Case Report
Two cases of interstitial pneumonia with cardiac failure developing in patients treated with the new antidepressant venlafaxine are presented. A strong relationship between the development of the patients' illness and the initiation of venlafaxine treatment was identified. The cytochrome P (CYP) 450 system is involved in the metabolism of venlafaxine, suggesting that alterations in the drug metabolic clearance might be, at least in part, responsible for the development of drug-induced damage in these cases. This might occur either as a consequence of a genetic factor or concomitant drug therapy with an inhibitor of the related CYP system. After identifying the causative agent in the first case, withdrawal of the antidepressant together with corticosteroid treatment led to a favorable outcome. In the other case, the multiorgan failure became fatal. These cases highlight a hitherto undescribed association of an adverse lung reaction and heart failure due to venlafaxine.
Keywords: antidepressant drug, venlafaxine; cytochrome P450; druginduced pneumonitis; heart failure
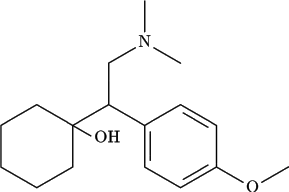
The number of drugs that have been shown to damage the respiratory system continues to increase (1, 2). The clinical pattern is diverse. Venlafaxine is an antidepressant with a unique chemical structure. It inhibits significantly reuptake of both serotonin and norepinephrine and lacks notable muscarinic-cholinergic or el-adrenergic effects. The serum halflife of the active metabolite of venlafaxine is 11 hours (3). Reported adverse effects include nausea, somnolence, insomnia, dizziness, constipation, sweating, anorexia, asthenia, nervousness, dose-dependent blood pressure elevation (4), and a potential risk for cardiac conduction changes or orthostatic hypotension (3). To date, only a few case reports have described adverse pulmonary effects, e.g., lung damage (5), acute eosinophilic pneumonia causing respiratory insufficiency (6), and pulmonary granulomatosis (7). This report describes two cases with drug-induced pneumonitis and heart failure associated with venlafaxine treatment.
CASE 1
A 21-year-old woman was admitted to her local hospital 2 months before referral to the Sarcoidosis Management Center (Maastricht, The Netherlands), with progressive dyspnea, a nonproductive cough, vomiting, weight loss (15 kg), and syncope of 4 weeks' duration. She had never smoked and had no prior history of respiratory illness or relevant comorbidity. No environmental or occupational pulmonary risk factors were apparent. A chest radiograph (CXR) showed subtle diffuse reticulonodular opacities throughout both lungs (Figure 1). The High-resolution computed tomography (HRCT) showed numerous diffuse bilateral small ill-defined pulmonary nodules (Figure 2). Lung function tests disclosed a restrictive ventilatory defect, severe depression of gas transfer, and a resting hypoxia on room air (Table 1). An ECG showed left bundle branch block. Echocardiography revealed a left ventricular (LV) ejection fraction of 38% with reduced function. Coronary angiography was normal. Cardiomyopathy and myocarditis were considered. She was treated with corticosteroids commenced at 50 mg daily, to which she responded well (Table 1). The corticosteroid dose was tapered every 2 days by 10 mg and finally stopped 10 days after initiation. Thereafter, her clinical condition deteriorated. As no explanation for the cardiopulmonary disease could be established and sarcoidosis was considered, she was referred to the Sarcoidosis Management Center.
