Since altered regulation of intracellular calcium concentration may be the final common pathway in the pathogenesis of asthma, [1] considerable interest has been generated in evaluating the efficacy of calcium channel blockers in this disease. [2] The results of several studies indicate that these agents generally do not alter resting airway caliber, but modestly alter experimentally induced asthma, depending upon the agent, dose, and method of provocation. [3-11]
Verapamil is a potent calcium channel blocker which inhibits calcium influx in smooth muscle preparations [12] and inhibits or relaxes acetylcholine-induced contraction of tracheal muscle strips, [13,14] although it is generally less potent than gallopamil (D-600) in these models. Studies of verapamil in asthmatic subjects [3,5-7,10] have shown no effect on resting airway function, and either no effect or a modest blocking effect on histamine-induced, methacholine-induced, or exercise-induced bronchoconstriction. A more significant blocking effect was demonstrated by Ahmed et al [7] in ragweed-sensitive subjects in whom inhaled, but not oral, verapamil markedly increased the dose of inhaled antigen required to produce an early increase in airway resistance. As these studies of verapamil in asthmatic subject have generally used only one dose level of the drug, it is unclear whether the variability in results and the small magnitude of effect were functions of inadequate dosage (pharmacokinetic failure) or an inherent lack of effect of the drug (pharmacodynamic failure). Therefore, the current study was designed to study inhaled verapamil over a wide range of doses to determine whether this drug would provide protection against methacholine-induced and exercise-induced bronchoconstriction. Unexpectedly, we found that the higher doses actually induced bronchoconstriction in a majority of subjects.
MATERIALS AND METHODS
Selection of Subjects
A total of 13 subjects were enrolled in the study; ten participated in both the methacholine challenge and exercise phases, whereas three participated only in the exercise study. Subjects were 19 to 31 years of age (mean, 21 years) with a history of mild intermittent asthma. The concentration of methacholine required to decrease
Table 1--Demographic Data and Documentation of Airway Hyperreactivity Prior to Entrance into Study
[FEV.sub.1] by 20 percent from baseline ([PC.sub.20]) was 12 mg/ml or less at entrance into the study (Table 1). No subject had required corticosteroids or hospitalization for asthma or had had a viral respiratory tract infection in the previous 60 days. None of the subjects had been seen in an emergency room for treatment of acute asthmatic symptoms in the previous 30 days.
On baseline evaluation, each subject was required to have an [FEV.sub.1] value of 70 percent of predicted or more, and on each study day the [FEV.sub.1] was within 90 to 110 percent of the previous evaluation. Before each study, theophylline was withheld for 24 to 48 hours, inhaled albuterol for at least 12 hours, and inhaled isoproterenol for at least 4 h. Studies were conducted at the same time each day in the same laboratory, where temperature and humidity were kept constant. The protocol was approved by the University of Florida Health Center Institutional Review Board, and written informed consent was obtained from each subject. An investigator-sponsored IND was filed with the Food and Drug Administration.
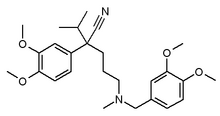
Administration of Inhaled Verapamil
Inhaled verapamil was prepared by dissolving verapamil hydrochloride powder (Knoll Pharmaceuticals, Inc.) in physiologic saline solution containing 5 percent ethanol and 2 percent propylene glycol. The pH was adjusted to 6.4 with a solution containing 0.5 percent sodium chloride and 0.375 percent sodij bicarbonate. The final verapamil concentration was 80.0 mg/ml. Each dose was prepared by diluting aliquots of the stock solution with an appropriate volume of physiologic saline solution containing 5 percent ethanol and 2 percent propylene glycol to increase solubility, such that the final volume was always 3.0 ml with an osmolarity of 1,100 m0sm or less. Placebo was diluent alone.
Doses were placed in an updraft nebulizer (Hudson model 1734T) driven by an air compressor (DeVilbiss 561). The mean output from the updraft nebulizer was 0.267 [+ or -] 0.015 ml/min ([+ or-]SD). The nebulizer was attached to a T-tube, with the subject breathing through one side of this tube through a low-dead-space one-way valve, in order to reduce loss of dose to the atmosphere. From the mouthpiece the system delivered an aerosol with an aerodynamic mass median diameter of 4.6 [mu]. Aerosol particle size and osmolarity did not appear to vary with drug concentration. Each dose required 10 to 12 minutes to nebulize.
