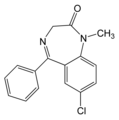
Valium
Diazepam, market under brand names of: Valium, Seduxen; and in Europe Apozepam, Diapam, is a 1,4-benzodiazepine derivative, which possesses anxiolytic, anticonvulsant, sedative and skeletal muscle relaxant properties. Diazepam is used to treat anxiety and tension, and is the most effective benzodiazepine for treating muscle spasms. It is also used as a sedative premedication for various medical procedures, and to treat alcohol and opiate withdrawal symptoms. Occasionally, diazepam is used by military and paramilitary snipers to relax muscles and slow breathing for increased firing accuracy. Diazepam is a Schedule IV drug under the Convention on Psychotropic Substances. more...
Diazepam is one of the 'standard benzodiazepines' most often used in clinics and for outpatients. It is enrolled in the WHO List of 'Essential Drugs'.
When introduced in 1963, it was the best of the new alternatives to barbiturates, drugs that could be deadly with an overdose. Diazepam (like the other benzodiazepines) did not have this danger, nor immediately obvious side effects, and became in widespread use to treat chronic anxiety. Diazepam was America's top-selling drug from 1969 to 1982, with peak sales in 1978 of 2.3 billion pills ($US600 million in sales).
However, it is now recognised that the drug is not as harmless as was first assumed. In the autumn of 1973, a report aired on the television show 60 Minutes attesting to the drug's addictiveness. This can occur in as little as four weeks. Following controversial and often polemic discussion prescriptions declined by nearly half in the 1980's and 1990's. Surprisingly, psychiatrists and neurologists have recently discovered new therapeutic fields for this 'old' drug diazepam (e.g. adjunctive treatment of extrapyramidal disorders, some forms of anxiety in children, and adjunctive treatment of spastic paresis); a process still ongoing.
Mode of action
In animals, diazepam appears to act on parts of the limbic system, the thalamus and hypothalamus, and induces calming effects. It binds in to specific benzodiazepine receptors, which are part of the GABA-receptors. When diazepam binds to this receptor, it causes an increase in the inhibitory effects of GABA. It is redistributed into tissues and fat deposits, and there is an adaptation of benzodiazepine receptors. In humans, tolerance to the sedative effects may develop within weeks, but tolerance to the anxiolytic efficiacy usually does not develop. Lorazepam, clonazepam and alprazolam show stronger anxiolytic effects compared to diazepam, but the former 3 drugs carry a particular high risk of abuse, misuse and psychological dependence.
Pharmacokinetics
Diazepam can be administered orally, intravenously or intramuscularly, or as a suppository. When taken orally, diazepam is rapidly absorbed and shows a fast onset of action. Absorption is much slower and more erratic when diazepam is given as an intramuscular injection. Diazepam is highly lipid-soluble and therefore crosses the blood-brain barrier easily. Diazepam is metabolised in the liver and it has a biphasic half-life. The half-life (t1/2α) is 20-100 hours, and its main active metabolite, desmethyldiazepam, has a half-life of 2-5 days. Diazepam's other active metabolites include, among others, temazepam and oxazepam. Diazepam and its metabolites are excreted into the urine.
Read more at Wikipedia.org