Physical examination revealed no abnormalities and no fever. Bronchoalveolar lavage fluid analysis (performed the day after admission to the Sarcoidosis Management Center) disclosed an increased total cell count (130 x 10^sup 4^/ml), predominantly lymphocytes (93.2%). Culture of bronchoalveolar lavage fluid was sterile. Laboratory findings including an autoantibody screen revealed no abnormalities; serum angiotensin-converting enzyme was low (1 U/L). Histological examination of lung tissue obtained by video-assisted thoracoscopic surgery demonstrated a mainly lymphocytic interstitial infiltrate (Figure 3A), with occasional giant cells and poorly formed nonnecrotizing giant cell granuloma (Figure 313). On further questioning, her recent drug history included no medication except venlafaxine (initially 75 mg daily; after 1 month 35 mg daily) for depression prescribed by her general physician, commenced 2 months before symptom presentation and continued during admission (the patient's own initiative without mentioning as she thought it was harmless). With the suspicion of a drug-induced hypersensitivity pneumonia, venlafaxine was stopped and glucocorticoid treatment restarted (40 mg daily, gradually tapered to cessation over 2 weeks). Her clinical condition improved within 2 weeks of drug cessation and corticosteroid medication. Dyspnea and cough disappeared, both CXR and HRCT abnormalities cleared, and lung function improved (Table 1). Moreover, her cardiovascular condition improved, with restoration of normal ECG findings, and the LV ejection fraction improved to 60%. Two weeks after admission all medication was stopped. At 3 years' follow-up the patient remained well without respiratory or cardiac disease.
CASE 2
A 62-year-old sales manager presented with a 6-week history of exertional dyspnea, a dry cough, and fever. He had a diagnosis of ischemic heart disease following an anterior myocardial infarction 30 years previously and chronic atrial fibrillation for which he was anticoagulated and prescribed digoxin. Between 1995 and 1999 he received amiodarone (200 mg daily). In March 1999, he was referred to the respiratory clinic because of a cough and an abnormal CXR revealing infiltrates in the right lower zone. Transbronchial biopsy demonstrated adenocarcinoma compatible with bronchoalveolar cell carcinoma. He underwent right lower lobectomy in October 1999; amiodarone was stopped and he remained well thereafter. Radiology and lung function improved. In July 2000, venlafaxine was started for depression. In August 2000 he developed progressive breathlessness and was transferred to the Royal Brompton Hospital (London, UK) in October.
Physical examination identified a fever (38.4 deg C), an irregulary irregular, relative bradycardia, and a blood pressure of 120/70. He was tachypneic (24/minute) with fine inspiratory crackles at the left base. A CXR revealed new left-sided ground glass shadowing. The HRCT, compared with a scan performed in June 2000, demonstrated the appearance of new ground glass shadowing in both lungs, especially the left lower lobe. Lung function tests showed a deterioration since May 2000 (Table 1). Echocardiography demonstrated significant reduction in LV function (May 2000: LV end-diastolic diameter, 5.2 cm; endsystolic diameter, 4.9 cm; November 2000: end-diastolic diameter, 6.4 cm; end-systolic diameter, 5.0 cm).
The patient was treated with broad-spectrum antibiotics, verapamil and digoxin, and oxygen, and anticoagulation was adjusted. The differential diagnosis included recurrence of bronchoalveolar cell carcinoma, or a drug-induced infiltrative lung disease (DI-ILD). The timing of the presentation soon after starting the antidepressant drug venlafaxine, together with its pattern on HRCT, favored venlafaxine as the cause. Venlafaxine was stopped. Empirical steroid treatment was deemed too hazardous in the context of a persisting febrile illness, and raised inflammatory indices (C-reactive protein > 100 mg/L). During the next 24 hours, he developed hypotension and O2 desaturation. His condition deteriorated and despite inotropic support, he progressed to multiple organ failure and died.
Autopsy revealed large pulmonary emboli, focal ischemia and superficial ulceration of the colonic mucosa, and heart failure. The lungs showed evidence of local recurrence of carcinoma on the right. On the left, there were features of established interstitial fibrosis and florid organizing pneumonia without eosinophils, but no features of lymphocytic interstitial pneumonia or carcinoma.
