Study objectives: To evaluate the effect of adding zatirlukast or low-dose theophylline to a beclomethasone dipropionate (BDP) extra-fine hydrofluoroalkane aerosol on bronchial hyperresponsiveness as the primary outcome variable.
Methods: Twenty-four patients with mild-to-moderate asthma were studied using a randomized crossover design with the following three treatment blocks: (1) beclomethasone, 100 [micro]g/d, alone for the first 2 weeks followed by 400 [micro]g/d alone for the next 2 weeks; (2) beclomethasone, 100 [micro]g/d, followed by 400 [micro]g/d, with the addition of zafirlukast, 20 mg bid; (3) beclomethasone, 100 [micro]g/d, followed by 400 [micro]g/d, with the addition of theophylline, 200 to 300 mg bid. Measurements were made after 2 and 4 weeks of each treatment and at pretreatment baseline.
Results: The mean trough plasma theophylline concentration was 6.7 mg/L, coinciding with the anti-inflammatory target range (ie, 5 to 10 mg/L). The provocative dose of methacholine causing a 20% fall in FE[V.sub.1] (as doubling dose difference from baseline) was significantly (p < 0.05) greater with beclomethasone, 100 [micro]g, plus zafirlukast (1.1 doubling dose) but not with beclomethasone, 100 [micro]g, plus theophylline (0.7 doubling dose) compared to beclomethasone, 100 [micro]g alone (0.4 doubling dose), but not compared to beclomethasone, 400 [micro]g alone (1.1 doubling dose). There were also significant (p < 0.05) differences between beclomethasone, 100 [micro]g, plus zafirlukast (but not BDP, 100 [micro]g, plus theophylline) vs beclomethasone, 100 [micro]g, alone in terms of nitric oxide level, midexpiratory phase of forced expiratory flow, and peak expiratory flow. There were no further significant improvements observed with the addition of zafirlukast or theophylline to beclomethasone, 400 [micro]g.
Conclusions: A leukotriene receptor antagonist, but not low-dose theophylline, conferred significant additive anti-inflammatory effects to therapy with a low-dose inhaled corticosteroid but not to that with a medium dose of an inhaled corticosteroid. Thus, optimizing the dose of inhaled corticosteroid as monotherapy would seem to be the logical first step, which is in keeping with current guidelines.
Key words: airway hyperresponsiveness; asthma; beclomethasone; theophylline; zafirlukast
Abbreviations: BDP = beclomethasone dipropionate; CI = confidence interval; CV = coefficient of variation; HFA = hydrofluoroalkane; ICAM = intercellular adhesion molecule; NO = nitric oxide; P[D.sub.20] = provocative dose of a substance causing a 20% fall in FE[V.sub.1]
**********
Asthma is recognized to be a chronic inflammatory disorder of the airways, with many cells and cellular elements playing a role. (1) Inflammation occurs throughout the lungs, extending from proximal airways through to alveolar tissue. (2-4) This airway inflammation can be detected early in the course of the disease, often before patients have noted symptoms. (5,6) Consequently, early recognition of airway inflammation may afford the opportunity for therapeutic intervention, thereby preventing irreversible airway remodeling. (7,8)
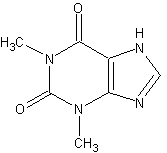
Therapeutic strategies are available to target inflammation present in the small airways. (9) These may be reached systemically, using tablet therapies such as oral theophyllines or leukotriene receptor antagonists, both of which are believed to have a combination of weak anti-inflammatory and bronchodilatory effects. (10,11) Alternatively, with the development of extrafine hydrofluoroalkane (HFA) corticosteroid aerosols, it is now possible to target the small airways more effectively using topical therapy. (12)
Inhaled corticosteroids currently remain the "gold standard" in topical anti-inflammatory therapy, and this is reflected in their positioning in UK and US asthma management guidelines, for patients with mild, moderate, and severe persistent asthma. (1,13) Nevertheless, it is also recognized that long-term treatment with high doses of inhaled corticosteroids may result in the potential for systemic adverse effects. (14)
The aim of this study was to evaluate the effects of adding either low-dose oral theophylline or leukotriene receptor antagonist to the treatment of patients with persistent asthma, who already are receiving either a low-to-medium dose of an inhaled corticosteroid. We elected to use low-dose theophylline in order to achieve trough plasma levels to coincide with the modern anti-inflammatory target range of 5 to 10 mg/L. Bronchial hyperresponsiveness to methacholine challenge was chosen a priori as the primary outcome variable as it is considered to reflect the underlying inflammatory process in asthma and is more sensitive than conventional lung function variables in patients with mild-to-moderate disease.
