Definition
Decongestants are medicines used to relieve nasal congestion (stuffy nose).
Purpose
A congested or stuffy nose is a common symptom of colds and allergies. This congestion results when membranes lining the nose become swollen. Decongestants relieve the swelling by narrowing the blood vessels that supply the nose. This reduces the blood supply to the swollen membranes, causing the membranes to shrink.
These medicines do not cure colds or reverse the effects of histamines -- chemicals released as part of the allergic reaction. They will not relieve all of the symptoms associated with colds and allergies, only the stuffiness.
When considering whether to use a decongestant for cold symptoms, keep in mind that most colds go away with or without treatment and that taking medicine is not the only way to relieve a stuffy nose. Drinking hot tea or broth or eating chicken soup may help.
Description
Decongestants are sold in many forms, including tablets, capsules, caplets, gelcaps, liqui-caps, liquids, nasal sprays, and nose drops. These drugs are sometimes combined with other medicines in cold and allergy products designed to relieve several symptoms. Some decongestant products require a physician's prescription, such as Claritin and Allegra, but there are also many nonprescription (over-the-counter) products. Ask a physician or pharmacist about choosing an appropriate decongestant.
Commonly used decongestants include oxymetazoline (Afrin and other brands), phenylpropanolamine, and pseudoephedrine (Sudafed, Actifed, and other brands). The decongestant oxymetazoline is also used in some eye drops to relieve redness and itching.
In addition to being used as a decongestant, phenylpropanolamine also is used as an ingredient in some appetite suppressant products, because it temporarily reduces hunger. Some physicians question its effectiveness as a decongestant.
Recommended dosage
The recommended dosage depends on the drug. Check with the physician who prescribed the drug or the pharmacist who filled the prescription for the correct dosage, and always take the medicine exactly as directed. If using nonprescription (over-the-counter) types, follow the directions on the package label or ask a pharmacists for assistance. Never take larger or more frequent doses, and do not take the drug for longer than directed.
Precautions
Decongestant nasal sprays and nose drops may cause a problem called rebound congestion if used repeatedly over several days. When this happens, the nose remains stuffy or gets worse with every dose. The only way to stop the cycle is to stop using the drug. The stuffiness should then go away within about a week. Anyone who shows signs of severe rebound congestion should also contact his or her physician.
Do not use decongestant nasal sprays for more than 3 days. Decongestants taken by mouth should not be used for more than 7 days. If the congestion has not gone away in this time, or if the symptoms are accompanied by fever, call a physician.
Do not use a decongestant nasal spray after the product's expiration date. If the product has become cloudy or discolored, throw it away and do not use it. Do not share droppers or spray bottles with anyone else, as this could spread infection. Do not let droppers and bottle tips touch countertops or other surfaces.
Some decongestants cause drowsiness. People who takes these drugs should not drive, use machines or do anything else that might be dangerous until they have found out how the drugs affect them.
The decongestant phenylpropanolamine has caused serious side effects, including death, when taken in large amounts. Follow all instructions carefully.
Phenylpropanolamine may interact with caffeine, causing symptoms that include disorientation, confusion, and talking incoherently. Anyone taking phenylpropanolamine should avoid anything that contains caffeine. This includes coffee, tea, cola, chocolate, and many prescription and nonprescription (over-the-counter) medicines. Older people are especially likely to have this problem, so they should be particularly careful about combining caffeine and phenylpropanolamine.
In general, older people may be more sensitive to the effects of decongestants and may need to take lower doses to avoid side effects. People in this age group should not take long-acting (extended release) forms of decongestants unless they have previously taken a short-acting form with no ill effects.
Children may also be more sensitive to the effects of decongestants. Serious side effects are possible if they are given large amounts of these drugs or if they swallow nose drops, nasal spray or eye drops. If this happens, call a physician or poison center immediately.
Special conditions
People with certain medical conditions or who are taking certain other medicines can have problems if they take decongestants. Before taking these drugs, be sure to let the physician know about any of these conditions:
Allergies
Anyone who has had unusual reactions to decongestants in the past should let his or her physician know before these drugs or any similar drugs, such as amphetamine, dextroamphetamine, ephedrine, epinephrine, isoproterenol, metaproterenol (Alupent), methamphetamine, norepinephrine, phenylephrine, pseudoephedrine, or terbutaline (Brethine). The physician should also be told about any allergies to foods, dyes, preservatives, or other substances. In particular, some phenylpropanolamine products also contain the dye tartrazine, which causes an allergic reaction in some people. People who are allergic to aspirin are particularly likely to be allergic to tartrazine.
