IN MODERN LIFE, we each get to choose how to act and whom to be. This freedom can also be a curse, because we must make our choices based on approaches to doing and being that may be persuasive but are often in conflict. Our choices are centered on the stories we tell ourselves and the stories we are told; our challenge is to find good ways to choose among contradictory stories.
Such decisions are among the most basic challenges we face, because they become the foundation for a succession of other choices we make throughout our lives, often with no clearly right answers yet with long-term consequences. When we want to make the "right" decision about education, child rearing, or medicine, we must first sort out conflicting claims about what is true.
But while modern life offers us an abundance of compelling stories about what is best for us to do, it offers little guidance for finding our way through a thicket of equally plausible but often mutually contradictory points of view.
There are as many compelling illustrations of this issue as there are choices to make. The example I will use centers on a personal medical decision, but it involves far broader issues: social norms, approaches to choice, even identity. It is about mood medication.
Mother's Little Helper
I'm a prime candidate for such medication--female, entering menopause, with a full-time job and two active children. I've long been prone to bouts of sadness and lethargy. I usually answer yes to most of the depression screening questions found in women's magazines and drug company pamphlets. On top of my symptoms of depression, I have lots of anxiety; I'm definitely a worry-wart, imagining disasters of many kinds befalling me, my loved ones, and the world.
Plenty of experts have tried to convince me that I need mood medication. In the last 10 years my primary care physician, my gynecologist, and even my allergist's assistant have offered to get me prescriptions. I'm also being targeted by pharmaceutical companies with magazine and TV ads that describe me exactly and tell me that I can greet the dawn with gusto, romp with my children, smile at myself in the mirror, and be productive, cheerful, and optimistic ("like myself again") if I take their drugs. Why am I resisting taking mood medications, an option that millions of my fellow citizens have already chosen?
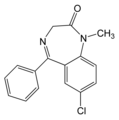
One reason I'm hesitant to take Prozac, Zoloft, Xanax, Celexa, Wellbutrin, or their like involves a related but complicating issue: alcoholism. Years ago, I quit drinking because I believed I was an alcoholic, and if this is true it makes taking even doctor-prescribed drugs problematic. When I was first struggling to control my alcohol use, I strongly resisted the alcoholic label. But my resistance was interpreted by a counselor as denial, which is a key element in the diagnosis of alcoholism. And as with those depression screening questions, I could answer yes to well over the minimum number of questions required for an official diagnosis of alcoholism.
Since even with my best efforts I was unable to control my drinking, I finally adopted the language and beliefs--what we in academic life call the discourse--of alcoholism recovery, including the conviction that the only way to control my addiction was to abstain completely from alcohol and other mood-altering substances. I've successfully abstained from these, one day at a time for more than 20 years.
Many in 12-step recovery circles believe that mood medication--20 years ago it was Librium, Valium, and tricyclic antidepressants--is just alcohol in pill firm. In the 1980s, lots of recovering alcoholics (more women than men) considered themselves dual addicts because they both drank and took pills. Recovering addicts were therefore considered to be one drink or drug away from active addiction. So if these beliefs are true, antidepressants are (for me, if I am indeed an addict) not useful medicine but dangerous drugs. Even everyday medicine--cough syrup, pain pills--could lead me back into active addiction, at least according to some members of the 12-step recovery community. So perhaps I am right to be especially-wary.
Yet today many recovering alcoholics make exceptions for doctor-prescribed medications. Even as they consider themselves recovering alcoholics, they are taking and feeling better on mood medication such as Prozac and stimulants such as Ritalin (taken for"adult attention deficit disorder"). These people believe they are treating medical conditions, not feeding their addiction. They believe prescription medication, taken when recommended by a doctor to treat a real illness, is not dangerous and does not lead to relapse.