Methacholine Study
Bronchial Provocation. Methcholine challenge was performed by a modification of the method of Cockcroft et al. [15] Several strengths of methacholine hydrochloride solution were prepared from powder (J.T. Baker Chemical Co.), and the same lot was used for all subjects. Baseline spirometric data (Collins survey spirometer) consisted of FVC, [FEV.sub.1], and FEF25-75%. Values were calculated with a microprocessor (Eagle I; Warren E. Collins, Inc). The best of three attempts was recorded and expressed both as actual values and as percent predicted for age, gender, and height. [16]
Bicarbonate-buffered saline solution, pH 7.4 (Albaye, Hollister-Stier), was inhaled for 2 min from a Wright nebulizer (Roxon MediTech) driven by 50-psi compressed oxygen at 7 L/min. The Wright nebulizer was precisely calibrated to provide an output of 0.13 ml/min. A single spirometric maneuver was performed at 30, 90, and 180 seconds after inhalation and was repeated thereafter at 2 min intervals until the lowest [FEV.sub.1] was obtained.
On each study day the initial concentration of methacholine was two twofod dilutions below the [PC.sub.20] value obtained on the study qualifying day (Table 1). The methacholine solution was nebulized for 2 min and spirometry repeated (as described previously) until the lower [FEV.sub.1] was recorded. This procedure was repeated with twofold increasing concentrations of methacholine until [FEV.sub.1] was decreased by 20 percent or more. The change in [FEV.sub.1] was calculated as follows:
% [Delta] [FEV.sub.1] = lowest [FEV.sub.1] (diluent)-lowest [FEV.sub.1] (methacholine) / lowest [FEV.sub.1] (diluent) X 100
The dose of methacholine required to produce a 20 percent decrease in [FEV.sub.1] ([PC.sub.20]) was interpolated graphically from the last two data points of the plot of percent change in [FEV.sub.1] and log-dose methacholine.
Experimental Design. Subjects inhaled placebo (diluent alone) or 5, 10, 20, 40, 80, or 160 mg of verapamil in a single-blind crossover design. One dose was administered per day at least 48 hours after the previous dose, and each subject completed the entire study within 15 days. Placebo was randomized in the first three study days, but for safety reasons, verapamil was given sequentially from low to high dose.
Spirometry, methacholine [PC.sub.20], blood pressure, heart rate, and the P-R interval of the ECG were measured 2 h before and 15 minutes after each test dose. The dose was administered after [FEV.sub.1] returned to within 90 to 110 percent of baseline. Previous studies conducted in our laboratory indicated that serial methacholine challenges performed at intervals of 2 or more hours were not associated with either a carryover effect or tachyphylaxis. [11] In addition, the fact that the 95 percent confidence interval for the mean [PC.sub.20] ratio after and before placebo was 0.9 to 1.2 in the present study provides further evidence that the interval between challenges was appropriate.
When the second [PC.sub.20] was reached, a 10-ml sample of blood was obtained for measurement of serum concentrations of verapamil and its principal metabolite, norverapamil. The P-R interval was calculated as the average of ten consecutive beats measured from lead 2 of a single-channel electrocardiograph.
Data Analysis. The effect of verapamil on airway reactivity to metacholine was expressed as the ratio of [PC.sub.20] after drug or placebo administration to the [PC.sub.20] before the dose. This drug activity ratio (DAR) represents the increase in [PC.sub.20] resulting from verapamil (decrease in airway reactivity).
Exercise Study
Bronchial Provocation. Subjects were asked not to exercise prior to reporting to the laboratory. The exercise challenge was standardized by altering the treadmill incline and speed over 3 to 4 minutes in order to achieve target conditions of a minute ventilation of 55 percent to 65 percent of calculated maximum voluntary ventilation based on the subject's measured [FEV.sub.1] [17] while not exceeding 75 percent to 85 percent of maximum predicted heart rate. [18] Minute ventilation was used as an end point because of the possibility that verapamil would decrease heart rate. If this had occurred, subjects would have received unequal work loads between treatment regimens. Heart rate was monitored continuously during the exercise period, while minute ventilation and oxygen consumption were measured in a breath-by-breath fashion (Beckman Metabolic Measurement Cart). During exercise, subjects breathed ambient air maintained between 22[Degrees]C and 24[Degrees]C and 40 percent to 50 percent relative humidity.
Subjects were exercised at target conditions for 6 minutes. Spirometry was performed before and at 3, 5, 8, 10, and 15 minutes after exercise.
