Background: The restoration of coronary flow after transient ischemia immediately induces life-threatening ventricular tachyarrhythmias. Although most of these arrhythmias disappear spontaneously, some of them induce serious hemodynamic changes. This retrospective study investigates the efficacy of therapy with intracoronary verapamil to terminate reperfusion-induced ventricular tachyarrhythmias in patients with acute myocardial infarction (AMI).
Methods and results: Between February 1992 and February 2003, 390 patients with a diagnosis of AMI were enrolled into the study. All patients received mechanical revascularization therapy within 6 h of onset of symptoms, and 109 patients experienced reperfusion-induced tachyarrhythmias. A subset of these patients was treated with intracoronary verapamil (0.25 to 1.0 mg) to terminate the reperfusion-induced tachyarrhythmia. They were evaluated for immediate termination of the tachyarrhythmias, hemodynamic changes, resumption rates, and major complications. Thirty-one patients (28%) were treated with intracoronary verapamil for the immediate termination of reperfusion-induced ventricular tachyarrhythmias. These tachyarrhythmias included 6 premature ventricular contractions, 19 accelerated idioventricular rhythms, 3 ventricular tachycardias, 2 ventricular fibrillations (VFs), and 1 torsades de pointes. Intracoronary verapamil was effective in rapidly terminating all reperfusion-induced arrhythmias except for VFs. The side effects of treatment included temporary hypotension (two patients) and bradycardia (one patient), although all patients recovered spontaneously. No major complications were induced by the intracoronary use of verapamil, and no resumptions of arrhythmias were documented.
Conclusion: Intracoronary administration of verapamil can safely terminate reperfusion-induced ventricular tachyarrhythmias in a rapid manner. However, this effect was not seen for reperfusion-induced VF.
Key words: acute myocardial infarction; percutaneous coronary intervention; reperfusion arrhythmia; verapamil
Abbreviations: AIVR = accelerated idioventricular rhythm; AMI = acute myocardial infarction; LAD = left anterior descending coronary artery; PCI = percutaneous coronary interventional therapy; PVC = premature ventricular contraction; RCA = fight coronary artery; TdP = torsades de pointes TIMI = Thrombolysis in Myocardial Infarction; VF = ventricular fibrillation; VT = ventricular tachycardia
**********
Restoration of coronary flow after transient ischemia immediately induces ventricular tachyarrhythmias such as accelerated idioventricular rhythm (AIVR), ventricular tachycardia (VT), torsades de pointes (TdP), and ventricular fibrillation (VF). (1-3) Although reperfusion-induced arrhythmias demonstrate the successful reperfusion of an occluded coronary artery, they require special attention because hemodynamics may rapidly deteriorate. It is therefore clinically important to establish the mechanism of such reperfusion arrhythmias and treat them.
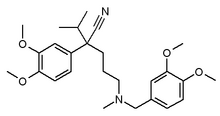
The causes of reperfusion arrhythmias are not filly understood. A delay after depolarization-induced activity (4) and all increase in [Ca.sub.2+] concentration are thought to play a role. (5) Blocking the L-type [Ca.sub.2+] channel has been shown to be effective in preventing reperfusion arrhythmias in rats. (6,7) Verapamil, an L-type [Ca.sub.2+] channel-blocking agent, has been shown to inhibit VT, TdP, and VF in animals and humans. (8-10) However, most investigators assessed the antiarrhythmic activity of verapamil by IV administration prior to coronary reperfusion. The aim of this study was to determine the ability of the intracoronary administration of verapamil to terminate reperfusion ventricular tachyarrhythmias during coronary intervention in patients with acute myocardial infarction (AMI).