MATERIALS AND METHODS
Patients
Patients who were recruited were between the ages of 18 and 65 years, with an established diagnosis of mild-moderate persistent asthma requiring prior inhaled steroid use of [less than or equal to] 1000 [micro]g budesonide/beclomethasone dipropionate (BDP) or [less than or equal to] 500 [micro]g fluticasone propionate daily. They were required to have an FE[V.sub.1] of at least 70% of the predicted normal value at screening and were required to exhibit hyperresponsiveness to methacholine challenge in terms of a provocative dose of a substance (ie, methacholine) causing a 20% fall in FE[V.sub.1] (P[D.sub.20]) of < 500 [micro]g (which is equivalent to a provocative concentration of methacholine causing a 20% fall in FE[V.sub.1] of < 5 mg/mL). The Tayside Medical Ethics Committee granted ethical approval to the study, and informed, written consent was obtained from all patients.
Study Design
The study had a randomized, placebo-controlled, single-blind, double-dummy, three-way crossover design. Following an initial screening visit, all eligible patients entered a 7 to 10 days placebo run-in. Thereafter, in randomized sequence, each patient received 4 weeks of active treatment, each active treatment being preceded by or separated by either placebo run-in or washout (Fig 1). The three active treatments were as follows:
1. BDP HFA 134a formulation (QVAR Autohaler; 3M Health Care Ltd; Loughborough, UK; 50 [micro]g/100 [micro]g per actuation) at low dose (50 [micro]g bid as 1 puff bid) for the first 2 weeks followed by an increased dose (200 [micro]g bid as 2 puffs bid) for the next 2 weeks, with a placebo tablet given twice daily throughout the 4 weeks.
2. BDP HFA, 50 [micro]g bid for the first 2 weeks followed by 200 [micro]g bid for the next 2 weeks, but in addition zafirlukast (Accolate; AstraZeneca; King's Langley, UK; 20 mg per tablet), 1 tablet twice daily (ie, 40 mg daily given throughout the 4 weeks).
3. BDP HFA, 50 [micro]g bid for the first 2 weeks followed by 200 [micro]g bid for the next 2 weeks, but in addition theophylline (Uniphyllin Continuous sustained release 200-mg or 300-mg tablets; Napp Pharmaceuticals; Cambridge, UK), one tablet (ie, 200 or 300 mg twice daily throughout the 4 weeks [the 300-mg dose was only for patients weighing > 80 kg, and these patients received 200 mg bid for first week and the higher 300-mg dose bid for the remaining 3 weeks]).
[FIGURE 1 OMITTED]
Measurements
Screening Visit: Patients had methacholine P[D.sub.20] measured on two separate visits to assess the protection afforded 30 min after a 400-[micro]g dose of albuterol (Ventolin Accuhaler [200 [micro]g per actuation]; Glaxo Wellcome UK Ltd; Uxbridge, UK). The inhaler technique was assessed using a placebo inhaler and a checking device (In-check; Clement Clarke International Ltd; Harlow, UK).