Experimental Design. Placebo (diluent alone) and two dose levels of verapamil were given in a double-blind randomized crossover manner on different days at least 48 hours apart. The lower dose of verapamil was 10 mg, since it produced the largest effect without inducing bronchoconstriction during the methacholine study. The high dose was the highest dose tolerated during the methacholine phase: five subjects received 20 mg; three subjects received 40 mg; one subject received 80 mg and one subject received 160 mg.
Spirometry, blood pressure, heart rate, and the P-R interval of the ECG were measured before and 15 minutes after the diltiazem dose and, again, at the completion of the exercise. In addition, a 10-ml sample of blood was obtained at the end of the exercise challenge for measurement of verapamil and norverapamil concentrations in serum.
Data Analysis. The maximum percent change in [FEV.sub.1] induced by exercise was calculated as follows:
% [Delta] [FEV.sub.1] = postdose [FEV.sub.1] - lowest postexercise [FEV.sub.1] / postdose [FEV.sub.1] X 100
Measurement of Verapamil in Serum
Verapamil and nonverapamil were measured in serum by reverse-phase high-pressure liquid chromatography using an ultraviolet detector (J. Pieper, unpublished data). The assay has a sensitivity of 25 ng/ml and a coefficient of variation for between-day precision of 6.4 percent at 75 ng/ml (n = 10). Recovering of verapamil from serum is 83 percent with this method.
Statistical Analysis
Methacholine Study. An analysis of variance for repeated measures (ANOVA) was used to evaluate differences between treatments in predose to postdose changes in [PC.sub.20], blood pressure, and the P-R interval of the ECG. Duncans multiple range test was used to determine the source of a difference when ANOVA was significant. Results were considered statistically significant at p<0.05. Since not all patients were able to complete the methacholine study, a paired t-test then was used to compare DAR values of subjects who completed 5, 10, 20, and 40 mg with the placebo DAR. To compensate for the use of multiple t-tests, p<0.02 was accepted as statistically significant (0.05 / 4 t-tests).
Exercise Study. An ANOVA, as described previously, was used to compare minute ventilation, oxygen consumption, heart rate, and maximum percent decrease in [FEV.sub.1] after exercise during the two dose levels of verapamil and placebo for the ten subjects able to tolerate both doses. Results were considered statistically significant at p<0.05.
Unless indicated otherwise, all results are expressed as mean [+ or -] SEM to indicate the range of mean values that would be obtained if these experiments were repated several times.
RESULTS
Methacholine Challenge
Ten subjects completed the methacholine study. The FVC, [FEV.sub.1] and FEF25-75% were not significantly altered after placebo or 5, 10, or 20 mg of verapamil (Fig 1); however, cough, wheezing, and decreases in [FEV.sub.1] of greater than 10 percent occurred in two subjects after 20 mg, in five subjects after 40 mg, and in two subjects after 80 mg. Consequently, the mean [FEV.sub.1] for the group was significantly reduced at the 40-mg dose (Fig 1). Postdose methacholine challenge was not performed when [FEV.sub.1] decreased by 10 percent or more.
The methacholine challange procedure was reproducible, with a mean ([+ or -] SEM) ratio of [PC.sub.20] after placebo to [PC.sub.20] before placebo (DAR) of 1.1 [+ or -] 0.1 (Fig 2). The 95 percent confidence interval for the mean DAR during placebo was 0.9 to 1.2.
The maximum DAR of 2.1 [+ or -] 0.2 occurred after the 10-mg dose (p<0.001). The 5-mg and 20-mg doses of verapamil did not produce a statistically significant change in DAR from placebo (p>0.01) (Fig 2). No changes in cardiovascular parameters occurred at any dose. Serum concentrations of verapamil showed an increase in proportion to dose. Metabolite concentrations were absent in most subjects (Table 2).