METHODS AND MATERIALS
Study Population
The study population consisted of 390 consecutive patients admitted to Hiroshima City Asa Hospital from 1992 to 2003 with the following conditions: (1) diagnosis of AMI; and (2) percutaneous coronary intervention (PCI) therapy within 6 h of the onset of symptoms for Thrombolysis in Myocardial Infarction (TIMI) (11) grade 0/1 coronary flow. The study admission criteria included prolonged chest pain (ie, of > 30 min duration), typical ECG changes, successful reperfusion therapy within 6 h of the onset of chest pain as documented by coronary angiography, and more than a threefold increase in serum creatine phosphokinase levels. Among these patients, only those with an occurrence of reperfusion ventricular arrhythmias were selected. The study population consisted of 83 men and 26 women aged 32 to 88 years (mean [[+ or -] SD] age, 65 [+ or -] 11 years). The infarct-related artery was the right coronary artery (RCA) in 42 patients, the left main trunk artery in 1 patient, the left anterior descending coronary artery (LAD) in 58 patients, and the left circumflex coronary artery in 8 patients. Written, informed consent was obtained from all patients before they entered the study.
Coronary Angiography and Primary PCI
Coronary angiography and primary PCI were performed within 6 h of the onset of symptoms of AML Once the femoral or radial artery" was catheterized, 5,000 to 10,000 IU heparin was administered. Primary PCI was performed by use of a conventional catheter balloon technique. Reperfusion was considered to be successful when flow in the infarct-related artery was improved to TIMI grade 2 or 3.
Definitions
Rapid ventricular rhythms were classified by heart rate as AIVR (ie, > 60 beats/min but < 120 beats/min) or VT (ie, [greater than or equal to] 120 beats/min). AIVR and VT were further classified by their duration as sustained (ie, lasting > :30 s) or nonsustained (ie, lasting < 30 s).
Effect of Verapamil on Termination of Reperfusion Arrhythmias
The ability of verapamil (Vasolan; Eisai Co, Ltd; Tokyo, Japan) to terminate reperfusion arrhythmias was determined in patients with AIVR, VT, TdP, and/or VF that developed within 10 min of reperfusion. A single bolus infusion of 0.1 mg/mL verapamil diluted in a serum saline solution was delivered by a guiding catheter. For patients with AIVR of > 30 s duration, an intracoronary, bolus infusion of verapamil was performed, while continuous ECG and BP recordings were obtained. Patients whose arrhythmias were nonsustained or terminated spontaneously were excluded to assess precisely the effect of verapamil on AIVR. VT, TdP, and VF patients who had severe hemodynamic compromise were cardioverted immediately. The termination of sustained AIVR, sustained VT, or TdP during or within 30 s of the cessation of treatment was defined as a successful termination of arrhythmia. If the arrhythmia resumed within 20 min of cessation, the termination of reperfusion arrhythmia was considered to be unsuccessful.
Statistical Analysis
The data are expressed as the mean [+ or -] SD or the number (percentage) of patients. Differences between categoric variables were analyzed by [chi square] analysis, and differences between continuous variables were analyzed by the Student t test. A p value of < 0.05 was considered to be statistically significant.
RESULTS
Patient Population
Over an 11-year period, 390 patients were admitted to our hospital with a diagnosis of AMI and received mechanical revascularization therapy for TIMI grade 0/1 coronary flow within 6 h of symptom onset. Among these, 109 patients in the acute phase and with an occurrence of reperfusion arrhythmias were enrolled into the study. Thirty-one patients were treated by the intracoronary use of verapamil, 22 patients were treated by other antiarrhythmic drugs (lidocaine, 16 patients; disopyramide, 6 patients), and 9 patients were treated by electrical cardioversion. Patient characteristics are shown in Table 1.
Reperfusion Arrhythmias and the Effects of Verapamil on Termination of Reperfusion Arrhythmias
At the time of reperfusion, several tachyarrhythmias were induced. These included 26 cases of premature ventricular contraction (PVC), 61 cases of AIVR, 12 cases of VT, 1 case of TdP, and 9 cases of VF.
AIVR was nonsustained or subsided spontaneously in 38 patients (62%). VT and VF were terminated with cardioversion because of hypotension in 9 of the 21 patients (43%). All reperfusion-induced arrhythmias that were treated by IV administration of lidocaine (50 to 100 mg) or disopyramide (50 mg) were not successfully terminated.
