HILTON HEAD ISLAND, S.C. -- Among patients who received morphine after cesarean section, 7% developed hypothermia, and lorazepam normalized temperatures in 80% of these women, according to the findings of an early report presented at the annual meeting of the Society for Obstetric Anesthesia and Perinatology.
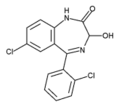
Although larger studies are needed to confirm the effectiveness of lorazepam, low doses of the antianxiety medication are safe and not associated with any side effects. Physicians may want to consider using it if active warming is not effective, said Dr. Jason Wang, an obstetric anesthesia fellow at Beth Israel Deaconess Medical Center, Boston.
Morphine-induced hypothermia is a well-described phenomenon in animals.
"For some reason, morphine decreases the central thermal temperature setting in the brain," he said. The body then perceives the normal temperature of 37[degrees]C to be a fever, spurring peripheral vasodilatation, heat loss, and sweating. Yet this cause of hypothermia is not a commonly recognized phenomenon. Obstetricians and anesthesiologists miss it, because they assume that the patient's temperature has dropped as a result of simply having undergone surgery.
Although active warming measures usually resolve hypothermia caused by surgery patients who have morphine-induced hypothermia tend to remain cold for several hours regardless of heating efforts.
During that time, they're losing water from sweating and increasing their risk of developing cardiac arrhythmias, he said during an interview with this newspaper.
In a study involving 208 women undergoing C-sections, 193 received spinal morphine, and 15 received epidural morphine. A total of 14 patients (7%) became hypothermic, with temperatures dropping below 95.5[degrees]F.
Patients with hypothermia tended to feel hot and sweaty, despite the fact that their temperatures were well below normal.
"One patient's temperature was down to 93[degrees]F, and she still complained of feeling hot," Dr. Wang observed.
Among the 10 patients who received lorazepam, a bolus dose of up to 1 mg by intravenous push, symptoms resolved and temperatures normalized in 8 of the women within 90 minutes.
By comparison, patients who received active warming with commercial warming blankets, hot air pumps, and heated saline intravenously tended to take much longer for their symptoms and temperatures to normalize, he commented.
These findings shouldn't discourage physicians from using intrathecal morphine, Dr. Wang emphasized in an interview. Morphine's benefits in terms of providing powerful and prolonged anesthesia are unrivaled, and the side effect of hypothermia is manageable.
Animal studies have shown that other drugs, such as diazepam, are also effective in at least partially resolving morphine-induced hypothermia, but lorazepam appears to be ideal because it's fast acting and lasts 6-8 hours, which is long enough to prevent a relapse, he said.
COPYRIGHT 2002 International Medical News Group
COPYRIGHT 2002 Gale Group