Pregnancy
In studies of laboratory animals, some decongestants have had unwanted effects on fetuses. However, it is not known whether such effects also occur in people. Women who are pregnant or who plan to become pregnant should check with their physicians before taking decongestants.
Women who take the decongestant phenylpropanolamine after delivery may be more likely to have mood or mental changes.
Breastfeeding
Some decongestants pass into breast milk and may have unwanted effects on nursing babies whose mothers take the drugs. Women who are breastfeeding should check with their physicians before using decongestants. If they need to take the medicine, it may be necessary to bottle feed the baby with formula while taking it.
Other medical conditions
Anyone with heart or blood vessel disease, high blood pressure, diabetes, enlarged prostate, or overactive thyroid should not take decongestants unless under a physician's supervision. The medicine can increase blood sugar in people with diabetes. It can be especially dangerous in people with high blood pressure, as it may increase blood pressure.
Before using decongestants, people with any of these medical problems should make sure their physicians are aware of their conditions:
- Glaucoma
- History of mental illness.
Use of certain medicines
Taking decongestants with certain other drugs may affect the way the drugs work or may increase the chance of side effects.
Side effects
Decongestant nasal sprays and nose drops
The most common side effects from decongestant nasal sprays and nose drops are sneezing and temporary burning, stinging, or dryness. These effects are usually temporary and do not need medical attention. If any of the following side effects occur after using a decongestant nasal spray or nose drops, stop using the medicine immediately and call the physician:
- Increased blood pressure
- Headache
- Fast, slow, or fluttery heartbeat
- Nervousness
- Dizziness
- Nausea
- Sleep problems.
Decongestants taken by mouth
The most common side effects of decongestants taken by mouth are nervousness, restlessness, excitability, dizziness, drowsiness, headache, nausea, weakness, and sleep problems. Anyone who has these symptoms while taking decongestants should stop taking them immediately.
Patients who have these symptoms while taking decongestants should call the physician immediately:
- Increased blood pressure
- Fast, irregular, or fluttery heartbeat
- Severe headache
- Tightness or discomfort in the chest
- Breathing problems
- Fear or anxiety
- Hallucinations
- Trembling or shaking
- Convulsions (seizures)
- Pale skin
- Painful or difficult urination.
Other side effects may occur. Anyone who has unusual symptoms after taking a decongestant should get in touch with his or her physician.
Interactions
Decongestants may interact with a variety of other medicines. When this happens, the effects of one or both of the drugs may change or the risk of side effects may be greater. Do not take decongestants at the same time as these drugs:
- Monoamine oxidase inhibitors (MAO inhibitors) such as phenzeline (Nardil) or tranylcypromine (Parnate), used to treat conditions including depression and Parkinson's disease. Do not take decongestants at the same time as a MAO inhibitor or within two weeks of stopping treatment with an MAO inhibitor unless a physician approves.
- Other products containing the same or other decongestants
- Caffeine.
In addition, anyone who takes decongestants should let the physician know all other medicines he or she is taking. Among the drugs that may interact with decongestants are:
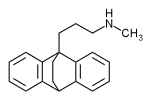
- Tricyclic antidepressants such as imipramine (Tofranil) or desipramine (Norpramin)
- The antidepressant maprotiline (Ludiomil)
- Amantadine (Symmetrel)
- Amphetamines
- Medicine to relieve asthma or other breathing problems
- Methylphenidate (Ritalin)
- Appetite suppressants
- Other medicine for colds, sinus problems, hay fever or other allergies
- Beta-blockers such as atenolol (Tenormin) and propranolol (Inderal)
- Digitalis glycosides, used to treat heart conditions.
The list above does not include every drug that may interact with decongestants. Be sure to check with a physician or pharmacist before combining decongestants with any other prescription or nonprescription (over-the-counter) medicine.
Key Terms
- Appetite suppressant
- Medicine used to help control weight by decreasing the desire to eat.
- Fetus
- A developing baby inside the womb.
- Hallucination
- A false or distorted perception of objects, sounds, or events that seems real. Hallucinations usually result from drugs or mental disorders.
Further Reading
Gale Encyclopedia of Medicine. Gale Research, 1999.