Are they right? Previous generations of doctors happily prescribed the tranquilizers and pep pills--the Mother's Little Helpers--that brought many women into what they defined as active addiction. In my early sobriety, I heard harrowing tales of how hard it was for these women to learn to live without the pills that their doctors had prescribed for the same kinds of symptoms I struggle with today. And it turns out that today's new and improved mood medications are also difficult to quit, requiring a gradual weaning process much like other addictive drugs. How are Paxil, Zoloft, and Xanax any different from Miltown, Librium, and Valium, the pills many critics now denounce as addictive drugs used to keep women of the '50s and '60s passive and complacent?
Coming Down Again
If you believe the media coverage of the 1990s, the newer selective serotonin reuptake inhibitors (SSRIs) are unlike the drugs of the past because these new medications treat a chemical imbalance that causes the diseases of depression and anxiety. Many who take these medications believe they are correcting a brain chemical deficit. But this is a marketing model that misrepresents what neuroscientists currently know about brain chemistry and the reasons these drugs may work. On top of that, depression, anxiety, and even alcoholism aren't diseases like cancer of diabetes, even if it may be helpful to think of them this way.
There is plenty of controversy about whether alcoholism even exists of, if it does, if it really is a disease. The original use of the term disease in Alcoholics Anonymous was metaphorical, aimed at destigmatizing the condition and describing its relentless course if untreated. But alcoholism, along with anxiety and depression, has come to count as a disease in the diagnostic manuals used by psychotherapists and physicians. This means that at least for prescription and insurance purposes, they are diseases. Yet this pathologizing of elements of human experience begs the question: What makes heavy drug or alcohol use, long-term sadness, or heightened anxiety a disease?
And what constitutes addiction? Most of us are dependent on something, and in the last few decades people have learned to define themselves as gambling addicts, sex addicts, food addicts, exercise addicts, television addicts, and so on. For all the claims about how "nonaddictive" current mood medications are, the mounting evidence suggests otherwise, since most long-term users feel dependent on them and cannot easily stop using them. And although the American Psychiatric Association says withdrawal effects like those experienced by people who abruptly stop using SSRIs are neither necessary nor sufficient for a diagnosis of "substance dependence" such symptoms traditionally were seen as the hallmarks of addiction.
Furthermore, for all my commitment to continued sobriety, I'm far from "drug free" today if you count caffeine, as we should, as a mood-altering substance. I carry a Thermos of strong tea with me every day, carefully doling out my cups to avoid getting a pounding headache. How is this different from carrying a small flask of medicinal whiskey? Aren't caffeine and nicotine as addictive (if addiction exists) as alcohol and heroin, if not more so?
So are popular products like Prozac, Paxil, Zoloft, Xanax, and Celexa best understood as drugs that change us or as medicines that cure us? What makes them one or the other, beyond social convention and a doctor's prescription?
There's another twist. I have spent most of my life learning how to cope with my moods. I'm deeply invested in figuring out how to glean something useful from my depressions as well as learning how to manage and make the most of my periods of elation. I have found ways to minimize the damage and disruption that my periods of gloom and nameless grief can cause. My moodiness is--and has always been--my "self." Perhaps there's some benefit to living with, rather than medicating, my temperament. I've certainly learned a lot about the range of ways reality can feel. What does it mean for me to start defining myself as "mood-disordered" or "chemically imbalanced" or "borderline personality disordered" or "ADHD"?
By whose story should I live? Am I simply an especially emotionally responsive person, or have I squandered most of my life trying to compensate for biological dysfunctions that modern medicine now allows me to correct?
When it comes to deciding if I should medicate my moods, I am, as we say in my academic field, situated at the intersection of conflicting discourses. But this is true for all of us, with of without mood swings, possible addictions, or persuasive physicians. The invention and marketing of medications that seem to alleviate symptoms of depression and anxiety make it possible for every one of us to choose to take what some would call drugs and others would call medicine, to become (depending on your point of view) an addict, or your old self, or even a preferable self. We are all faced with this choice, as well as many others. How do we choose well?
Three overlapping but conflicting discourses operate whenever we think about taking pills to influence our emotions--discourses of addiction, of neuroscience, and of mental health. Each of these has its own opposition, a discourse that challenges all its premises. If I want to choose wisely about taking or not taking antidepressants, I have to find my way not only through each of these three discourses, each with different evidence and assumptions, but through three additional discourses--the ones that challenge that evidence and those assumptions.
