value in the dilution series. (13)
RESULTS
Microbiologic Results
Nine patients had infections with S pneumoniae, eight patients with Haemophilus influenzae, six patients with Moraxella catarrhalis, four patients with Haemophilus parainfluenzae, and three patients with Staphylococcus aureus. Among the S pneumoniae isolates, all but one, which had a MIC of 16 [micro]g/mL, were found to be fully susceptible to levofloxacin. All H influenzae, M catarrhalis, and H parainfluenzae isolates were fully susceptible to levofloxacin. Two of three S aureus isolates were methicillin resistant, and the levofloxacin MIC was > 4 mg/L (the first isolate had a MIC of 8 [micro]g/mL, and the second isolate had a MIC of 64 [micro]g/mL). The range of MIC values is referred in Table 2.
Pharmacokinetic Profile
The mean peak concentration in serum (6.5 mg/L; 95% confidence interval [CI], 4.3 to 8.7) was found 1 h after administration, while that in sputum (5.1 mg/L; 95% CI, 2.4 to 7.8) was found 4 h after administration. Levofloxacin was always detectable 24 h after administration both in serum (0.8 [micro]g/mL; 95% CI, 0.3 to 1.3) and in sputum (1.2 [micro]g/mL; 95% CI, 0.1 to 2.3) [Fig 1]. The mean [AUC.sub.0-24] was 39.60 mg/L (95% CI, 25.57 to 53.16) in serum and 37.38 [micro]g/mL (95% CI, 13.80 to 61.08) in sputum.
[FIGURE 1 OMITTED]
Clinical Outcomes
At the posttherapy visit, treatment was successful (cure or improvement) in 27 patients (90%). At the late posttherapy visit, all cured patients were exacerbation free (Table 3).
Microbiologic Outcomes
Eradication rates at the end of treatment were 90% (27 of 30 patients). Persistence of S pneumoniae isolates was found in one of nine patients (11.1%), whereas that of S aureus was found in two of three patients (66.6%). Both of the strains were methicillin resistant. At the late posttherapy visit, there was not recurrence or reinfection.
Pharmacodynamics vs Antibacterial Response
Treatment was successful in eight patients when the [AUC.sub.0-24]/MIC ratio was > 40 for serum and in nine patients when it was > 30 for sputum. It was also successful in seven patients when the Cmax/ MIC ratio was > 5.01 for serum and in nine patients when it was > 4.01 for sputum. Treatment was successful in 90% (27 of 30 patients) when the [AUC.sub.0-24]/MIC ratios were > 125 for serum and 100 for sputum, and Cmax/MIC was > 10.01 for serum and > 8.01 for sputum following the first dose (Table 4). When response was partitioned by bacterial species and pharmacokinetics/pharmacodynamics parameters, two methicillin-resistant S aureus eases (MIC = 16 [micro]g/mL and 64 [micro]g/mL, respectively) and one levofloxacin-resistant S pneumoniae case (MIC = 16 [micro]g/mL) failed treatment. This was a consequence of higher MICs that did not allow to reach neither [AUC.sub.0-24]/MIC ratio > 40 for serum and > 30 for sputum nor Cmax/MIC ratio > 5.01 for serum and > 4.01 for sputum.
DISCUSSION
With fluoroquinolones, an [AUC.sub.0-24]/MIC ratio of 25 to 40 (roughly equivalent to a Cmax/MIC of 3:1) has been correlated with a survival benefit in 50% of the infected animals. (14) However, data from in vitro and animal models (15-17) of infection suggest that [AUC.sub.24]/MIC ratios for S pneumoniae < 30 were associated with significantly reduced extents of bacterial killing and in some instances regrowth.
Other authors, such as Schentag, (18) support the [AUC.sub.24]/MIC ratio target of 125. With an [AUC.sub.0-24]/ MIC ratio of 125 (Cmax/MIC, 5:1), approximately 80% of all the available AUC from the regimen is above the MIC.
As there has generally been good correlation between data gleaned from in vitro and animal models and data from the few human studies, (10) a reasonable working hypothesis is that [AUC.sub.0-24]/MIC ratios of approximately 125 predict optimal activity of fluoroquinolones, although ratios as low as 30 to 50 may be sufficient for S pneumoniae. Nonetheless, supporting human data confirming these observations are extremely limited.
An early human study (19) relevant to fluoroquinolone pharmacodynamics was conducted with ciprofloxacin in patients with nosocomial pneumonia. In this study of 50 patients, (19) bacterial eradication from the lower respiratory tract was correlated with high Cmax/MIC ratios and high [AUC.sub.0-24]/MIC ratios. Other studies in humans have documented that at an [AUC.sub.0-24]/MIC ratio of > 125 (45 patients), the probabilities of clinical and microbiological cures were significantly higher, (20) although lower [AUC.sub.0-24] MIC ratios may be sufficient in the treatment of Gram-positive infection. (13,21,22)
Our study confirms that levofloxacin is effective in the treatment of acute exacerbation of chronic bronchitis. It also indicates that a serum [AUC.sub.0-24]/MIC ratio > 125 and/or a sputum [AUC.sub.0-24]/MIC ratio > 100, and a serum Cmax/MIC ratio of [greater than or equal to] 10 and/or a sputum Cmax/MIC ratio [greater than or equal to] 8 are predictors of therapeutic efficacy for levofloxacin in patients with an acute exacerbation of chronic bronchitis and this independently from the offending pathogens, although sometimes lower [AUC.sub.0-24]/MIC and Cmax/ MIC ratios might be sufficient.