DISCUSSION
The similar clinicopathologic picture and temporal association with drug initiation in the cases presented strongly suggest the development of venlafaxine-induced noneosinophilic interstitial pneumonia and cardiac failure. Such simultaneous association has not been reported previously. In the first patient, withdrawal of the drug together with steroid treatment led to complete recovery, further supporting the drug association. In the second case, the temporal relationship and the pattern on HRCT and autopsy (organizing pneumonia) were consistent with a DI-ILD. An association of venlafaxine use and the reported clinical picture was a strong possibility. Moreover, amiodarone likely played no role in the final illness, having been stopped 17 months previously. The list of drugs implicated in lung injury has grown rapidly during the last decades (1, 2). The exact mechanism of lung injury is uncertain for most drugs. As venlafaxine reduces serotonin reuptake-like anorexic agents-a possible association with pulmonary hypertension has been considered (8). It is unlikely to be a direct effect and is probably a result of biotransformation of the drug in the lung to reactive metabolites and/ or oxygen species that damage lung cells (8). The lung is the target for this toxicity because of accumulation of the drug in the lung and/or the presence of a specific biotransformation pathway in the lung.
In hypersensitivity pneumonitis, as in DI-ILD, the first stage consists of an inflammatory process that evolves, over years, inevitably toward pulmonary fibrosis (1, 2, 9). Presumably, in some cases the presence of a fibrotic process reflects presentation at a later stage occurring after a previously overlooked allergic inflammation. Interestingly, Hubbard and coworkers found an association between cryptogenic fibrosing alveolitis and tricyclic antidepressant exposure (10). Therefore, for clinicians an early diagnosis of such pneumonitis is important because early drug cessation will reduce significantly the risk of irreversible fibrosis (2, 10). Even though not uncommon, the diagnosis of druginduced disease may be complicated by the fact that the symptoms are often nonspecific, the patient's underlying disease may be responsible for cardiopulmonary abnormalities, and the use of multiple drugs reduces the chances of identifying the offending agent (1, 2, 11). In general, the recognition of DI-ILD has become an increasingly important area in pulmonary disorders. Clinical presentation of DI-ILD varies and to relate lung disease with a drug, there must be a temporal relationship, appropriate clinical presentation, and ideally, improvement with discontinuation of the drug. Drug-induced reactions can cause any known pattern of lung histology. There are no specific tests; rechallenge is unlikely to be helpful and is generally regarded to be dangerous.
Venlafaxine belongs to a new generation of antidepressants inhibiting the reuptake of serotonin/noradrenaline (12). The exact mechanism of lung injury is uncertain for most DI-ILDs (8,12). DI-ILD is an established, albeit infrequent complication of the serotonin reuptake inhibitors such as fluoxetine (7, 8, 13). Increased pulmonary capillary leakage, noncaseating giant cell granulomas, interstitial pneumonia, and nonnecrotizing vasculitis have been described (14, 15). Various cardiovascular side effects reported with venlafaxine include vascular headache, angina pectoris, hypotension, but also hypertension and syncope (16,17). Less commonly, sinus bradycardia, first-degree atrioventricular block, bundle branch block, and even sudden death have been reported, suggesting venlafaxine is a possible proarrhythmic agent. The cases described had documented evidence of deterioration in ventricular function coincident with the use of venlafaxine and, in Case 1, an improvement on withdrawal. Direct toxic effect or hypersensitivity is likely.