This is a daunting project, but I think it is fairly typical of what modern life asks of each of us. We are always being asked to choose among conflicting stories. The dominant challenge of the modern age is figuring out how to make wise choices.
Might as Well Get Juiced
Most of the stories we are told serve some purpose: to sell a product, support a belief, sustain a social position. The first thing to ask of any contemporary story is the obvious one: Who benefits? In a mass-mediated world, many different self-interested groups are offering us stories we seem to want to hear. In the case of mood medication, the pharmaceutical industry is spending and making stunning amounts of money selling us a story of "chemical imbalances" that their product can safely correct. The recovery community and the mental health industry are both telling us a story of epidemic levels of disorders that require their particular kinds of treatment. And the medical establishment believes it is now better able to "do something" for the many patients who are stressed, anxious, and unhappy.
Those who take mood medication of-ten report that they are now much better able to cope with their stress, anxiety, and unhappiness. They are grateful, even if they are simultaneously uneasy about relying on pills or about various side effects. As Peter Kramer's 1993 bestseller Listening to Prozac describes so compellingly, many even celebrate the "new self" that cosmetic psychopharmacology seems to make possible. But even the most fervent celebrators of the possibilities of self-enhancement through medication express ambivalence about going too far with self-transformation. We may have the chemical ability to create and sustain ever more resilient and productive and desirable selves. Should we take that option?
If we are surrounded by contradictory stories, whose stories count? Clearly, we have every reason to be skeptical of the stories told to us through advertising. Is this also true of the stories told to us by politicians and journalists ? What about the stories told to us by the medical community, grassroots organizations, teachers, religious leaders, scientists, family members, or even those that emerge from our own gut? People with good intentions and no desire to make money from us can still have a vested interest in persuading us to their way of thinking. But how can we know if it is also in our interest?
It's Not Easy
Because it is all too easy to fall for plausible but damaging stories, we need to find ways to figure out which stories to believe. We aren't as good as we think we are at using evidence to make wise decisions. As Michael Shermer points out in Why People Believe Weird Things (1997), we fall into logical fallacies and superstitious beliefs with amazing ease. In his analysis of pseudoscientific thinking, Shermer identifies a number of characteristics that bolster faith in our current practices of medicating depression and anxiety.
For example, we are too easily persuaded by anecdotal evidence, by scientific language, and by bold statements, all of which have abounded in media coverage of mood medication. I've reviewed news coverage of mood medication since the early 1990s, and Shermer's caveats describe perfectly their heady mix of personal success stories, accounts of scientific breakthroughs, and hyperbolic language of personal, social, and cultural transformation.
We also succumb to emotive words ("depression is a disease ...") and false analogies ("... to be treated like diabetes"). And we tend to over-rely on authorities ("neuroscientists believe ... "). We like to split the world in two (well or sick, normal or abnormal, functional or dysfunctional). We eagerly deploy circular reasoning ("I feel better now that I'm taking this medicine, which I'm told is treating a chemical imbalance; therefore my brain is imbalanced and I must need the medication"). Why do we fall for hokum? Shermer believes we ate vulnerable to false beliefs because we want certainty, especially in an increasingly complex society.
But sorting out what is best to believe requires some heavy intellectual lifting. It requires discursive analysis, empirical analysis, and ideological evaluation. Armed with these, I can get to what counts most: the consequences of belief.
Having concluded that there are three competing discourses at issue (addiction, neuroscience, mental health), I researched the history of mental illness, drugs and drug use, and addiction treatment and recovery, as well as accounts of how wrong and dangerous the dominant perspective in each of these areas has been. The more I read, the more confusing and contradictory things became.
Were evil drug companies profiting from our need to be efficient emotional machines, brainwashing us into thinking we were mentally ill? Was the mental health industry an elaborate, expensive, debilitating sham? Was the pharmaceutical industry creating a nation of addicts for its own profit? Was the medical establishment just trying to keep patients drugged and tractable?