Verapamil was administered to 6 patients with PVC, 19 with sustained AIVR, 3 with sustained VT, 1 with TdP, and 2 with VF. Although 0.5 mg verapamil was generally administered, 1 AIVR patient with a proximal LAD lesion supported by intraaortic balloon pumping and 1 VT patient with an RCA lesion were treated with 0.25 mg verapamil to avoid excessive hypotension or bradycardia. Because AIVR caused severe systemic hypotension in two patients with proximal LAD lesions, 1.0 mg verapamil was administered to ensure the termination of AIVR. Arrhythmias terminated during or immediately after the administration of verapamil in all 29 patients with PVC, AIVR, VT, and TdP (Table 2, Fig 1-3). However, two VFs were not terminated with verapamil therapy. AIVR or VT cycle length did not accelerate in any of the patients in response to verapamil. Arrhythmias did not resume until the completion of the PCI in all 29 patients.
[FIGURES 1-3 OMITTED]
Hemodynamic Changes and Complications
Therapy with the intracoronary administration of verapamil temporarily reduced systolic BP to approximately 65 mm Hg in two AIVR patients (Table 2). The occluded artery was the proximal RCA in one patient and the proximal LAD in the other. However, systolic BP returned to > 100 mm Hg within 1 min without any treatment. In a patient with a proximal RCA lesion, the intracoronary use of verapamil reduced his heart rate to approximately 35 beats/min (Table 2). However, heart rate spontaneously recovered to > 50 beats/min within 30 s. No major complications were induced by the intracoronary use of verapamil.
DISCUSSION
Our results confirm that the intracoronary use of verapamil can safely terminate reperfusion-induced ventricular tachyarrhythmias. Furthermore, we saw no evidence for the resumption of arrhythmias 'after treatment. It is important to rapidly terminate reperfusion ventricular arrhythmias, because hemodynamics have the potential to quickly deteriorate, especially during reperfusion-induced VT or VF. (12,13) AIVR also may induce hypotension in patients with depressed cardiac function. (14) To our knowledge, the present study is the first to demonstrate that the intracoronary use of verapamil can effectively and safely terminate ventricular tachyarrhythmias that develop at the time of reperfusion in humans. Our results support the findings of two previous case reports demonstrating that the IV use of verapamil terminated ventricular arrhythmias that were refractory to traditional therapeutic measures in one patient undergoing coronary artery-bypass surgery (9) and in another patient undergoing aortic valve replacement. (10)
Previous studies (8-10) have demonstrated that the IV use of verapamil prior to coronary reperfusion is effective in inhibiting VT, TdP, and VF, and they suggested that such treatment might improve the patient's prognosis. However, the IV use of verapamil may induce various systemic side effects, such as hypotension and bradycardia, and the systemic IV use of verapamil may be undesirable during the acute phase of acute coronary syndromes. Because conduction and antiarrhythmic effects occur at low plasma levels, one may avoid the undesirable hemodynamic depression associated with high plasma levels by titrating verapamil to the desired clinical effect. In studies of conscious subjects with good ventricular function, (15,16) no adverse hemodynamic effects were observed at steady-state systemic verapamil levels of < 200 ng/mL, although PR interval prolongation persisted for up to 4 h after the termination of the infusion. We injected only 0.25 to 1.0 mg verapamil into the coronary artery, and the systemic effects of its pressure and rate reduction were low enough to avoid any adverse hemodynamic changes. Although such a low dose of intracoronary verapamil prior to reperfusion could not prevent the occurrence of life-threatening reperfusion arrhythmias, our data suggest that it is able to rapidly terminate such arrhythmias when they do occur and to prevent them from recurring.
