The prevalence of both community- and hospital-acquired methicillin-resistant Staphylococcus aureus (MRSA) has gone through the roof of our incubators. Some have speculated that the increase may be due to the inappropriate use of third-generation cephalosporins, (1) while others have suggested widespread use of quinolones is responsible. (2)
Laboratorians may not appreciate the extremely limited antibiotic options available to treat MRSA infections. Because many MRSA isolates test clindamycin-resistant, susceptibility reports using the standard Gram-positive panels list vancomycin and linezolid as the only antibiotics to which the offender is sensitive.
[FIGURE 1 OMITTED]
Because vancomycin-resistant staphylococci are very rare, vancomycin has long been considered the gold standard for treating MRSA infections. Unfortunately, despite its in vitro activity, when vancomycin is used as single-drug therapy to treat MRSA infections, cure rates in serious infections have been very disappointing. Sakoulas (3) has reported 44% failures in treating bacteremia, and Moise and Schentag (4) have shown 40% failures in treating lower respiratory-tract infections.
In treating nonserious MRSA infections, such as wounds, skin, and urinary-tract infections (UTIs), in addition to slow cure rates and failures, vancomycin is practically and economically burdensome. Because there is no oral form, a patient for whom vancomycin is prescribed must wear an infusaport around the clock. Additionally, he must visit daily an infusion center or have home infusion service. To avoid toxicity, blood levels must be monitored. Vancomycin drug acquisition, administration, and laboratory costs are approximately $100 per day.
Most MRSA isolates test sensitive to linezolid, an oral drug that is usually well tolerated, but which carries a risk of hematological abnormalities, including myelosuppression and thrombocytopenia. Linezolid costs $120 per day (i.e., $1,200 for a 10-day course). For the many patients in our community who do not have health insurance, both vancomycin and linezolid are extremely unaffordable, making these nonviable treatment options.
The increase in childhood MRSA infections, especially ear and wound infections, was distressing to our pediatricians. When they prescribed vancomycin, they were unhappy about having to defend themselves to parents complaining about the practical problems of caring for a child who had to continuously wear an infusaport and have multiple blood draws. In response to their pleas for vancomycin and linezolid alternatives, queries to colleagues and subsequent multiple literature searches on the Internet resulted in some "hot tips."
Rifampin combination therapy to the rescue
Rifampin, which kills bacteria by inhibiting DNA-dependent RNA polymerase, was first introduced for use in the United States in 1971 and was approved for use to treat pulmonary tuberculosis and meningococcal carriage. It continues to be used today as part of long-term oral-combination therapy for mycobacterial infection. More recently, although it is ineffective single-drug therapy for treating staphylococcal infections, numerous studies have shown that when rifampin is combined with vancomycin, trimethoprim-sulfamethoxazole (trimeth/sulfa), minocycline, or ciprofloxacin, the resulting in vivo synergy markedly improves clinical outcomes.
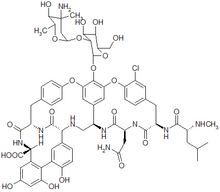
When an isolate tests sensitive for rifampin in combination with vancomycin, trimeth/sulfa, minocycline, or ciprofloxacin, depending on the site of the infection, the appropriate combination therapy is suggested to the physician as an additional option to consider. A flowchart (Figure 1) shows which rifampin combination therapy may be appropriate. These are not given as a substitute for the report on the routine Gram-positive antibiotics specified by NCCLS (now known as the Clinical Laboratory Standards Institute) but, rather, as additional options for the clinician to consider.
Pharmacology
Because rifampin is eliminated by the liver, reduced doses may be needed if the patient has elevated liver enzymes. Rifampin is available in both oral and intravenous (IV) forms. The IV form is very irritating to veins and must be diluted in large volumes of fluid and infused over several hours. Because the IV form offers no advantages in antibiotic levels over the oral form, the IV form is usually avoided except for use in patients who are not able to tolerate oral medications.
No severe interactions with other medications are indicated; however, rifampin speeds up the metabolism of other medications eliminated by the liver, such as anticoagulants, antiseizure drugs, narcotics, and birth control pills, which might require pharmacist consultation to adjust dosages of these other medications to maintain the same effect.