Or did the dramatic rise in mood medication mean that people have been, or are now, suffering depression in epidemic proportions? If so, are they fortunate to have these ways to avoid succumbing to this devastating scourge? According to this story, these medications are a boon, not a conspiracy. They empower people to recover from debilitating conditions that until now have ruined lives.
The "cosmetic psychopharmacology" perspective goes even further. It suggests that we now have the technology and techniques to match our mood to our circumstances to become the people we need and want to be. This isn't drug addiction, of treating a debility, but a free choice to use whatever means we have at our disposal to make our lives ever better. Just as we would choose to use antibiotics, vaccines, liposuction, orthodontia, or eyeglasses, we could use mood medication to adjust ourselves to--or triumph over the demands of today. As Carl Elliott compellingly explains in the recent Better Than Well: American Medicine Meets the American Dream, there are multiple "enhancement technologies" people use for self-improvement. These medications are modern means to long-sought ends; why not make the most of them?
Between these two claims--conspiracy and boon--is the seemingly scientific middle ground, offered by news-magazines, pharmaceutical P.R., and the mental health community, among others. It goes like this: Americans are experiencing an epidemic of depression, now fortunately treatable by a new class of drugs that restores brain chemical balance. The Zoloft ads, with their childish bubbles of serotonin, are the best example of this version of how and why the latest form of mood medication works. According to this story, these drugs aren't perfect (better, more promising ones are on the way), but they are effective and fairly sale. We are not becoming addicts, and we are not using medicine to feel better than normal; we are simply taking medicine to rectify a brain chemical imbalance. As the pamphlets on depression remind us, it's just like taking insulin if you are a diabetic.
Each of these ways of thinking about mood medication draws in various ways on the three deeper discourses. The neuroscientific perspective focuses on how brain chemicals affect mood; the addiction perspective focuses on how drugs are used to cope with life; and the mental health perspective focuses on what are normal or abnormal feelings. So the next step is to sort out the empirical evidence for each of these stories: What do we really know about brain chemicals, addiction, and mental health?
If only empirical evidence were so easy to evaluate. Instead, each of these perspectives generates its own plausible antithesis; this is the dialectic of discourses. Not everyone believes the serotonin story: There are many reputable neuroscientists, such as Elliott Valenstein, author of the 1998 book Blaming the Brain, who reject the simple model of chemical deficit that the drug companies use to market their products. Nonetheless, the ads and their critics are both using the discourse of neuroscience: They use the same evidence to support or refute the role of serotonin in mood.
Likewise, the dominant 12-step perspective on addiction and recovery has both proponents and critics. Alcoholics Anonymous and related programs are allied, in complex ways, with a rehabilitation industry that treats alcohol and drug use as a disease that can be put into remission but never cured. Critics point out that these programs rely on techniques of brainwashing and conversion to convince people they are victims of a disease that only the 12-step process can treat. But both proponents and critics of these programs share the discourse of addiction and recovery. They draw on or refute experiential as well as experimental evidence about how to address problematic drug and alcohol use.
Already we are combining discourses: Are antidepressants problematic drugs or deficit-correcting medicines? In order to sort out the addiction discourse, we need to figure out the neuroscience discourse. And that doesn't necessarily help us with the third discourse on what constitutes mental health.
Emotional Rescue
What is normal mood, anyway? The antidepressant ads suggest that the products they tout help you "feel like yourself again." But who is this "self" and should he or she be the vibrant, active, zest-filled person the ads depict? What makes us so sure that mental health is about feeling good most of the time? There are those who argue convincingly for the value and worth of the darker emotions, who are highly critical of a modern American propensity to make everything sunny.
There are also social critics who argue that it benefits capitalism to keep workers cheerful and productive, and that it benefits patriarchy to keep women chipper and docile. From their perspectives, taking antidepressants prevents the kind of legitimate anger and motivated action that social inequalities require; it makes us all into Stepford employees and partners. But is this argument disrespectful of the genuine suffering these new medications supposedly alleviate? Sorting out what constitutes reasonable and unreasonable emotionality is a highly charged, and often highly personal, endeavor. Whose experiences and beliefs count here? Should we consult the social critics, mental health professionals, our family and friends, or our own preferences?
