Physicians seeing young girls and women with epilepsy now have strong reason to ensure the prescription of newer anti-epileptic drugs whenever possible.
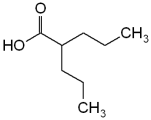
New data suggest that older anti-epileptic drugs (AEDs) particularly valproic acid, when taken during pregnancy, are associated with a high risk of birth defects, said Dr. Diego Wyszynski, who presented his findings at the meeting of the European Federation of Neurological Societies.
"This is the first time that we have data from large pregnancy registries on old anti-epileptic drugs as well as some of the new drugs. So this is a new message alerting clinicians to think, even when they see a young patient, about the risks of the drug during pregnancy." Dr. Wyszynski, assistant professor of medicine and of epidemiology at Boston University, said in an interview.
Published studies suggest that approximately half of all patients with epilepsy tend to stick with the first drug they are prescribed, so starting girls on or switching them to drugs with low teratogenic risk makes sense, he said.
His recommendations are based on new data from three large AED pregnancy registries, which show that the rate of birth defects associated with valproic acid use during pregnancy is between two and three-and-a-half times higher than the rate associated with newer AEDs. Malformations associated with valproic acid include heart defects, spina bifida, multicystic dysplastic kidney, postaxial polydactyly type B, inguinal hernia, and penile hypospadias.
The North American Antiepileptic Drug Pregnancy Registry, for which Dr. Wyszynski is the senior epidemiologist, included 3,400 women from the United States and Canada. The United Kingdom Epilepsy and Pregnancy Register included 2,637 women from Great Britain, and the Australian Independent Prospective Pregnancy Registry included 630 women.
All three registries showed that the risks of serious birth defects associated with carbamazepine and lamotrigine (Lamictal)--both newer AEDs--are between 2% and 3%, which is in line with the baseline risk in women not taking AEDs.
The registries also showed a significantly increased risk associated with valproic acid: 6% in the U.K. registry, almost 11% in the North American registry, and more than 6% in the Australian registry.
In addition, Dr. Wyszynski's group has published data from the North American registry showing that 5 of 77 pregnancies (6.5%) with exposure to phenobarbital were associated with major malformations, which suggests a risk 2-3 times higher for the offspring of exposed women than that in the general population (Arch. Neurol. 61[5]:673-678, 2004).
"The major surprise was not the results per se but that coming from different pregnancy registries, all with different collection protocols and definitions of malformations, the results are remarkably similar." said Dr. Wyszynski. "Now we know that valproic acid substantially increases the risk of birth defects, whereas lamotrigine and carbamazepine do not."
But valproic acid remains a popular AED, because it is well tested and very efficacious, he said. Some patients might not get optimal seizure control on a newer drug.
Additionally, the choice of poorer seizure control in favor of less teratogenicity may not necessarily be safer for the fetus in all cases.
"Having seizures during pregnancy could be so serious that it could endanger the life of both the mother and the fetus, so all these things need to be taken into account," he said.
Although the risks of birth defects associated with lamotrigine and carbamazepine appear no greater than the baseline risk, they should not be viewed as risk-free. Children of women who take lamotrigine and carbamazepine in pregnancy "have the same rate of malformations that you find in the general population, which is not zero," he said.
Additionally, these drugs have other risks associated with them. Carbamazepine, like valproic acid, has been linked to an increased rate of neurodevelopmental and low IQ problems, and long-term lamotrigine use has been tied to the development of polycystic ovary syndrome and osteoporosis.
Both the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics recommend an increased dose of folic acid (4 g/day) preconceptually for women taking AEDs. But 50% of pregnancies in the United States are unplanned, underscoring the need to tackle the issue as early as possible, he said
Switching to a safer AED in pregnancy could potentially do more harm than good. "Because most of the malformations occur between the first and second month of gestation, by the time most women realize they are pregnant it will be too late to prevent them. So not only will switching the drug at this point be ineffective in reducing the risk of malformations, but it may also increase her risk of seizures," he said.
BY KATE JOHNSON
Montreal Bureau
COPYRIGHT 2004 International Medical News Group
COPYRIGHT 2004 Gale Group