IN THIS ARTICLE, I'll acquaint you with 11 new drugs introduced in the second half of 2002, including:
* voriconazole, a new treatment for invasive aspergillosis and other dangerous fungal infections
* adefovir dipivoxil and peginterferon alfa-2a, antiviral therapies for hepatitis B and hepatitis C, respectively
* alosetron HCl, a drug for diarrhea-predominant irritable bowel syndrome (IBS) that was taken off the market in 2000 because of dangerous complications related to constipation, and tegaserod maleate, approved for women with IBS whose primary symptom is constipation.
Unless otherwise specified, the information in the following summaries applies to adults, not children. Consult the package insert for information regarding each drug's safety during pregnancy and breast-feeding. Also consult the package insert, your pharmacist, or a comprehensive drug reference for more details on precautions, drug interactions, and adverse reactions* for all drugs.
Antifungal drug
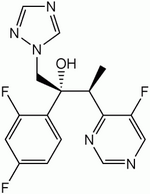
Voriconazole
Effective treatment for aspergillosis with fewer adverse effects
Indicated to treat invasive aspergillosis, voriconazole (Vfend, Pfizer) is the newest triazole antifungal drug on the market, joining fluconazole and itraconazole. Like these two previously marketed drugs, voriconazole is available in both oral and parenteral forms.
Each year, about 50,000 Americans experience invasive aspergillosis. This difficult-to-treat and potentially fatal fungal infection most often affects cancer patients receiving chemotherapy and patients who've received organ or bone marrow transplants. The standard treatment, amphotericin B, must be given parenterally and causes adverse reactions in almost all patients.
Voriconazole, which may be used as the primary treatment for invasive aspergillosis, was shown to be more effective and better tolerated than amphotericin B in a comparative study. Voriconazole is also indicated for treatment of several other serious fungal infections in patients who are unresponsive to or intolerant of other therapy.
The most common adverse reactions associated with voriconazole are visual disturbances. Affecting nearly 30% of patients, they're generally mild and reversible.
From 15% to 20% of Asian patients may metabolize voriconazole poorly because of a genetic problem affecting the CYP 2C19 pathway. These patients should be monitored closely and the dosage of voriconazole adjusted if indicated. The prevalence of poor metabolizers among white and black patients is 3% to 5%.
Precautions: (1) Use voriconazole with caution in patients with a history of sensitivity to other drugs in its class. The potential for cross-hypersensitivity is unknown. (2) Closely monitor patients during intravenous (I.V.) infusion of voriconazole for anaphylactoid reactions, which occurred infrequently during trials. (3) Because voriconazole tablets contain lactose, don't give them to patients with such rare hereditary problems as galactose intolerance, Lapp lactose deficiency or glucose-galactose malabsorption. (4) Voriconazole has the potential to interact with many other drugs. See the product insert for details. (5) Monitor liver function tests at the start of and during therapy with voriconazole because of rare reports of serious hepatic reactions (hepatitis, cholestasis, and liver failure). (6) Don't use I.V. voriconazole in patients with moderate to severe renal failure unless the expected benefit justifies the risk of drug accumulation. (7) Closely monitor patients for Stevens-Johnson syndrome, a rare adverse reaction reported in clinical studies. (8) In patients with mild to moderate hepatic cirrhosis, reduce the maintenance dosage of voriconazole by half. (The drug's safety for patients with severe hepatic cirrhosis hasn't been evaluated.)
Adverse reactions: visual disturbances (altered visual perceptions, blurred vision, color vision change, photophobia), increased alanine aminotransferase (ALT) and aspartate aminotransferase (AST) concentrations, increased creatinine concentrations, dermatologic reactions such as rash, fever, vomiting, hallucinations, anaphylactoid reactions during I.V. infusions of the drug (flushing, fever, sweating, tachycardia, chest tightness, dyspnea, rash)
Supplied as: 50-mg and 200-mg tablets and single-use vials containing 200 mg of the drug and 3,200 mg of SBECD, a solubilizing agent
Dosage:
* I.V.: After reconstitution and dilution, administer a loading dose of 6 mg/kg every 12 hours for two doses, followed by a maintenance dosage of 4 mg/kg every 12 hours. Infusions should run over 1 to 2 hours at a maximum rate of 3 mg/kg/hour.
* Oral: 200 mg every 12 hours in patients weighing more than 88 pounds (40 kg) and 100 mg every 12 hours in patients weighing less than 88 pounds. May be increased to 300 mg every 12 hours in patients weighing more than 88 pounds and 150 mg every 12 hours in patients weighing less than 88 pounds.