Levofloxacin was ineffective against two isolates of S aureus, both methicillin-resistant strains. This was not unexpected, because it is well known that fluoroquinolones do not have high a AUC/MIC ratio for methicillin-resistant S aureus and are unlikely to be effective against these organisms. (18) Furthermore, it has been documented that the MICs of levofloxacin against resistant S aureus were twofold to fourfold above the peak levels achieved in an in vitro pharmacokinetic model. (23)
In this study, the mean Cmax of levofloxacin in sputum (5.1 mg/L) was found at 1 h after administration. The levels that we have measured were similar to those obtained in a series of studies. (2,3,24,25) The levofloxacin high concentrations in lung tissue cause higher Cmax/MIC ratios, with values that approach those proposed by Schentag. (18) Therefore, we can postulate that the relatively low values that we have found in sputum as good predictors of therapeutic efficacy for levofloxacin in patients with an acute exacerbation of chronic bronchitis could reflect higher value in lung tissue. A Japanese study (26) that enrolled 23 patients undergoing lung resection or bronchoscopy has shown a very strong correlation between the level of levofloxacin in lung tissue and that in serum, whereas correlation between those in sputum and in serum was not significant. This finding indicates that the correlation between lung tissue concentration of the drug and its MIC values for the infectious agent is more important than that between sputum concentration and MIC. However, since obtaining serial samples is difficult to impossible in protected sites like those in lung, mainly bronchial mucosa; also for ethical reasons, one must examine only a single sample from each site of interest from each patient. (10) Using a site/plasma drug concentration ratio at a single time point as a measure of drug penetration is problematic, as there is often system hysteresis that causes the ratio to change nearly continuously with time. (16) For all these reasons, we believe that interrelationship between the sputum pharmacokinetics and pharmacodynamics is a feasible real pulmonary predictor for outcome, at least in acute exacerbations of chronic bronchitis. This means that the pharmacodynamic values that we have obtained in sputum with levofloxacin may be used as predictors of therapy outcomes.
Manuscript received October 4, 2004; revision accepted February 25, 2005.
REFERENCES
(1) Honeybourne D. Antibiotic penetration in the respiratory tract and implications for the selection of antimicrobial therapy. Curr Opin Pulm Med 1997; 3:170-174
(2) Lee LJ, Sha X, Gotfried MH, et al. Penetration of levofloxacin into lung tissue after oral administration to subjects undergoing lung biopsy or lobectomy. Pharmacotherapy 1998; 18: 35-41
(3) Andrews JM, Honeybourne D, Jevons G, et al. Concentrations of levofloxacin (HR 355) in the respiratory tract following a single oral dose in patients undergoing fibre-optic bronchoscopy. J Antimicrob Chemother 1997; 40:573-577
(4) Gotfried MH, Danziger LH, Rodvold KA. Steady-state plasma and intrapulmonary concentrations of levofloxacin and ciprofloxacin in healthy adult subjects. Chest 2001; 119:1114-1122
(5) Nagai H, Yamasaki T, Masuda M, et al. Penetration of levofloxacin into bronchoalveolar lavage fluid. Drugs 1993; 45(suppl):259
(6) Cazzola M, Matera MG, Noschese P. Parenteral antibiotic therapy in the treatment of lower respiratory tract infections: strategies to minimize the development of antibiotic resistance. Pulm Pharmacol Ther 2000; 13:249-256
(7) Cazzola M, Matera MG. Interrelationship between pharmacokinetics and pharmacodynamics in the design of dosage regimens for treating acute exacerbations of chronic bronchitis. Respir Med 1998; 92:895-901
(8) Lode H, Borner K, Koeppe P. Pharmacodynamics of fluoroquinolones. Clin Infect Dis 1998; 27:33-39
(9) Turnidge J. Pharmacokinetics and pharmacodynamics of fluoroquinolones. Drugs 1999; 58(suppl):29-36
(10) Cazzola M, Matera MG, Terzano C, et al. Delivering antimicrobials to the lungs: considerations for optimising outcomes. Am J Respir Dis 2002; 1:261-272
(11) Siafakas NM, Vermeire P, Pride NB, et al. Optimal assessment and management of chronic obstructive pulmonary disease (COPD). Eur Respir J 1995; 8:1398-1420