The precise mechanism by which verapamil terminates reperfusion tachyarrhythmias remains unknown. However, one possibility is that the attenuation of [Ca.sub.2+] influx via the L-type [Ca.sub.2+] channel prevents the development of delayed post-depolarization-induced triggered activity. One study (17) demonstrated that 4-aminopyridine abolished the TdP and VF noted during the reperfusion period, but it did not reduce the incidence of VT. Verapamil, on the other hand, abolished the TdP and VF, and reduced VT. These results suggest that delayed post-depolarization-induced triggered activity is likely to play an essential role in the development of VT, TdP, and VF, and that a transient outward current that is sensitive to 4-aminopyridine is necessary for the occurrence of TdP or VF. The underlying mechanism of VF or TdP may be different from that of VT in the ischemic reperfused heart. Another study (18) demonstrated that the administration of dipyridamole could prevent and terminate reperfusion arrhythmias such as AIVR and VT. They suggested that cyclic adenosine monophosphate-mediated triggered activity might, at least in part, be responsible for reperfusion-induced AIVR and VT. Further studies are needed to clarify the precise mechanism of such reperfusion arrhythmias.
We did not observe any recurrence of reperfusion-induced ventricular tachyarrhythmias in our study. This suggests that the stabilization of the electro-physiologic instability of cardiac myocytes following reperfusion might lead to the maintenance of the stable state.
Clinical Implications
The incidence of reperfusion-induced ventricular tachyarrhythmias was 28% in our study. This incidence is not high enough for us to use antiarrhythmic agents in all patients treated with coronary reperfusion therapy because of their unfavorable side effects. As discussed previously, the side effects of verapamil include systemic hypotension and bradycardia. However, these effects are dose-dependent and can be avoided by local use. The present study demonstrates that the intracoronary administration of verapamil is safe and effective. However, our study also demonstrates that the intracoronary administration of verapamil is not effective in terminating reperfusion-induced VF, and its use may be limited to patients with AIVR, VT, or TdP.
Study Limitations
The present study has several limitations. First, we treated only a small number of patients. However, the incidences of AIVR, VT, and VF were similar or even lower than those reported in previous studies. (2,19,20) Therefore, our treated population was clinically relevant to patients with reperfusion-induced ventricular tachyarrhythmias. Second, it is possible that some AIVR might resolve spontaneously. Therefore, the ability of verapamil to terminate AIVR might be unnecessary in some cases. However, since all cases of AIVR immediately disappeared during or shortly after the intracoronary administration of verapamil, we believe that most eases of AIVR were terminated by therapy with verapamil.
CONCLUSIONS
In conclusion, our study demonstrates that the intracoronary administration of verapamil can rapidly and safely terminate reperfusion-induced ventricular tachyarrhythmias. These effects were demonstrated for patients with reperfusion-induced AIVR, TdP, and VI', but intracoronary administration of verapamil could not effectively terminate reperfusion-induced VF in vivo.
* From the Department of Cardiology, Hiroshima City Asa Hospital, Hiroshima, Japan.