Nursing considerations:
(1) Because of the potential for vision changes, advise the patient to avoid driving at night during treatment and to avoid other potentially hazardous activities if he perceives visual changes. Also tell him to avoid strong direct sunlight. (2) Teach him to take voriconazole tablets at least 1 hour before or 1 hour after a meal. (3) Reconstitute and dilute the I.V. formulation as directed in the product insert. Discard any unused solution in the vial. (4) Don't dilute voriconazole with 4.2% sodium bicarbonate infusion, which may degrade the drug, and don't infuse the solution into the same line with other drugs or parenteral nutrition. (5) Monitor the patients response to treatment. If he doesn't tolerate treatment, the I.V. maintenance dosage should be reduced to 3 mg/kg every 12 hours and the oral maintenance dosage reduced in 50-mg increments to 200 mg every 12 hours (for patients weighing more than 88 pounds). (6) If the patient is taking warfarin, monitor the anticoagulant response closely; voriconazole may increase warfarin's action. Check the product insert for other potential drug interactions.
Drugs for hepatitis
Adefovir dipivoxil
New option for treating hepatitis B
Adefovir dipivoxil (Hepsera, Gilead Sciences) has been approved for treatment of chronic hepatitis B virus (HBV) infection in adults with evidence of active viral replication and either evidence of persistent elevations in serum aminotransferases (ALT or AST) or active disease. When adefovir was initially investigated as a treatment for human immunodeficiency virus (HIV) infection, studies were stopped because of problems with nephrotoxicity. However, researchers learned that a considerably lower and safer dosage is effective against HBV.
Adefovir inhibits HBV DNA polymerase (reverse transcriptase) and includes activity against some HBV isolates that are resistant to lamivudine, which is also indicated for HBV infection. So far, resistance to adefovir hasn't been a problem.
Although adefovir is active against HIV, the effective dosage is far higher than that recommended for treating HBV This lower dosage would encourage HIV resistance if adefovir were inadvertently given to a patient with HIV infection. Consequently, HIV antibody testing should be offered to patients before treatment with adefovir begins.
Most patients tolerate adefovir well, but the drug's potential for serious adverse reactions merits a black-box warning regarding nephrotoxicity, lactic acidosis, HIV resistance in patients with unrecognized or untreated HIV infection, and severe exacerbation of hepatitis when therapy is discontinued.
Precautions: (1) Use caution in patients taking other drugs that may impair renal function, such as aminoglycosides, vancomycin, cyclosporine, tacrolimus, and nonsteroidal anti-inflammatory drugs. (2) Reduce the dosage of adefovir in patients with impaired renal function (creatinine clearance less than 50 ml/minute) and monitor renal function in all patients. (3) Monitor for lactic acidosis and severe hepatomegaly with steatosis. These rare but dangerous adverse reactions are associated with nucleoside reverse transcriptase inhibitors, which have properties similar to adefovir. Most people experiencing these problems are women; other risk factors include liver disease, obesity, and prolonged drug therapy. (4) If treatment is discontinued, closely monitor for severe acute exacerbation of hepatitis, which may be fatal.
Adverse reactions: asthenia, headache, abdominal pain, nausea
Supplied as: 10-mg oral tablets
Dosage: 10 mg once a day. In patients with impaired renal function: 10 mg every 48 or 72 hours, depending on creatinine clearance (see product labeling for details). In hemodialysis patients: 10 mg every 7 days following dialysis
Nursing consideration: Tell the patient that he may take the drug without regard to food.
Peginterferon alfa-2a
Longer-lasting action against hepatitis C
Indicated for use alone or in combination with ribavirin, peginterferon alfa-2a (Pegasys, Roche) is indicated to treat chronic hepatitis C virus (HCV) infection in adults who have compensated liver disease and who haven't been previously treated with interferon alfa. The drug's "pegylated" form gives it a longer duration of action than interferon alfa-2a.
Administered once weekly by subcutaneous (S.C.) injection, peginterferon alfa-2a has been approved for combination therapy with ribavirin, which the patient takes orally twice a day. The two drugs will almost always be used together.
The recommended duration of treatment for most patients is 48 weeks. However, in patients with HCV genotypes 2 and 3, the recommended duration is 24 weeks because longer periods of treatment haven't improved the response.
Like other alfa interferons, peginterferon alfa-2a has a black-box warning alerting practitioners to the potential for causing or aggravating life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Although uncommon, depression, suicide, drug abuse relapse, and serious bacterial infections have been associated with these drugs. Ribavirin is also associated with many serious adverse reactions, including fetal death and birth defects, so carefully review product labeling.