Study Visits: At all visits, diary cards were reviewed and measurements were made of spirometry, exhaled nitric oxide (NO) concentration, methacholine bronchial challenge, and overnight (ie, 10:00 PM to 8:00 AM) urinary cortisol/creatinine levels. At selected visits, blood was taken for measurement of eosinophil levels, liver function, vascular cell adhesion molecule levels, and theophylline concentrations (visits 1, 3, 4, 6, 7, and 9). Patients withheld from taking their study medication on the morning of the laboratory visit, so all measurements were made at trough (ie, approximately 12 h after their preceding evening dose was received). Methacholine challenge was performed according to guidelines using a validated computer-assisted dosimetric method. (15,16) The exhaled-breath NO level was measured according to recommended guidelines using an integrated clinical real-time NO gas analyzer (model LR2000; Logan Research; Rochester, UK) with an accuracy of 2 parts per billion NO with a response time of 2 s. (17) Patients filled in a domiciliary diary card daily (ie, morning and evening) throughout the entire study to measure peak flow, asthma symptoms, (scale, 0 to 4) and rescue short-acting [[beta].sub.2]-agonist requirements.
Blood/Urine Measurements: The peripheral blood eosinophil counts were measured using a hematology analyzer (model SE-9000; Sysmex UK Ltd; Bucks, UK). Liver function tests (ie, for alanine transaminase, alkaline phosphatase, and bilirubin levels) were measured using an automated biochemistry analyzer (Hitachi 917; Roche Diagnostics Ltd; Sussex, UK). Plasma E-selectin and intercellular adhesion molecule (ICAM)-1 levels were measured by enzyme immunoassays (R&D Systems; UK). The within-assay coefficient of variation for E-selectin and ICAM-1 were 1.0% and 2.7%, respectively. Urinary cortisol was assayed with a commercial radioimmunoassay kit (Incstar Ltd; Berkshire, UK). The coefficient of variation (CV) for analytical imprecision for urinary free cortisol was 5.5% within the assay, and 6.4% between assays. The urinary creatinine level was measured on an autoanalyzer (Cobas-bio; Roche Products Ltd; Hertsfordshire, UK). The within-assay CV was 1.0%, and the between-assay CV was 1.0%.
Statistical Analysis
The study was designed with at least 80% power to detect a one doubling-dose difference in methacholine P[D.sub.20] (the primary end point) between treatments using a crossover design. The logarithmic transformation of the data for methacholine P[D.sub.20], blood eosinophil level, and overnight urinary cortisol level was required in order to normalize the distribution. Analysis was performed on the 24 patients who completed all visits per protocol, with an initial comparison being made of placebo baseline values prior to each treatment. Multifactorial analysis of variance and Bonferroni multiple-range testing were used to compare within-treatment and between-treatment effects after 2 and 4 weeks of active treatments. Between-treatment comparisons were made in terms of the change from the respective placebo pretreatment baseline value. Within-treatment comparisons were made by comparing values after 2 and 4 weeks with the respective pretreatment baseline.
RESULTS
Patients
Thirty-two patients fulfilled the inclusion criteria at the initial screening visit and entered the placebo run-in prior to randomization. Of these patients, four were unable to tolerate the placebo run-in prior to randomization at visit 1 because of worsening asthma symptoms. Thus, 28 patients were randomized to receive active treatments in crossover fashion. Of these 28 patients, 3 were withdrawn from the study following asthma exacerbation, and 1 was withdrawn from the study following an episode of intolerance to theophylline (ie, nausea). Thus, 24 patients completed the study in total, and their demographic data are summarized in Table 1. At screening, on two separate visits, patients exhibited a 4.4 (95% confidence interval [CI], 3.5 to 5.3) doubling-dose difference in methacholine P[D.sub.20] comparing reversibility for before vs after albuterol administration, 400 [micro]g.
No significant differences in pretreatment (placebo) baseline values for any end points were seen analyzed according to either treatment (Table 2) or sequence (data not shown). The mean (SE) plasma theophylline concentration at trough was 37 [micro]mol/L (3.1 [micro]mol/L [equivalent to 6.7 mg/L]) after 4 weeks when patients were randomized to receive theophylline.