The risk for development of DI-ILD, cardiopulmonary effects, and clinical patterns vary depending on a variety of host and drug factors (2). The lung is a target for toxicity because of its biotransformation pathways and/or pulmonary drug accumulation. Moreover, metabolism of certain drugs and xenobiotics also occurs to some extent in all body tissues, but mostly in liver, lung, intestinal tract, kidney, and skin (18). Although the lung contains several enzymatic pathways capable of xenobiotic metabolism, it is generally agreed that the cytochrome P (CYP) superfamily of enzymes is the main system catalyzing the oxidative metabolism and metabolic activation of most toxins and drugs. However, knowledge of the functional activities and cellspecific localization of the pulmonary CYP forms is still incomplete (11). There is interindividual variation in the metabolic handling of drugs. Host factors including genetic polymorphisms of the CYP genes) may be important determinants of susceptibility to adverse drug effects (10, 11). Increased plasma concentrations of venlafaxine can be observed not only after overdose administration of the drug but also because of decreased clearance in some subjects (14). Venlafaxine is metabolized by an isoenzyme of the cytochrome P450 system (CYP2D6) (14). In particular, CYP2D6 may manifest phenotypically as slow or rapid metabolizers (18, 19). Administration of venlafaxine to poor metabolizers places them at risk of accumulation of the drug to toxic concentrations (14). Adverse drug reactions are possible if the drug is an inhibitor of CYP isoenzymes and disrupts enzyme function. Furthermore, genetic differences may affect the function of P450 enzymes, resulting in a related change in drug clearance and production of oxygen species (18, 19). Until phenotyping becomes widely available, careful therapeutic monitoring and follow-up should determine individualized dosage.
In the second patient, it is possible that aberrant cytochrome P450 metabolism predisposed him to interstitial pneumonitis when exposed to venlafaxine together with verapamil. Drugs with a narrow therapeutic window and long half-life may cause serious toxicity especially in the case of interaction with drugs with affinity for the same cytochrome P450 isoenzyme (14). Also, coadministration of venlafaxine with drugs that inhibit the activity of CYP2D6, such as some antiarrhythmic agents, could provoke accumulation of the drug and predispose patients to drug-induced damage (20, 21). Therefore, in using CYP inhibitors, careful drug monitoring is required together with renal function, debrisoquine phenotype, and concomitant drug administration (20).
In conclusion, these cases highlight that drug-induced cardiopulmonary disease should be considered as a potential side effect of venlafaxine and the possible role of cytochrome P450 inhibitors in the development of drug-induced reactions needs to be considered. Both clinical and genetic risk stratification-pharmacogenomics-may lead to more accurate prevention of drug-induced damage in the future. Generally, the diagnosis of drug-induced disease may be difficult because the clinical and biological symptoms are often nonspecific, and the patients' underlying disease may be responsible for cardiopulmonary disease. Moreover, patients often use multiple drugs, which reduces the chance of identifying the offending agent. However, our first case reports the development of pulmonary damage and cardiac failure in a healthy young woman without relevant comorbidity or medical history. In both cases, a strong relationship between the development of the patient's illness and the initiation of venlafaxine treatment appeared. This suggests a previously undescribed association between venlafaxine treatment and cardiopulmonary disease.
References
1. Foucher P, Biour M, Blayac JP, Godard P, Sgro C, Kuhn M, Vergnon JM, Vervloet D, Pfitzenmeyer P, Ollagnier M, Mayaud C, Camus P. Drugs that may injure the respiratory system. Eur Respir J 1997;10: 265-279.
2. Camus P, Foucher P, Bonniaud P, Ask K. Drug-induced infiltrative lung disease. Eur Respir J 2001;18:93s-100s.
3. Wernicke JF. The side effects and safety of fluxetine. J Clin Psychiatry 1985;46:59-67.
4. Partridge SJ, MacIver DH, Solanki T. A depressed myocardium. J Toxicol Clin Toxicol 2000;38:453-455.
5. Bass SP, Colebatch HJH. Fluoxetine-induced lung damage. Med J Aust 1992;156:364-365.
6. Fleisch MC, Blauer F, Gubler JGH, Kuhn M, Scherer TA. Eosinophilic
pneumonia and respiratory failure associated with venlafaxine treatment. Eur Respir J 2000;15:205-208.
7. Kerviler de E, Tredaniel J, Revlon G, Groussard O, Zalcman G, Ortoli J-M, Espie M, Hirsch A, Frija J. Fluoxetin-induced pulmonary granulomatosis. Eur Respir J 1996;9:615-617.
8. Reeve HL, Nelson DP, Archer SL, Weir EK. Effect of fluoxetine, phentermine, and venlafaxine on pulmonary arterial pressure and electrophysiology. Am J Physiol 1999;276:L213-L219.