(12) National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing: ninth informational supplement. Wayne, PA: National Committee for Clinical Laboratory Standards, 1999
(13) Fuchs PC, Barry AL, Brown SD. Is Escherichia coli ATCC 25922 useful for monitoring broth microdilution tests of fluoroquinolones? J Antimicrob Chemother 1997; 39:549-550
(14) Forrest A, Chodosh S, Amantea MA, et al. Pharmacokinetics and pharmacodynamics of oral grepafloxacin in patients with acute bacterial exacerbations of chronic bronchitis. J Antimicrob Chemother 1997; 40(suppl):45-57
(15) Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 1998; 26:1-10
(16) Lacy MA, Lu W, Xu X, et al. Pharmacodynamic comparisons of levofloxacin, ciprofloxacin, and ampicillin against Streptococcus pneumoniae in an in vitro model of infection. Antimicrob Agents Chemother 1999; 43:672-677
(17) Lister PD, Sanders CC. Pharmacodynamics of levofloxacin and ciprofloxacin against Streptococcus pneumoniae. J Antimicrob Chemother 1999; 43:79-86
(18) Schentag JJ. Clinical pharmacology of the fluoroquinolones: studies in human dynamic/kinetic models. Clin Infect Dis 2000; 31:S40-S44
(19) Peloquin CA, Cumbo TJ, Nix DE, et al. Evaluation of intravenous ciprofloxacin in patients with nosocomial lower respiratory tract infections. Arch Intern Meal 1989; 149: 2269-2273
(20) Forrest A, Nix DE, Ballow CH, et al. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob Agents Chemother 1993; 37:1073-1081
(21) Preston SL, Drusano GL, Berman AL, et al. Pharmacodynamics of levofloxacin: a new paradigm for early clinical trials. JAMA 1998; 279:125-129
(22) Ambrose PG, Grasela DM, Grasela TH, et al. Pharmacodynamics of fluoroquinolones against Streptococcus pneumoniae in patients with community-acquired respiratory tract infections. Antimicrob Agents Chemother 2001; 45:2793-2797
(23) Lister PD. Pharmacodynamics of moxifloxacin and levofloxacin against Staphylococcus aurcus and Staphylococcus epidermidis in an in vitro pharmacodynamic model. Clin Infect Dis 2001; 32(suppl):S33-S38
(24) Nakamori Y, Miyashita Y, Nakatani I, et al. Levofloxacin: penetration into sputum and once-daily treatment of respiratory tract infections. Drugs 1995; 49(suppl):418-419
(25) von Baum H, Bottcher S, Hoffmann H, et al. Tissue penetration of a single dose of levofloxacin intravenously for antibiotic prophylaxis in lung surgery. J Antimicrob Chemother 2001; 47:729-730
(26) Fujita A, Miya T, Tanaka R, et al. Levofloxacin concentrations in serum, sputum and lung tissue: evaluation of its efficacy according to breakpoint [in Japanese]. Jpn J Antibiot 1999; 52:661-666
Mario Cazzola, MD, FCCP; Maria Gabriella Matera, MD, PhD; Giovanna Donnarumma, MD; Maria Antonietta Tufano, MD; Alessandro Sanduzzi, MD; Federico Marchetti, BSc; and Francesco Blasi, MD
* From the Department of Pneumology (Dr. Cazzola), Unit of Pneumology and Allergology, A. Cardarelli Hospital, Naples; Department Experimental Medicine, Units of Pharmacology (Dr. Matera) and Microbiology (Drs. Donnarumma and Tufano), Second University, Naples; Department of Cardiovascular and Respiratory Sciences (Dr. Sanduzzi), Unit of Pneumology, University Federico II, Naples; Medical Department (Mr. Marchetti), GlaxoSmithKline S.p.A., Verona; and Institute of Respiratory Medicine (Dr. Blasi), Polyclinic Hospital, Institute of Care and Research, University of Milan, Milan, Italy.
Dr. Cazzola has received fees for speaking and consulting and/or financial support for attending meetings by Abbott, Altana, AstraZeneca, Boehringer Ingelheim, Chiesi Farmaceutici, GSK, Menarini Farmaceutici, Novartis, and Pfizer. Dr. Matera has received a consulting fee from Boehringer Ingelheim and financial support for attending meetings by AstraZeneca, GSK, and Pfizer. Dr. Donnarumma has received financial support for attending meetings at Wyeth. Dr. Tufano has received fees for speaking by Abbott, Bayer, Biomerieux, Formenti, Pfizer and/or financial support for attending meetings at Biomerieux. Dr. Sanduzzi has received fees for speaking from GSK and MSD. Dr. Marchetti is a GSK employee, and GSK sells levofloxacin in Italy. Dr. Blasi has received research and lectures grants from Abbott, Altana, GSK, Pfizer, and Sanofi-Aventis.
Correspondence to: Mario Cazzola, MD, FCCP, Via del Parco Margherita 24, 80121 Napoli, Italy; e-mail mcazzola@qubisoft.it
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group