Bronchial Hyperresponsiveness to Methacholine
Significant (p < 0.05) bronchoprotection was seen within each active treatment group, compared to the respective placebo pretreatment baseline P[D.sub.20] value. For patients treated with beclomethasone monotherapy, this improvement in P[D.sub.20] was significant (p < 0.05) only at the 400-[micro]g dose, whereas with the addition of theophylline or zafirlukast, significant (p < 0.05) bronchoprotection was seen with 100-[micro]g and 400-[micro]g doses of beclomethasone.
For between-treatment comparisons (Fig 2) given as the doubling-dose difference from pretreatment baseline, there was a significantly greater (p < 0.05) improvement in P[D.sub.20] with beclomethasone, 100 [micro]g, plus zafirlukast (1.1 doubling dose), but not with beclomethasone, 100 [micro]g, plus theophylline (0.7 doubling dose), vs beclomethasone, 100 [micro]g, alone (0.4 doubling dose) but not vs beclomethasone, 400 [micro]g, alone (1.1 doubling dose).
[FIGURE 2 OMITTED]
Inflammatory Surrogates
Significant (p < 0.05) suppression of exhaled breath NO was seen within each active treatment group, compared to the respective pretreatment placebo baseline (Fig 3). At beclomethasone, 100 [micro]g, significant (p < 0.05) suppression of NO was seen only in those patients treated with additive zafirlukast, whereas with beclomethasone, 400 [micro]g, significant suppression occurred in all three groups.
[FIGURE 3 OMITTED]
For between-treatment comparisons given as the percentage change from pretreatment baseline, there was a significantly (p < 0.05) greater fall in NO with beclomethasone, 100 [micro]g, plus zafirlukast (48% fall), but not beclomethasone, 100 [micro]g, plus theophylline (34% fall), vs beclomethasone, 100 [micro]g, alone (32% fall) but not vs beclomethasone, 400 [micro]g, alone (50% fall).
Circulating E-selectin levels (only measured at 4 weeks) were significantly (p < 0.05) suppressed with all three active treatments among patients who received beclomethasone, 400 [micro]g, compared to pretreatment placebo baseline values. Circulating ICAM-1 levels (only measured at 4 weeks) were significantly suppressed vs baseline values only within the group receiving zafirlukast in addition to beclomethasone, 400 [micro]g. Significant (p < 0.05) suppression of blood eosinophils (only measured at 4 weeks) was seen in patients receiving beclomethasone, 400 [micro]g, either as monotherapy or with theophylline vs placebo baseline. There were no significant differences in the change from baseline values among the three treatments for any of the above parameters.
Spirometry and Peak Flow Measurements
Significant (p < 0.05) improvements in spirometry and peak flow occurred within all three treatment groups, compared to the pretreatment placebo baseline (Table 3). The effect of beclomethasone monotherapy on spirometry and morning peak flow was significant only for the 400-[micro]g dose, whereas with the addition of zafirlukast there were significant improvements in the 100-[micro]g and 400-[micro]g doses of beclomethasone. With the addition of theophylline to beclomethasone, 100 [micro]g, only the midexpiratory forced expiratory flow rate showed a significant (p < 0.05) within-treatment improvement compared to baseline. For between-treatment comparisons, such as the change from baseline, there were significantly (p < 0.05) greater improvements in midexpiratory forced expiratory flow and peak flow (morning and evening) with beclomethasone, 100 [micro]g, plus zafirlukast (but not theophylline) vs beclomethasone, 100 [micro]g, alone.
Symptoms and [[beta].sub.2]-Agonist Use
Significant (p < 0.05) improvements were seen within each active treatment group, compared to baseline. Although there were no significant differences between treatments as such, it can be seen that the addition of zafirlukast improved more diary card parameters, compared to baseline, in patients receiving beclomethasone, 100 [micro]g.