Your way through this thicket of contradictory, plausible, and interdependent discourses will no doubt be different from mine. All I want to do here is show how I've made my way, trying to evaluate evidence in ways that help me assess the consequences of believing in some stories instead of others. We can never know for sure if we are making the "right" decision. As Shermer notes, I will probably remember only the evidence and arguments that confirm my choice, and ignore or dismiss the evidence that contradicts it. But at least we each have the opportunity to try to sort things out for ourselves.
So: My own sense of the neurochemical evidence is that the medications so many are taking are far riskier and offer far less benefit that we now realize. So I believe in the "counter-discourse" of neuroscience--that the dominant serotonin story is misleading and potentially dangerous, and that the critique of the dominant story has it mostly right. The model of chemical imbalance sells drugs but doesn't have much to do with how brain chemistry actually functions in mental states. We still know very little about how (or even if) particular brain chemicals connect with particular moods, feelings, or perceptions, and neuroscientists are constantly revising their always-contingent models.
Evidence is accumulating that suggests much of the anecdotal evidence of successful mood alteration may be due to a placebo effect. Some recent controlled studies do not consistently show positive effects from these medications, and other studies suggest that side effects, including suicidal thoughts and actions, are more prevalent than previously publicized. The effects of the medicine on the brain may be structural, long-term, and not very beneficial. To me, that sounds like an unacceptable level of risk.
But maybe I really do have something wrong with my brain, and my heavy drinking in adolescence and early adulthood was my feeble attempt to deal with a condition these new medications could finally treat. Maybe my belief that I'm selling out my sobriety by taking legal drugs is ludicrous. There ate certainly compelling critiques of the recovery industry and 12-step programs (by, among others, reason contributors Thomas Szasz and Stanton Peele) that would suggest I have been propagandized and brainwashed. Critics of A.A. and related programs rightly note the ideological rigidity, lack of empirical evidence, cult-like qualities, hypocrisy, illogic, and cliche-ridden aspects of what has been called "the recovery movement." Have I fallen for an ideology that means I "keep coming back" for lies?
I am also plenty skeptical of the late-20th-century boom in insurance-funded rehabilitation institutions, and I am very much opposed to requiring those arrested for drunk driving to attend A.A. meetings of go into treatment if they want to avoid jail. I get uneasy around the cliches and psychobabble that flourish in some recovery settings. But I am also impressed by the democratic, self-supporting nature of A.A. and inspired by the sanity and wisdom of the people who sustain it. So in relation to this discourse, I (in the language of recovery) take what I need and leave the rest, and I am grateful to be able to hang around with people committed to recovery discourse. Nonetheless, I don't really believe alcoholism is a disease. Taking one drink or pill might not lead me back into active alcoholism, but it's just not worth the risk to me. So I'm choosing to live by the alcoholism discourse, even as I doubt many elements in it and agree with many elements of the critique of it.
You Can't Always Get What You Want
One of the reasons I can do this is that I find much of the dominant mental health discourse so unconvincing. I used to think that we'd made great strides in treating serious mental illnesses such as schizophrenia, and that we are now making progress with anxiety and depression. Not any more; the history of the treatment of mental illness is an appalling one, up to and including the present day. If you doubt this, read Robert Whitaker's 2002 book Mad in America: Bad Science, Bad Medicine, and the Enduring Mistreatment of the Mentally Ill, and learn how the mentally ill have suffered horrible indignities and permanent brain damage thanks to mainstream mental health practices. He points out, for example, that the shuffling gait, jerking arm movements, and vacant facial expression we now think of as symptoms of schizophrenia are due, in large part, to dopamine deficiencies caused by current medication, not the condition itself.