Minocycline, a tetracycline with unusual clinical efficacy against S aureus, is contraindicated in pregnant and pediatric patients. It must be taken with a full glass of water, and the pills must be swallowed whole to avoid esophagitis. Additionally, to prevent it from binding with calcium, minocycline must be taken between meals. It can also be bound and inactivated by magnesium and aluminum present in some antacids.
Although our clinicians were familiar with the antibiotics whose sensitivity we routinely report, very few of them were familiar with rifampin, as most have not managed tuberculosis. Because many also had not used minocycline, we believed it important to update them on the pharmacology of both antibiotics. We knew communicating pharmacology information would clutter routine reports, so we opted to write pharmacology addenda specific to each rifampin combination therapy option presented and attach these to the reports (see Tables 1, 2, and 3). The culture and sensitivity report directs the physician to read the addendum.
Treating MRSA and MRSE infections
Although vancomycin single-drug therapy may fail, even in treating MRSA and significant methicillin-resistant Staphylococcus epidermis (MRSE) infections due to isolates that test vancomycin-sensitive, addition of oral rifampin to vancomycin may improve the cure rate. (5,6) We present this to the clinician as an option to consider if the patient has a serious staphylococcal infection, such as a bacteremia, pneumonia, or internal body site infection.
Because its dialysis properties are well understood, vancomycin is often given at the time of dialysis to treat all types of infections in dialysis patients with suspected Gram-positive infections. With pharmacist consultation for dosing and interactions with other medications, oral rifampin may be a useful adjunct to vancomycin. In contrast, the dialysis properties of trimeth/sulfa and minocycline are less predictable; their use may be dangerous in dialysis patients.
For the treatment of nonserious skin and wound infections, trimeth/sulfa and rifampin combination therapy may be an alternative to vancomycin in patients of all ages. (7,8) For adults who have sulfa allergies or who have isolates that test trimeth/sulfa-resistant, minocycline plus rifampin may be an efficacious vancomycin alternative. (9,10)
Ciprofloxacin plus rifampin may be a third, but less-desirable, vancomycin alternative because ciprofloxacin use may result in increased MRSA rates and because the isolates often test ciprofloxacin-resistant, per the flowchart (Figure 1). (11)
Trimeth/sulfa monotherapy may be effective in treating MRSA and significant MRSE UTIs in patients of all ages whose isolates test sensitive. Although no references could be found specifically addressing minocycline plus rifampin for the treatment of UTIs, this combination has been shown in the above studies to be effective in treating more severe infections, which suggests it should be considered in treating staphylococcal UTIs in sulfa-allergic patients or in patients with trimeth/sulfa-resistant isolates.
Protecting the laboratory's legal liability status
Because the use of rifampin combination therapy may be a new approach supported by studies published some time ago, concern may exist that if these sensitivity-testing options are given to the physician, the laboratory possibly may be sued if the patient does not respond and/or there are other unintended adverse outcomes. In addition to providing the pharmacology addenda to clinicians, we believe that we have additional solid grounds, making such a situation a remote possibility.
For any isolate reported as sensitive to a given antibiotic, because of patient variables and other factors, it is never the case that in vitro sensitivity guarantees clinical success. Similarly, when we report the rifampin combination therapy results, we state these antibiotic combinations may be an option to consider. We never use language that would direct the physician to use rifampin combination therapy or in any way imply guaranteed clinical efficacy.
We have also continued to report the routine Gram-positive antibiotics specified by the NCCLS guidelines. We continue to provide our physicians sensitivity-testing information that gives them the choice to treat patients with infections caused by sensitive staphylococci with clindamycin (inducible resistance negative), vancomycin, and linezolid. We have not limited the clinicians' choices but, rather, we have expanded them.
To assist the laboratory, NCCLS has established breakpoints for rifampin and tetracycline, which predict minocycline susceptibility. The NCCLS guidelines also include a footnote stating that rifampin should not be used as single-drug therapy, but the guidelines do not specify the antibiotics with which rifampin should be combined. By using antibiotics that have been shown in published studies to have efficacy when combined with rifampin, we have "connected the dots," taking the guidelines to the next level.