Overnight Urinary Cortisol/Creatinine
No significant differences were noted in overnight urinary cortisol corrected for creatinine excretion. Geometric mean pooled values (n = 72) were as follows: placebo, 3.9 nmol/mmol (95% CI, 3.4 to 4.5); beclomethasone (100 [micro]g), 4.1 nmol/mmol (95% CI, 3.5 to 4.7); beclomethasone (400 [micro]g), 3.3 nmol/ mmol (2.9 to 3.8).
DISCUSSION
Our study showed that adding a leukotriene receptor antagonist to a low dose of an inhaled corticosteroid resulted in improvements in different parameters of antiasthma activity. The combination of a leukotriene receptor antagonist, but not low-dose theophylline, with a low dose of inhaled corticosteroid conferred greater effects on inflammatory surrogates (such as methacholine P[D.sub.20] and exhaled NO levels) compared to a low dose of inhaled corticosteroid (beclomethasone, 100 [micro]g/d) alone but not compared to a medium dose of inhaled corticosteroid (beclomethasone, 400 [micro]g/d) alone. For example, there was the same 1.1 doubling-dose shift in methacholine P[D.sub.20] with beclomethasone, 100 [micro]g, plus zafirlukast or beclomethasone, 400 [micro]g, alone. Adding a leukotriene receptor antagonist or theophylline to treatment conferred no additional benefit to a medium dose of an inhaled corticosteroid used as monotherapy. A 1.0 doubling-dose shift in bronchial hyperresponsiveness would normally be considered a clinically relevant improvement. The 400-[micro]g dose of beclomethasone was not associated with significant systemic suppression of overnight urinary cortisol excretion corrected for creatinine. These findings emphasize the importance of first optimizing the dose of inhaled corticosteroid before considering adding a second-line therapy with a leukotriene receptor antagonist or theophylline. Furthermore, the UK drug costs (9.64 [pounds sterling]) for 28 days of monotherapy with HFA BDP, 400 [micro]g/d, is considerably less than the combination of HFA beclomethasone, 100 [micro]g/d (2.20 [pounds sterling]) and zafirlukast, 40 mg/d, (25.69 [pounds sterling]). There is also the issue of compliance with multiple therapies, which might assume relevance in the long term.
Since inhaled or oral corticosteroids have not been shown to attenuate leukotriene production in vivo, (18,19) it is perhaps not surprising that using a leukotriene receptor antagonist in patients already receiving low-dose inhaled corticosteroids may confer additional benefits. This is supported by studies comparing the additive effects either of zafirlukast or montelukast compared to placebo in patients already receiving inhaled corticosteroids. (20-22) In particular, in one of these studies in patients with mild-to-moderate persistent asthma, zafirlukast was found to significantly reduce bronchial hyperresponsiveness to methacholine and exhaled NO when given in addition to a low-to-moderate dose of an inhaled corticosteroid, as was the case in our study. (22) Other studies (23,24) also have suggested indirectly that leukotriene receptor antagonists provide complementary benefits to inhaled corticosteroid therapy and may even facilitate dose reduction of the latter.