REFERENCES
(1) Balke CW, Kaplinsky E, Michelson EL, et al. Reperfusion tachyarrhythmias: correlation with antecedent coronary artery occlusion tachyarrhythmias and duration of myocardial ischemia. Am Heart J 1981; 101:449-456
(2) Goldberg S, Greenspon AJ, Urban PL, et al. Reperfusion arrhythmia: a marker of restoration of antegrade flow during intracoronary thrombolysis for acute myocardial infarction. Am Heart J 1983; 105:26-32
(3) Corr PB, Witkowski FX. Potential electrophysiologic mechanisms responsible for dysrhythmias associated with reperfusion of ischemic myocardium. Circulation 1983; 68:I16-I24
(4) Antzelevitch C, Sicouri S. Clinical relevance of cardiac arrhythmias generated by after depolarizations: role of M cells in the generation of U waves, triggered activity and torsade tie pointes. J Ain Coll Cardiol 1994; 23:259-277
(5) Thandroyen FT, McCarthy J, Burton KP, et al. Ryanodine and caffeine prevent ventricular arrhythmias during acute myocardial ischemia and reperfusion in rat heart. Circ Res 1988; 62:306-314
(6) Swies J, Omogbai EK, Smith GM. Occlusion and reperfusion-induced arrhythmias in rats: involvement of platelets and effects of calcium antagonists. J Cardiovasc Pharmacol 1990; 15:816-825
(7) Baxter GF, Yellon DM. Attenuation of reperfusion-induced ventricular fibrillation in the rat isolated hypertrophied heart by preischemic diltiazem treatment. Cardiovasc Drags Ther 1993; 7:225-231
(8) Yamamoto K, Bando S. Effects of verapamil and magnesium sulfate on electrophysiologic changes during acute myocardial ischemia and following reperfusion in dogs: comparative effects of administration by intravenous and coronary sinus retroperfusion routes. Angiology 1996; 47:557-568
(9) Kapur PA, Norel E, Dajee H, et al. Verapamil treatment of intractable ventricular arrhythmias after cardiopulmonary bypass. Anesth Analg 1984; 63:460-463
(10) Baraka A, Usta N. Verapamil treatment of intractable reperfusion ventricular tachycardia/fibrillation. Anesth Analg 1986; 65:102-103
(11) Chesebro JH, Knatterud G, Roberts R, et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase; clinical findings through hospital discharge. Circulation 1987; 76:142-154
(12) Toiler GH, Stone PH, Muller JE, et al. Prognosis after cardiac arrest due to ventricular tachycardia or ventricular fibrillation associated with acute myocardial infarction (the MILIS Study): Multicenter Investigation of the Limitation of Infarct Size. Am J Cardiol 1987; 60:755-761
(13) Volpi A, Maggioni A, Franzosi MG, et al. In-hospital prognosis of patients with acute myocardial infarction complicated by primary ventricular fibrillation. N Engl J Med 1987; 317:257-261
(14) Bigger JT Jr, Dresdale FJ, Heissenbuttel RH, et al. Ventricular arrhythmias in ischemic heart disease: mechanism, prevalence, significance, and management. Prog Cardiovasc Dis 1977; 19:255-300
(15) Reiter MJ, Shand DG, Aanonsen LM, et al. Pharmacokinetics of verapamil: experience with a sustained intravenous infusion regimen. Am J Cardiol 1982; 50:716-721
(16) Chew CY, Hecht HS, Collett JT, et al. Influence of severity of ventricular dysfunction on hemodynamic responses to intravenously administered verapamil in ischemic heart disease. Am J Cardiol 1981; 47:917-922
(17) Miyashita T, Kubota I, Yamaki M, et al. 4-aminopyridine inhibits the occurrence of ventricular fibrillation but not ventricular tachycardia in the reperfused, isolated rat heart. Jpn Circ J 2000; 64:602-605
(18) Yoshida Y, Hirai M, Yamada T, et al. Antiarrhythmic efficacy of dipyridamole in treatment of reperfusion arrhythmias: evidence for cAMP-mediated triggered activity as a mechanism responsible for reperfusion arrhythmias. Circulation 2000; 101:624-630
(19) Mathey DG, Kuck KH, Tilsner V, et al. Non surgical coronary artery recanalization in acute transmural myocardial infarction. Circulation 1981; 63:489-497
(20) Markis JE, Malagold M, Parker JA, et al. Myocardial salvage after intracoronary thrombolysis with streptokinase in acute myocardial infarction. N Engl J Med 1981; 305:777-782
Manuscript received December 8, 2003; revision accepted April 7, 2004.
Reproduction of this article is prohibited without written permission from the American College of" Chest Physicians (e-mail: permissions@ehestnet.org).
Correspondence to: Masaya Kato, MD, PhD, Department of Cardiology, Hiroshima City Asa Hospital, 2-1-1 Kabeminami, Asakita-ku, Hiroshima 731-0293, Japan; e-mail: ma-katou@asahosp.city.hiroshima.jp
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group