Precautions: (1) Contra-indicated in patients with autoimmune hepatitis or hepatic decompensation and in infants. (2) Use extreme caution in patients with a history of depression. (3) Use with caution in patients with cardiovascular, pulmonary, or endocrine disease and in those with autoimmune disorders. (4) Use caution in patients with ophthalmologic disorders, such as diabetic or hypertensive retinopathy, because alfa interferons can cause or aggravate these conditions. All patients should have eye examinations before starting therapy, and those with eye problems should be monitored regularly. (5) Use caution in patients with baseline neutrophil counts less than 1,500 cells/mm^sup 3^; baseline platelet counts less than 90,000 cells/mm^sup 3^; or baseline hemoglobin less than 10 grams/dl. (6) Concurrent use of ribavirin isn't recommended in patients whose creatinine clearance is less than 50 ml/minute.
Adverse reactions: fatigue/asthenia, fever, rigors, headache, myalgia, arthralgia, irritability/anxiety/nervousness, insomnia, depression, anorexia, nausea/vomiting, injection-site reactions, alopecia, dizziness, dyspnea, pruritus, dermatitis, neutropenia
Supplied as: single-use vials containing 180 mcg of drug in 1 ml of solution
Dosage: 180 mcg S.C. once a week, on the same day each week. See the product labeling for dosage adjustments in patients experiencing depression or hematologic toxicity.
Nursing considerations: (1) Teach the patient to administer peginterferon alfa-2a in the abdomen or thigh and to rotate injection sites. (2) If he's also taking ribavirin (800 to 1,200 mg/day divided into two doses), tell him to take each dose with breakfast and dinner because food increases its bioavailability. (3) Tell him to store vials of peginterferon alfa-2a in the refrigerator and not to shake them. (4) Teach him to report symptoms of depression or suicidal thoughts to his practitioner. (5) Encourage him to keep appointments for eye examinations and blood tests. (6) Tell him that he can lessen the effects of flulike symptoms associated with peginterferon alfa-2a by administering the drug at bedtime and by taking acetaminophen. (7) If a female patient will be taking ribavirin, which causes fetal death and birth defects, rule out pregnancy before starting treatment. Teach her to use two forms of contraception during treatment and for at least 6 months after treatment ends. Female partners of men undergoing therapy should take the same precautions.
Antihyperlipidemic drug
Ezetimibe
Lipid-lowering drug with a unique mechanism of action
The first of a new class of lipid-lowering drugs, ezetimibe (Zetia; Merck, Schering) inhibits the intestinal absorption of cholesterol and related phytosterols. It's indicated as an adjunct to diet, as monotherapy, or in combination with a statin drug such as lovastatin to treat primary hypercholesterolemia. It's also indicated for two rare genetic disorders, homozygous familial hypercholesterolemia and homozygous sitosterolemia. It's the first drug to win approval for the latter condition.
By itself, ezetimibe is less effective than statins at lowering cholesterol. But it's safe and well tolerated-in trials, most adverse reactions occurred at a rate only slightly higher than placebo-so it can be added to a statin regimen to further reduce serum cholesterol concentrations without increasing the risk of adverse reactions associated with a higher statin dosage. Myopathy and rhabdomyolysis, rare but serious adverse reactions linked to statins, aren't associated with ezetimibe.
Precautions: (1) If ezetimibe is used with a statin, perform liver function tests when treatment starts and subsequently as recommended for the statin being used. (2) Use of ezetimibe with a fibrate derivative (such as gemfibrozil or fenofibrate) isn't recommended because of the potential for cholelithiasis. (3) Closely monitor patients taking ezetimibe and cyclosporine concurrently; cyclosporine may increase ezetimibe concentrations significantly. (4) Ezetimibe isn't recommended for patients with moderate or severe hepatic insufficiency.
Adverse reactions: diarrhea, abdominal pain, back pain, arthralgia, sinusitis
Supplied as: 10-mg oral tablets
Dosage: 10 mg/day
Nursing considerations: (1) Ezetimibe can be taken without regard to food. (2) Give ezetimibe at least 2 hours before or at least 4 hours after administration of cholestyramine or another bile acid sequestrant; these drugs may reduce the absorption and activity of ezetimibe. (3) If the patient is taking ezetimibe with a statin, he can take doses of the two drugs together.
Drugs for IBS
Alosetron HCl
IBS drug returns to market-this time, with tight controls on prescribing.