Analogous to leukotriene receptor antagonist therapy, theophylline also is recognized as possessing both bronchodilatory and anti-inflammatory properties. (25,26) Beneficial immunomodulatory effects may be seen at serum theophylline concentrations below those traditionally regarded as therapeutically useful in terms of achieving bronchodilatation (ie, 10 to 20 mg/L). Our mean trough theophylline level was 6.7 mg/L, which would coincide with the more modern anti-inflammatory target range of 5 to 10 mg/L. We elected to use low-dose theophylline in order to assess whether it exhibited additive effects to an inhaled corticosteroid in terms of surrogate inflammatory markers. In this respect, our patients had only mildly impaired lung function, and so significant bronchodilator responses would not be expected with low-dose theophylline therapy. The addition of theophylline to therapy with an inhaled steroid in patients with more severe asthma has been shown to be beneficial in several studies. (27-29)
Our choice of primary end point, bronchial hyperresponsiveness to methacholine challenge, is of clinical relevance. While the link between airways inflammation and bronchial hyperresponsiveness is not a simple one, one study (30) has demonstrated that reducing bronchial hyperresponsiveness to methacholine, in conjunction with optimizing symptoms and lung function for > 2 years, leads to more effective control of asthma and to a reduced number of exacerbations, reducing airway remodeling as assessed in bronchial biopsy specimens. Other data also have suggested that methacholine P[D.sub.20] may be a good surrogate for airway inflammation and disease severity. (31,32) Furthermore, the dose response to inhaled steroids in patients with mild-to-moderate asthma is much steeper for bronchial hyperresponsiveness than for lung function. (33)
Exhaled breath NO is recognized to be a sensitive marker of cytokine-driven airway inflammation. Significantly greater suppression of NO was seen with zafirlukast, but not theophylline, in conjunction with low-dose beclomethasone, in comparison to low-dose beclomethasone alone. This effect was not seen with zafirlukast when given in combination with the medium dose of beclomethasone. This is not surprising given that we know that near-maximal suppression of exhaled breath NO occurs with modest doses of inhaled corticosteroids. (33) We also observed significant suppression of circulating E-selectin following all treatments compared to placebo. E-selectin is a vascular cell adhesion molecule that is involved in the endothelial transmigration of inflammatory cells into the lungs. Of note, it is found only on activated endothelium, in contrast to other adhesion molecules. Elevated levels previously have been reported in patients with acute asthma and may reflect the extensive inflammatory response occurring in the airways during acute exacerbations. (34)
In a previous study using the same extra-fine particle HFA formulation of BDP, the effects of 100 [micro]g/d on spirometry were near maximal after 1 week compared to 6 weeks. (35) However, much longer periods may be needed to achieve peak effects on bronchial hyperresponsiveness. Hence, the greater response to beclomethasone, 400 [micro]g, than to beclomethasone, 100 [micro]g, in terms of methacholine P[D.sub.20] in our study may not merely be a function of dose, but also may be due to duration of therapy (ie, 4 weeks compared to 2 weeks). It is also possible that our results may only apply to the extra-fine HFA formulation of BDP in terms of being able to target the inflammatory process in the small airways. (12) It is therefore conceivable that with a coarser particle formulation, the additive effects of zafirlukast or theophylline might be seen at low or medium doses of the inhaled corticosteroid. In this respect, with conventional chlorofluorocarbon beclomethasone, 400 [micro]g/d, improvements in asthma control were seen with the addition of montelukast. (20)
In summary, a leukotriene receptor antagonist, but not low-dose theophylline, conferred significant additive anti-inflammatory effects to low-dose inhaled corticosteroid therapy, but not to medium-dose inhaled corticosteroid therapy. Our results reinforce the view that inhaled corticosteroids should be used as first-line anti-inflammatory therapy in the management of patients with persistent asthma. Second-line nonsteroidal agents, particularly leukotriene receptor antagonists, may still be useful as add-on therapy, however, although optimizing the dose of inhaled corticosteroid as monotherapy would seem to be the logical first step, in keeping with current asthma management guidelines.
ACKNOWLEDGMENT: The authors thank Lesley McFarlane for performing the cortisol assays, Michelle Paterson for nursing support, and Richard Brown for statistical advice.
