Definition
Bronchodilators are medicines that help open the bronchial tubes (airways) of the lungs, allowing more air to flow through them.
Purpose
People with asthma have trouble breathing, because their airways are inflamed and become narrowed. Normally, air moves smoothly from the mouth and nose through the airways and into the tiny air sacs of the lungs as a person breathes in. Breathing out (exhaling) happens automatically when the person stops breathing in. In a person with asthma, breathing in (inhaling) is not a problem. Incoming air can slide around the blockage, because the act of breathing in makes the airways expand. The problem comes when the person with asthma tries to breathe out. The air can no longer get past the blockage, and it remains trapped in the lungs. The person can then only take shallow breaths. Bronchodilators work by relaxing the smooth muscles that line the airways. This makes the airways open wider and allows air to leave the lungs. These drugs also are used to relieve breathing problems associated with emphysema, chronic bronchitis, and other lung diseases.
Description
Some bronchodilators are inhaled, using a nebulizer or an inhalation aerosol. Others are taken as injections or by mouth. Most are available only by prescription, but a few, such as ephedrine, can be bought without a physician's prescription. Examples of bronchodilators are albuterol (Proventil, Ventolin), epinephrine (Primatene), ipratropium (Atrovent), metaproterenol (Alupent, Metaprel), and terbutaline (Brethine).
Recommended dosage
The recommended dosage depends on the type of bronchodilator and may be different for different patients. Check with the physician who prescribed the drug or the pharmacist who filled the prescription for the correct dosage.
Precautions
Bronchodilators come with patient instructions. Be sure to carefully read them before using the medicine. If there is any confusion about how to use the medicine, check with the physician or pharmacist. Always use these medicines exactly as directed. Taking larger than recommended doses or using the medicine too often can lead to serious side effects and even death.
If symptoms do not improve or if they get worse after using a bronchodilator, call a physician right away.
Although some bronchodilators are available without a physician's prescription, these medicines should not be used unless a physician has diagnosed the patient's condition as asthma.
Some asthma experts believe that the overuse of bronchodilators can cause asthma to get worse. They advise patients and their physicians to consider controlling asthma with anti-inflammatory drugs including inhaled steroids such as beclomethasone dipropionate (Beclovent, Vanceril), flunisolide (AeroBid) or triamcinolone acetonide (Azmacort) Ideally, asthma should be controlled with an inhaled steroid that is used along with the bronchodilator. The more the inhaled steroid steroid controls the inflammation that causes the asthma, the less bronchodilator the patient needs to use because symptoms are under control.
Persons with diabetes should be aware that the bronchodilator epinephrine may raise their blood sugar levels.
Patients who are using an aerosol bronchodilator and an aerosol form of either ipratropium or a corticosteroid such as beclomethasone dipropionate (Beclovent, Vanceril) should use the bronchodilator first, then wait 5 minutes before using the other medicine. Check with a physician before using any other inhaled medications or other asthma medicines. The physician must determine the proper amount of time between doses.
Some bronchodilator products contain sulfites, that trigger an allergic reaction in certain people. Anyone who has a sulfite allergy should read the label carefully or check with a physician or pharmacist before using a bronchodilator. Call a physician immediately if any of these signs of an allergic reaction to sulfite occur:
- Bluish coloration of the skin
- Flushed or red face or skin
- Faintness
- Severe dizziness
- Increased wheezing or other breathing problems
- Skin rash, hives, or itching
- Swelling of the face, lips, or eyelids.
Special conditions
People with certain medical conditions or who are taking certain other medicines can have problems if they use bronchodilators. Before using these drugs, be sure to let the physician know about any of these conditions:
Allergies
Anyone who has had unusual reactions to any bronchodilator or an inhaled form of any other drug in the past should let his or her physician know before taking the drugs again. The physician should also be told about any allergies to foods, dyes, preservatives, or other substances.
Patients who are allergic to soybeans, soy lecithin, peanuts, or drugs based on atropine should not use the bronchodilator ipratropium (Atrovent).
Pregnancy
In studies of laboratory animals, some bronchodilators cause birth defects or miscarriage when the animals are given doses many times the usual human dose. Whether these drugs cause such problems in humans in unknown. Any woman who is pregnant or plans to become pregnant should check with her physician before using a bronchodilator.
Breastfeeding
Some bronchodilators pass into breast milk. Breastfeeding mothers should check with their physicians before using bronchodilators.