I've also read the academic literature on how the treatment of mental illness is actually a form of social control for deviant or disruptive behavior. I find these accounts convincing, especially in relation to women. The history of the treatment of women's depression shows how historically familiar the current reliance on medication is. Women have long been silenced and dismissed through labeling. When people seek to explain the alleged "epidemic" of depression, they don't look to the possibility of social causes and therefore the need for social changes, but instead focus on controlling and medicating the people who display disruptive symptoms.
Critics of modernity, from the Frankfurt School to the post-structuralists, point out that we can be convinced to become willing participants in our own oppression. They argue that capitalism, patriarchy, and modernity convince us to become what these systems need us to be. Even though I'm less worried about these systems than they are, I think there is at least some value in constant skepticism about the importance of being "normal" if "normal" means being docile and tractable.
In fact, I've long been drawn to the grouchy and the eccentric. There is something enlivening about being a crank, and something scary about how easily difference is labeled pathology these days. The relentless emphasis on "adjustment" that sociologists criticized in the 1950s is now so commonplace as to be almost invisible. But what's so great about being adjusted to systems I don't always believe in or support?
So here's where I end up: Mood medication is too risky for me to take or want to give to my kids, although I'm happy to let other people take whatever legal or illegal drugs they want as long as they realize what they are doing. I don't want my friends, family, of fellow citizens to get sucked into believing they are treating a chemical imbalance with medicine when what they are actually doing is taking drugs to feel better.
I think we make too much of being "normal" Variety and difference are good things. I want people to stop falling for stories about diseases and imbalances that make them eager consumers of expensive, possibly dangerous, and possibly ineffective drugs. Taking drugs to feel better may be just fine for you, but I am betting that the option is particularly dangerous for me. So far, living without most drugs (I'm keeping the caffeine) has worked out pretty well.
You Can Make It If You Try
If Shermer is right, I am most vulnerable to being duped when I believe that I've got it all figured out. The ideologically rigid are the easiest to fool. So in order to make wise decisions, I must do my best to stay open to alternative discourses, to what in scientific inquiry is called disconfirmation, while recognizing that my best bet is to put all easy answers to the test.
Because, at least for me, the easiest answers are the riskiest ones. For now I'll stick with my challenging but familiar anxiety, buoyed by knowing that in previous times and other cultures, worry and melancholy were valued differently. I'll accept that my perspective is not currently the dominant one, and that I may have to turn to historical of marginal of even discredited discourses for support. I'll ally myself with the difficult and eccentric over the easy and productive. I'll remain wary of the long-term effects of drugs that are invented and marketed to treat conditions that I think are just convenient and self-interested renamings of the human condition.
I'll also keep using some of the language of addiction, even though I don't believe alcoholism is really a disease. I'll use it because I gain direct benefit from following the metaphor, and because it gives me a way to make sense of how much different and better my life is now that I neither drink nor use drugs. I also choose to continue with the discourse of addiction, in spite of the compelling arguments about its limits and fallibility, because it allies me with people who are living in ways I value.
In this way, then, I am making the most of what modern life does so well: democratizing knowledge. More and more of us have access to multiple, contradictory ways of defining the world. We have more freedom to choose our beliefs than anyone has ever had before, but this increasing freedom comes without guarantees. We must realize that truth does not automatically emerge in a free marketplace of ideas. In today's mediated and self-interested marketplace of discourses, we each need to sort out our truths with diligence, skepticism, and persistence.
Joli Jensen (joli-jensen@utulsa.edu), a professor of communication at the University of Tulsa, is the author, most recently, of Is Art Good for Us? Beliefs About High Culture in American Life (Rowman & Littlefield).
JOLI JENSEN'S interest in mood-altering pharmaceuticals, the focus of "Emotional Choices" (page 28), is not merely academic. As someone who has wrestled with depression, Jensen says she has been "amazed by the number of different health care professionals who have offered to write me prescriptions, and by how baffled they are by my refusal to give these drugs a try." Jensen says she was reticent about offering such a personal take on the issue, but it is "only fair to illustrate--using my personal experience--the kinds of quandaries all of us face." Jensen teaches communications at the University of Tulsa.
COPYRIGHT 2004 Reason Foundation
COPYRIGHT 2004 Gale Group