Lastly, in every study published to date, whenever rifampin has been combined with any of the discussed antibiotics, clinical outcomes have been improved. To date, there have been no studies published in which rifampin clinical antagonism has been observed.
References
1. Fukatsu K, Saito H, Matsuda T, Ikeda S, Furukawa S, Muto T. Influences of type and duration of antimicrobial prophylaxis on an outbreak of methicillin-resistant Staphylococcus aureus and on the incidence of wound infection. Arch Surg. December 1997;132:1320-1325.
2. Weber SG, Gold HS, Hooper DC, Karchmer AW, Carmeli Y. Fluoroquinolones and the risk for methicillin-resistant Staphylococcus aureus in hospitalized patients. Emerg Infect Dis. November 2003;9:1415-1422.
3. Sakoulas G, Moise-Broder PA, Schentag J, Forrest A, Moellering RC Jr, Eliopoulos GM. Relationship of MIC and bactericidal activity to efficacy of vancomycin for treatment of methicillin-resistant Staphylococcus aureus bacteremia. J Clin Microbiol. June 2004;42:2398-2402.
4. Moise PA, Schentag JJ. Vancomycin treatment failures in Staphylococcus aureus lower respiratory tract infections. Int J Antimicrob Agents. November 2000;16 Suppl 1:S31-S34.
5. Gang RK, Sanyal SC, Mokaddas E, Lari AR. Rifampicin as an adjunct to vancomycin therapy in MRSA septicaemia in burns. Burns. 1999;25:640-644.
6. Burnie J, Matthews R, Jiman-Fatami A, Gottardello P, Hodgetts S, D'arcy S. Analysis of 42 cases of septicemia caused by an epidemic strain of methicillin-resistant Staphylococcus aureus: evidence of resistance to vancomycin. Clin Infect Dis. 2000;31:684-689.
7. Iyer S, Jones DH. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: a retrospective analysis of clinical presentation and treatment of a local outbreak. J Am Acad Dermatol. June 2004;50(6):854-858.
8. Walsh TJ, Standiford HC, Reboli AC, et al. Randomized double-blinded trial of rifampin with either novobiocin or trimethoprim-sulfamethoxazole against methicillin-resistant Staphylococcus aureus colonization: prevention of antimicrobial resistance and effect of host factors on outcome. Antimicrob Agents Chemother. June 1993;37(6):1334-1342.
9. Clumeck N, Marcelis L, Amiri-Lamraski MH, Gordts B. Treatment of severe staphylococcal infections with a rifampicin-minocycline association. J Antimicrob Chemother. June 1984; Suppl C:17-22.
10. Darouiche R, Wright C, Hamill R, Koza M, Lewis D, Markowski J. Eradication of colonization by methicillin-resistant Staphylococcus aureus by using oral minocycline-rifampin and topical mupirocin. Antimicrob Agents Chemother. August 1991;35(8):1612-1615.
11. Smith SM, Eng RHK, Tecson-Tumang F. Ciprofloxacin therapy for methicillin-resistant Staphylococcus aureus infections or colonizations. Antimicrob Agents Chemother. February 1989;33(2):181-184.
By Dennis L. Wegner, PhD
Dennis L. Wegner, PhD, is the consulting clinical microbiologist for a pathology group that provides laboratory services to eight community hospitals in southeast Iowa. On invitation, he presents his "Clinically Relevant, Cost-Effective Community-Hospital Microbiology" traveling workshop throughout the United States. He can be reached at dwegner@orhc.com.
Disclaimer: This article is intended solely as a literature review. The author and his employers do not wish to imply that recommendations are being made for treatment of staphylococcal infection in any patient and assume no legal liability for any treatment outcomes. Rather, it is hoped that the material contained in the article will prompt discussions between laboratorians, physicians, and pharmacists that will result in improved patient care. It is also hoped that the resultant decreased use of vancomycin will lessen the chances of selecting for vancomycin-resistant staphylococci and enterococci.
COPYRIGHT 2005 Nelson Publishing
COPYRIGHT 2005 Gale Group