Other medical conditions
Before using bronchodilators, people with any of these medical problems should make sure their physicians are aware of their conditions:
- Glaucoma
- Brain damage
- Convulsions (seizures) -- recently or anytime in the past
- Mental illness
- Parkinson's disease
- Diabetes
- Heart or blood vessel diseases
- Rapid or irregular heartbeat
- High blood pressure
- Overactive thyroid
- Enlarged prostate
- Obstruction of the neck of the bladder.
Use of certain medicines
Using bronchodilators with certain other drugs may affect the way the drugs work or may increase the chance of side effects.
Side effects
Some patients have a dry or irritated throat or a dry mouth after using bronchodilators. To help prevent these problems, gargle and rinse the mouth or take a sip of water after each dose.
The most common side effects are nervousness or restlessness and trembling. These problems usually go away as the body adjusts to the drug and do not require medical treatment. Less common side effects, such as bad taste in the mouth, coughing, dizziness or lightheadedness, drowsiness, headache, sweating, fast or pounding heartbeat, muscle cramps or twitches, nausea, vomiting, diarrhea, sleep problems and weakness also may occur and do not need medical attention unless they do not go away or they interfere with normal activities.
More serious side effects are not common, but may occur. If any of the following side effects occur, check with the physician who prescribed the medicine as soon as possible:
- Chest pain or discomfort
- Irregular or fluttery heartbeat
- Unusual bruising
- Hives or rash
- Swelling
- Wheezing or other breathing problems
- Numbness in the hands or feet
- Blurred vision.
Other side effects are possible. Anyone who has unusual symptoms after using a bronchodilator should get in touch with his or her physician.
Interactions
Bronchodilators may interact with a number of other medicines. When this happens, the effects of one or both of the drugs may change or the risk of side effects may be greater. Anyone who takes these drugs should let the physician know all other medicines he or she is taking. Among the drugs that may interact with bronchodilators are:
- Monoamine oxidase inhibitors (MAO inhibitors) such as phenelzine (Nardil) and tranylcypromine (Parnate), used to treat depression
- Other bronchodilators
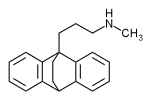
- Tricyclic antidepressants such as amitriptyline (Elavil) and imipramine (Tofranil)
- Beta blockers such as propranolol (Inderal) and atenolol (Tenormin), used to control high blood pressure
- Digitalis medicines, used to treat heart conditions, such as digoxin (Lanoxin)
- Drugs, such as certain diuretics (water pills), that lower potassium levels
- Ergoloid mesylates such as Hydergine, used to treat symptoms of Alzheimer's disease or multiple small stokes
- Ergotamine (Cafergot, Ergostat, and other brands), used to treat migraine and cluster headaches
- The antidepressant maprotiline (Ludiomil).
The list above does not include every drug that may interact with bronchodilators. Be sure to check with a physician or pharmacist before combining bronchodilators with any other prescription or nonprescription (over-the-counter) medicine.
Key Terms
- Anti-inflammatory
- Medicine used to relieve swelling, pain, and other symptoms of inflammation.
- Bronchitis
- Inflammation of the air passages of the lungs.
- Chronic
- A word used to describe a long-lasting condition. Chronic conditions often develop gradually and involve slow changes.
- Emphysema
- A lung disease in which breathing becomes difficult.
- Inflammation
- Pain, redness, swelling, and heat that usually develop in response to injury or illness.
- Nebulizer
- A device that turns liquid forms of medicine into a fine spray that can be inhaled.
- Sulfite
- A type of preservative that causes allergic reactions in some people.
Further Reading
For Your Information
Periodicals
- Fackelmann, Kathy A. "Anti-inflammatory drugs may quell asthma." (Discusses overuse of bronchodilators) Science News (September 26, 1992): 197.
Organizations
- Asthma and Allergy Foundation of America. 1125 15th Street NW, Suite 502, Washington, DC 20005. (800) 727-8462. http://www.aafa.org.
- American Academy of Allergy, Asthma and Immunology. 611 East Wells Street, Milwaukee, WI 53202. (414) 272-6071. http://www.aaaai.org/.
- National Heart, Lung and Blood Institute. National Institutes of Health, P.O. Box 30105, Bethesda, MD 20824-0105. (301) 251-1222. http://www.nhlbi.nih.gov/nhlbi/nhlbi.htm.
Gale Encyclopedia of Medicine. Gale Research, 1999.