REFERENCES
(1) National Asthma Education, and Prevention Program. Expert panel report 2: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Institutes of Health; April 1997; Publication No. 97-4051
(2) Kraft M, Djukanovic R, Wilson S, et al. Alveolar tissue inflammation in asthma. Am J Respir Crit Care Med 1996; 154:1505-1510
(3) Roche WR. Inflammatory and structural changes in the small airways in bronchial asthma. Am J Respir Crit Care Med 1998; 157:S191-S194
(4) Kraft M, Martin RJ, Wilson S, et al. Lymphocyte and eosinophil influx into alveolar tissue in nocturnal asthma. Am J Respir Crit Care Med 1999; 159:228-234
(5) Laitinen LA, Laitinen A, Haahtela T. Airway mucosal inflammation even in patients with newly diagnosed asthma. Am Rev Respir Dis 1993; 147:697-704
(6) Vignola AM, Chanez P, Campbell AM, et al. Airway inflammation in mild intermittent and in persistent asthma. Am J Respir Crit Care Med 1998; 157:403-409
(7) Lange P, Parner J, Vestbo J, et al. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med 1998; 339:1194-1200
(8) Chetta A, Foresi A, Del Donno M, et al. Airways remodeling is a distinctive feature of asthma and is related to severity of disease. Chest 1997; 11:852-857
(9) Thompson PJ. Drug delivery to the small airways. Am J Respir Crit Care Med 1998; 157:S199-S202
(10) Lipworth BJ. Leukotriene-receptor antagonists. Lancet 1999; 353:57-62
(11) Spina D, Landells LJ, Page CP. The role of theophylline and phosphodiesterase 4 isoenzyme inhibitors as anti-inflammatory drugs. Clin Exp Allergy 1998; 28(suppl):24-34
(12) Lipworth BJ. Targets for inhaled treatment. Respir Med 2000; 94(suppl):S13-S16
(13) British Thoracic Society. The British guidelines on asthma management: 1995 review and position statement. Thorax 1997; 52:S1-S21
(14) Lipworth BJ. Systemic adverse effects of inhaled corticosteroid therapy: a systematic review and meta-analysis. Arch Intern Med 1999; 159:941-955
(15) Crapo RO, Casaburi R, Coates AL, et al. Guidelines for methacholine and exercise challenge testing-1999. Am J Respir Crit Care Med 2000; 161:309-329
(16) Beach JR, Young CL, Avery AJ, et al. Measurement of airway responsiveness to methacholine: relative importance of the precision of drug delivery and the method of assessing response. Thorax 1993; 48:239-243
(17) Kharitonov S, Alving K, Barnes PJ. Exhaled and nasal nitric oxide measurements: recommendations: the European Respiratory Society Task Force. Eur Respir J 1997; 10:1683-1693
(18) O'Shaughnessy KM, Wellings R, Gillies B, et al. Differential effects of fluticasone propionate on allergen-evoked bronchoconstriction and increased urinary leukotriene [E.sub.4] excretion. Am Rev Respir Dis 1993; 147:142-146
(19) Dworski R, Fitzgerald GA, Oats JA, et al. Effect of oral prednisolone on airway inflammatory mediators in atopic asthma. Am J Respir Crit Care Med 1994; 149:953-959
(20) Laviolette M, Malmstrom K, Lu S, et al. Montelukast added to inhaled beclomethasone in treatment of asthma. Am J Respir Crit Care Med 1999; 160:1862-1868
(21) Virchow CJ, Prasse A, Naya I, et al. Zafirlukast improves asthma control in patients receiving high-dose inhaled corticosteroids. Am J Respir Crit Care Med 2000; 162:578-585
(22) Lipworth BJ, Dempsey OJ, Aziz I, et al. Effects of adding in a leukotriene receptor antagonist or a long acting [beta.sub.2]-agonist in asthmatic patients with the glycine-16 [beta.sub.2]-adrenoceptor genotype. Am J Med 2000; 109:114-121
(23) Tamaoki J, Kondo M, Sakai N, et al. Leukotriene antagonist prevents exacerbation of asthma during reduction of high-dose inhaled corticosteroid. Am J Respir Crit Care Med 1997; 155:1235-1240
