A 50-year-old man presented with primary lung cancer with bone lesions and calcifying liver nodi. Two months after stopping chemotherapy, he tied. Autopsy revealed multiple organ metastases. Histologically, the calcified nodi in the liver proved to be affected by tumor metastasis.
(CHEST 1997; 111:1121-22)
Key words: calcification, liver metastases, lung cancer
No report on calcifying metastases of the liver in the case of lung cancer has been found up until now. On the other hand, several cases of metastasizing primary colon adenocarcinoma with calcification developing in the metastatic nodi during local or systemic chemotherapy have been reported. The case described in the present report allows for the conclusion that, despite the presence of other signs of regression, calcification in liver metastases should not be regarded as an indication of good prognosis.
CASE REPORT
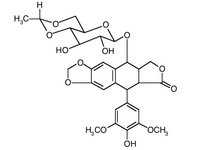
A 50-year-old man was admitted to the hospital with shortness of breath and right-sided subscapular pain that had started 2 months before admission. On the chest x-ray film, a 5 x 6-cm round shadow was seen in the left parahilar region which proved to be a primary adenocarcinoma originating in the 6th segment. A bone scan showed multiple pathologic accumulation of the isotope material, and on the liver scan inhomogeneity was detected. After informed consent, cytostatic treatment was started with epirubicin hydrochloride (Farmorubicin), cisplatine (Cisplatin), and etoposide (Vepesid). Following the third course of these drugs, the shadow on the chest x-ray film disappeared, leaving a linear shadow behind it; on the liver scan, echodense nodi 10 to 20 mm in diameter appeared; echodense nodi corresponded to calcifications in the liver (Fig 1). As the patient improved, the linear shadow disappeared, and the number of the pathologic radioisotope accumulations on the bone scan decreased. Therefore, the calcification was interpreted as a sign of regression of the malignant lesions in the liver. However, 4 months after discharge, having received 6 courses of chemotherapy, the patient was readmitted in a deteriorated state and died 1 month later with signs of multiple metastases. In the final period of the disease, the echodense and echopoor nodi enlarged, with the sign of calcification remaining unchanged. Autopsy revealed that the liver metastases contained a large amount of calcium (Fig 2.).
[Figures 1-2 ILLUSTRATION OMITTED]
DISCUSSION
Calcifying liver metastases can be seen in cases with primary colon adenocarcinoma, and such calcification can develop during local or systemic cytostatic therapy.[1] Although cases of calcifying nodal metastases in the midhilar region of primary adenocarcinoma of the lung have already been reported,[2] no account of calcifying liver metastases of primary lung cancer has been found. It is known that calcification of the primary lung cancer per se does not exclude a malignant process, and this calcification does not show any correlation with the histologic type.[3] In our case, calcification in the liver was first interpreted as a good prognostic sign; at the same time of its appearance, the number of pathologic lesions on the bone scan decreased and the chest x-ray film showed diminution of the shadow in the left parahilar region. However, 5 months later, the patient died with signs and symptoms of general metastases, with the autopsy showing calcifications in the tumorous nodi of the liver cells. In conclusion, the authors of the present study agree with Hruby et al[4] that any sign of calcification in liver metastases must be regarded as a manifestation of the malignant process, though its presence as an effect of the cytostatic treatment cannot be excluded.
REFERENCES
[1] Rubaltelli L, Zacchi C, Angelini F, et al. Liver metastases with posterior acoustic shadow in echography: causes and differential diagnosis. Radiol Med 1983; 69:316-19
[2] Austin JH, Grimes MM, Carberry D. CT detection of calcified nodal metastases of lung adenocarcinoma. J Comput Assist Tomogr 1988; 12:314-16
[3] Grewal RG, Austin JH. CT demonstration of calcification in carcinoma of the lung. J Comput Assist Tomogr 1994; 18:867-71
[4] Hruby VW, Traxler M, Wassipaul M, et al. Comparison of ultrasonic and CT diagnosis of solid liver tumors. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 1988; 148: 378-83
(*) From the Department of Respiratory Medicine and Pathology Institute, County Hospital, Pecs, Hungary Manuscript received June 3, 1996; revision accepted September 24, 1996. Reprint requests: Dr. Zoltan Baliko, Dept of Respiratory Medicine, County Hospital, Pecs, Angyan J u 2, 7635 Hungary
COPYRIGHT 1997 American College of Chest Physicians
COPYRIGHT 2004 Gale Group