Exercise Challenge
Thirteen subjects completed the exercise study. Three were unable to complete the higher dose regimen because of bronchoconstriction. Their data are not included in the analysis. Baseline [FEV.sub.1] was 88 [+ or -] 3 percent of predicted after placebo, 87 [+ or -] 3 percent of predicted after 10 mg of verapamil, and 89 [+ or -] 3 percent of predicted after the high-dose treatment (p>0.05) (Table 3). The nebulized doses had no significant effect on spirometric data. There was no significant difference in minute ventilation, oxygen consumption, or heart rate on the three study days, indicating that treatmill work load was the same on each treatment regiment; for example, oxygen consumption was 32.7 [+ or -] 1.4 ml/min/kg after placebo, 33.2 [+ or -] 1.4 ml/min/kg after 10 mg, and 33.4 [+ or -] 1.8 ml/min/kg
Table 2--Mean ([+ or -] SEM) Serum Concentrations of Verapamil and Norverapamil after Placebo and Increasing Doses of Inhaled Verapamil during Methacholine Study
after the high-dose regimen (p>0.05). The mean maximum change in [FEV.sub.1] was -17.1 [+ or -] 4.0 percent after placebo, -12.7 [+ or -] 4.3 percent after 10 mg of verapamil, and -6.4 [+ or -] 3.5 percent after high-dose verapamil (p<0.05). The difference between the high dose and 10 mg was not statistically significant. There were no significant effects on the P-R interval of the ECG between the three regimens of treatment. Serum concentrations of verapamil and norverapamil were similar to those measured during the methacholine study and did not correlate with maximum percentage of decrease in [FEV.sub.1] (not shown).
DISCUSSION
As previously noted, most prior studies of calcium channel blockers in asthma have used a single dose level. In this study, administration of verapamil by inhalation allowed us to study large doses delivered directly to the airways without producing untoward cardiovascular effects. We demonstrated that both 10 mg and a "high dose" (20 to 160 mg) of inhaled verapamil modestly, but significantly, inhibited exercise-induced bronchoconstriction (Table 3). Overall, the degree of protection from exercise-induced bronchconstriction was similar in magnitude to that afforded by cromoly, [19,20] but much less than the effect of [[Beta]sub.2]-adrenergic agonists. [20,21]
We also found that the 10-mg dose of verapamil significantly attenuated methacholine-induced bronchoconstriction; however, higher doses did not afford greater protection (Fig 2) and were not well tolerated. The failure to completely protect against methacholine-induced bronchoconstriction may relate to the cellular mechanisms by which methacholine induces bronchoconstriction. Acetylcholine at lower concentrations ([10.sup.-7] M) causes calcium influx through voltage-dependent channels in canine trachealis smooth muscle, whereas at higher concentrations ([10.sup.-4] M), calcium influx predominantly occurs through receptor-operated channels. [2] Since verapamil works primarily on voltage-operated calcium channels, [22,23] it therefore has little effect on methacholine-induced bronchoconstriction.
Interestingly, inhaled verapamil, at doses greater than 10 mg, caused bronchoconstriction. Seven of our ten subjects experienced cough, wheeze, and a greater than 10 percent decrease in [FEV.sub.1] at the higher doses. This did not occur with placebo (diluent alone) and was not due to hyperosmolarity of the nebulized solution, since all doses of the active drug and placebo had a similar osmolarity. Moreover, this adverse effect was not observed in an identical study that we conducted with inhaled gallopamil, the methoxy derivative of verapamil. [11] This bronchocostrictor effect may be related to a weak [Beta]-adrenergic antagonist effect of verapamil. Feldman et al, [24] using a radioligand binding technique, found that verapamil and its major
[TABULAR DATA OMITTED]
metabolite, norverapamil, have a strong affinity for the human lymphocyte [[Beta].sub.2]-adrenergic receptor in vitro. The binding characteristics were those of a [Beta]-adrenergic receptor antagonist. Thus, bronchoconstriction after verapamil inhalation could be related to [[Beta].sub.2]-adrenergic receptor antagonism. Because of this antagonistic effect, it is also possible that our finding of only modest attenuation of methacholine-induced bronchoconstriction by the 10-mg dose resulted from concurrent [[Beta].sub.2]-adrenergic receptor antagonism which, in part, counterbalanced the beneficial effect.
CONCLUSION
Inhaled verapamil at low dosage does not alter resting bronchomotor tone but has a modest protective effect against exercise-induced and methacholine-induced bronchoconstriction; however, at higher doses, inhaled verapamil induces bronchoconstriction, probably by [[Beta].sub.2]-adrenergic receptor antagonism. These data suggest that high doses of verapamil administered systemically should be used with caution in asthmatic patients.