(24) Lofdahl CG, Reiss TF, Left JA, et al. Randomized, placebo controlled trial of effect of a leukotriene receptor antagonist, montelukast, on tapering inhaled corticosteroids in asthmatic patients. BMJ 1999; 319:87-90
(25) Sullivan P, Bekir S, Jaffar Z, et al. Anti-inflammatory effects of low-dose oral theophylline in atopic asthma. Lancet 1994; 343:1006-1008
(26) Kidney J, Dominguez M, Taylor PM, et al. Immunomodulation by theophylline in asthma: demonstration by withdrawal of therapy. Am J Respir Crit Care Med 1995; 151:1907-1914
(27) Evans DJ, Taylor DA, Zetterstrom O, et al. A comparison of low-dose inhaled budesonide plus theophylline and high-dose inhaled budesonide for moderate asthma. N Engl J Med 1997; 337:1412-1418
(28) Ukena D, Harnest U, Sakalauskas R, et al. Comparison of addition of theophylline to inhaled steroid with doubling of the dose of inhaled steroid in asthma. Eur Respir J 1997; 10:2754-2760
(29) Rivington RN, Boulet LP, Cote J, et al. Efficacy of Uniphyl, salbutamol, and their combination in asthmatic patients on high-dose inhaled steroids. Am J Respir Crit Care Med 1995; 151:325-332
(30) Sont JK, Willems LN, Bel EH, et al. Clinical control and histopathologic outcome of asthma when using airway hyperresponsiveness as an additional guide to long-term treatment. Am J Respir Crit Care Med 1999; 159:1043-1051
(31) Laprise C, Laviolette M, Boutet M, et al. Asymptomatic airway hyperresponsiveness: relationships with airway inflammation and remodelling. Eur Respir J 1999; 14:63-73
(32) Weiss ST, Van Natta ML, Zeiger RS. Relationship between increased airway responsiveness and asthma severity in the childhood asthma management program. Am J Respir Crit Care Med 2000; 162:50-56
(33) Wilson AM, Lipworth BJ. Dose-response evaluation of the therapeutic index for inhaled budesonide in mild to moderate atopic asthmatic patients. Am J Med 2000; 108:269-275
(34) Montefort S, Lai CK, Kapahi P, et al. Circulating adhesion molecules in asthma. Am J Respir Crit Care Med 1994; 149:1149-1152
(35) Busse WW, Brazinsky S, Jacobson K, et al. Efficacy response of inhaled beclomethasone dipropionate in asthma is proportional to dose and is improved by formulation with a new propellant. J Allergy Clin Immunol 1999; 104:1215-1222
* From the Asthma and Allergy Research Group (Drs. Dempsey, Fowler, Wilson, and Lipworth), Department of Clinical Pharmacology & Therapeutics, and the Department of Medicine (Dr. Kennedy), Section of Vascular Medicine & Biology, Ninewells Hospital and Medical School, University of Dundee, Dundee, Scotland, UK.
This study received no pharmaceutical financial support and was funded by an Anonymous Trust University of Dundee research grant and by a grant from TENOVUS (registered charity SC009675, Glasgow, UK). Drs. Lipworth, Dempsey, Fowler, and Wilson have received financial support from 3M Healthcare (Loughborough, UK) for attending postgraduate educational meetings. Dr. Lipworth has received support from 3M Healthcare for giving occasional educational talks. 3M Healthcare supplied QVAR and placebo inhalers, and Glaxo-Wellcome Ltd (Uxbridge, UK) supplied Ventolin inhalers.
Manuscript received July 25, 2001; accepted January 3, 2002.
Correspondence to: Brian J. Lipworth, MD, Professor of Allergy and Pulmonology, Asthma and Allergy Research Group, Department of Clinical Pharmacology & Therapeutics, Ninewells Hospital and Medical School, University of Dundee, Dundee DD1 9SY, Scotland; e-mail: bj.lipworth@dundee.ac.uk
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group