9. Akoun GM, Milleron BJ, Mayaud CM, Tholoniat D. Provocation test coupled with bronchoalveolar lavage in diagnosis of propranolol-- induced hypersensitivity pneumonitis. Am Rev Respir Dis 1989;139: 247-249.
10. Hubbard R, Venn A, Smith C, Cooper M, Johnston , Britton J. Exposure to commonly prescribed drugs and the etiology of cryptogenic fibrosing alveolitis. Am J Respir Crit Care Med 1998;157:743-747.
11. Hukkanen J, Pelkonen O, Raunio H. Expression of xenobiotic-metabolizing enzymes in human pulmonary tissue: possible role in susceptibility for ILD. Eur Respir J 2001;18:122s-126s.
12. Feighner JP. The role of venlafaxine in rational antidepressant therapy. J Clin Psychiatry 1994;55:62-68.
13. Chrysanthopoulos C, Siablis D, Kounis NG. Amiodarone-induced recurrent allergic pneumonitis. Ann Allergy 1988;60:111-114.
14. Khalifa M, Daleau P, Turgeon J. Mechanism of sodium channel block by venlafaxine in guinea pig ventricular myocytes. J Pharmacol Exp Ther 1999;291:280-284.
15. Liu X, Emery CJ, Laude E, Herget J, Gill G, Cope G, Barer GR. Adverse pulmonary vascular effects of high dose tricyclic antidepressants: acute and chronic animal studies. Eur Respir J 2002;20:344-352.
16. These ME. Effects of venlafaxine on blood pressure: a meta-analysis of original data from 3744 depressed patients. J Clin Psychiatry 1998;59: 502-508.
17. Reznik I, Rosen Y, Rosen B. An acute ischaemic event associated with the use of venlafaxine: a case report and proposed pathophysiological mechanisms. J Psychopharmacol 1999;3:193-195.
18. Wormhoudt LW, Commandeur JNM, Vermeulen PE. Genetic polymerphisms of human N-acelyltransferase, cytochrome P450, glutathione-- S-transferase, and epoxide hydrolase enzymes: relevance to xenobiotic metabolism and toxicity. Crit Rev Toxicol 1999;29:59-124.
19. Michalets EL. Update: clinically significant cytochrome P450 drug interactions. Pharmacotherapy 1998;18:84-112.
20. Haefeli WE, Bargetzi MJ, Follath F, Meyer UA. Potent inhibition of cytochrome P450IID6 (dedrisoquin 4-hydroxylase) by flecainide in vitro and vivo. J Cardiovasc Pharmacol 1990;15:776-779.
21. Birgersdotter UM, Wong W, Turgeon J, Roden DM. Stereoselective genetically-determined interaction between chronic flecanide and quidine in patients with arrhythmias. BrJ Clin Pharmacol 1992;33:275-- 280.
Marjolein Drent, Suveer Singh, Anton P. M. Gorgels, David M. Hansell, Otto Bekers, Andrew G. Nicholson, Robert Ian van Suylen, and Roland M. du Bois
Departments of Respiratory Medicine, Cardiology, Clinical Chemistry, and Pathology, and Sarcoidosis Management Center, University Hospital Maastricht, Maastricht, The Netherlands; and Departments of Respiratory Medicine, Radiology, and Pathology, Royal Brompton Hospital, London, United Kingdom
(Received in original form July 24, 2002; accepted in final form October 16, 2002)
Correspondence and requests for reprints should be addressed to Marjolein Drent, M.D., Ph.D., Department of Respiratory Medicine, University Hospital of Maastricht, P.O. Box 5800, 6202 AZ Maastricht, The Netherlands. E-mail: mdr@slon. azm.nl
Copyright American Thoracic Society Apr 1, 2003
Provided by ProQuest Information and Learning Company. All rights Reserved