REFERENCES
[1] Middleton E Jr. Antiasthmatic drug therapy and calcim ions: review of pathogenesis and role of calcium. J Pharm Sci 1980; 69:243-51
[2] Barnes PJ. Clinical studies with calcium antagonists in asthma. Br J Clin Pharmacol 1985; 20:2895-985
[3] Patel KR. The effect of verapamil on histamine- and methacholine-induced bronchoconstriction. Clin Allergy 1981; 11:441-47
[4] Corris PA, Nairman S, Gibson GJ. Nifedipine in the prevention of asthma induced by exercise and histamine. Am Rev Respir Dis 1983; 128:991-92
[5] McIntyre E, Fitzgibbon B, Otto H, Minson MB, Alpers J, Ruffin R. Inhaled verapamil in histamine-induced bronchoconstriction. J Allergy Clin Immunol 1983; 71:375-81
[6] Popa VT, Somani P, Simon V. The effect of inhaled verapamil on resting bronchial tone and airway contractions induced by histamine and acetylcholine in normal and asthmatic subjects. Am Rev Respir Dis 1984; 130:1006-13
[7] Ahmed T, Russi E, Kim CS, Danta I. Comparative effects of oral and inhaled verapamil on antigen-induced bronchoconstriction. Chest 1985; 88:176-80
[8] Cuss FM, Barnes PJ. The effect of inhaled nifedipine on bronchial reactivity to histamine in man. J Allergy Clin Immunol 1985; 76:718-23
[9] Hartmann V, Magnussen H. Effect of diltiazem on histamine- and carbachol-induced bronchospasm in normal and asthmatic subjects. Chest 1985; 87:174-79
[10] Patel KR, Tullett WM. Comparison of two calcium antagonists, verapamil and gallopamil (D-600), in exercise-induced asthma. Eur J Respir Dis 1985; 67:269-71
[11] Massey KL, Hill M, Harman E, Rutledge D, Ahrens R, Hendeles L. Dose-response of inhaled gallopmail (D-600), a calcium channel blocker, in attenuating airway reactivity to methacholine and exercise. J Allergy Clin Immunol 1988; 81:912-18
[12] NAwarth H, Blei I, Generg R, Ludwig C, Zong X. No stereo-specific effects of the optical isomers of verapamil and D-600 on the heart. In: Zanchetti A, Krikler DM, eds. Calcium antagonism in cardiovascular therapy. Amsterdam: Excerpta Medica, 1981:52
[13] Himori N, Taira N. Differential effects of the calcium-antagonistic vasodilators, nifedipine and verapamil, on the tracheal musculative and vaculature of the dog. Br J Pharmacol 1980; 68:595-97
[14] Carpenter H, Chapman GA, Singer S, Abraham W, Ahmed T. Effect of gallopamil, a calcium channel blocker on carbachol and histamine-induced bronchoconstriction in sheep in vivo and in vitro. Am Rev Respir Dis 1986; 133:A-14
[15] Cockcroft DW, Killian DN, Millon JJA, Hargreave FE. Bronchial reactivity to inhaled histamine: a method and clinical survey. Clin Allergy 1977; 7:235-43
[16] Morris JF, Koski A, Johnson LC. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis 1971; 103:57-67
[17] Mohan-Kumar T, Gimenez M. Maximal ventilation at rest and exercise in patients with chronic pulmonary disease. Respiration 1984; 46:291-302
[18] Eggleston PA, Rosenthal RR, Anderson SA, Anderton R, Bierman SW, Bleecker ET, et al. Guildelines for the methodology of exercise challenge testing of asthmatics. J Allergy Clin Immunol 1979; 64:6442-45
[19] Pollock J, Kiechel MF, Cooper D, Weinberger M. Relationship of serum theophylline concentration to inhibition of exercise-induced bronchospasm and comparison with cromolyn. Pediatrics 1977; 60:840-44
[20] Bundgaard, Rasmussen FV, Madsen L. Pretreatment of exercise-induced asthma in adults with aerosols and pulverized tablets. Allergy. 1980; 35:39-45
[21] Anderson SD, Seale JP, Rozea P, Bandler L, Theobald G, Lindsay DA. Inhaled and oral salbutamol in exercise-induced asthma. Am Rev Respir Dis 1976; 114:493-500
[22] Farley JM, Miles PR. The sources of calcium for acetylcholine induced contractions of dog tracheal smooth muscle. J Pharmacol Exp Ther 1978; 207:340-55
[23] Colburn RF. Electromechanical coupling in canine trachealis muscle: acetylcholine contractions. Am J Physiol 1979; 236:C177-84
[24] Feldman RD, Park GD, Laicy CY. The interactions of verapamil and norverapamil with beta-adrenergic receptors. Circulation 1985; 72:547-54
COPYRIGHT 1991 American College of Chest Physicians
COPYRIGHT 2004 Gale Group