In early 2000, alosetron HCl (Lotronex, GlaxoSmithKline) was approved and marketed for women with diarrhea-predominant irritable bowel syndrome (IBS). Later that year, it was taken off the market because of reports of serious complications related to constipation, including obstruction, perforation, impaction, toxic megacolon, and secondary ischemia.
Because alosetron had been effective for many patients with diarrhea-predominant IBS whose symptoms hadn't responded to other drugs, the Food and Drug Administration (FDA) worked with the drug's manufacturer to return it to the market. Changes that make the drug safer include a lower recommended initial dosage, narrower indications for use, and tight control over prescribing and dispensing the drug.
Alosetron controls diarrhea by blocking the action of serotonin at 5-HT^sub 3^ sites in the enteric nervous system. It's indicated only for women with severe, diarrhea-predominant IBS of 6 or more months' duration who've failed to respond to conventional therapy and in whom anatomic and biochemical abnormalities of the GI tract have been ruled out. Fewer than 5% of people (about 185,000 Americans) with IBS are considered to have the severe form.
Only physicians enrolled in GlaxoSmithKline's Prescribing Program for Lotronex can prescribe the drug. Responsibilities outlined in the program include patient teaching, regular monitoring for adverse reactions, and reporting complications.
Pharmacists can dispense the drug only with written prescriptions to which a special sticker has been affixed. Telephone, fax, or computerized prescriptions aren't permitted. The drug is dispensed with a patient medication guide, package insert, and survey enrollment form. Prescribers can enroll in the program by calling 1-888-825-5249 or visiting http://www.lotronex.com.
Precautions: (1) Contraindicated in patients with constipation or a history of chronic or severe constipation, intestinal obstruction, stricture, toxic megacolon, GI perforations or adhesions, ischemic colitis, impaired intestinal circulation, thrombophlebitis or hypercoagulable state, Crohn's disease or ulcerative colitis, or diverticulitis. (2) Contraindicated in patients who can't understand or comply with conditions of the program. (3) Use caution in patients who are elderly, debilitated, or taking other medications that decrease GI motility because they're at risk for constipation. (4) Stop treatment immediately if the patient becomes constipated or develops signs of ischemic colitis (bloody diarrhea, new or worsening abdominal pain).
Adverse reactions: constipation, ischemic colitis, abdominal discomfort and pain, nausea
Supplied as: 1-mg oral tablets
Dosage: 1 mg/day for the first 4 weeks. If this dosage is well tolerated but doesn't adequately control IBS symptoms, the dosage may be raised to 1 mg twice a day.
Nursing considerations: (1) Tell the patient that she can take alosetron without regard to food. (2) Teach her to contact the prescriber immediately if she experiences constipation, rectal bleeding, or new or worsening abdominal pain. (3) If her condition doesn't improve after 4 weeks of treatment at the higher dosage, treatment with alosetron should be discontinued.
Tegaserod maleate
First drug approved for constipation-predominant IBS
In 2002, a new drug for IBS, tegaserod maleate (Zelnorm, Novartis), was approved for short-term treatment of women with IBS whose primary symptom is constipation. Tegaserod is the first drug available for this form of IBS.
Indicated for short-term treatment of women with constipation-predominant IBS, tegaserod is a serotonin receptor partial agonist that increases basal motor activity and improves GI motility. It has a unique mechanism of action and is the first drug approved for constipation-predominant IBS.
Precautions: (1) Contraindicated in patients with a history of bowel obstruction, symptomatic gallbladder disease, suspected sphincter of Oddi dysfunction, abdominal adhesions, severe renal impairment, or moderate to severe hepatic impairment. (2) Contraindicated in patients who are experiencing or frequently experience diarrhea. (3) Discontinue immediately if the patient has new or worsening abdominal pain. (4) Use with caution in patients with mild hepatic impairment.
Adverse reactions: diarrhea, abdominal pain, nausea, flatulence, headache
Supplied as: 2-mg and 6-mg oral tablets
Dosage: 6 mg twice a day before meals for 4 to 6 weeks. For patients who respond to therapy during this time, another 4 to 6 weeks of therapy may be considered. The drug's effectiveness for more than 12 weeks of therapy hasn't been tested.
Nursing considerations: (1) Teach the patient to take the drug before meals because food reduces its bioavailability. (2) Tell her that she may experience an episode of diarrhea during the first week of therapy. If diarrhea persists, or she experiences new or worsening abdominal pain, she should contact the prescriber immediately.
Antipsychotic drug
Aripiprazole
Convenient regimen encourages adherence to treatment.
Aripiprazole (Abilify; Bristol-Myers-Squibb, Otsuka) is classified as an atypical antipsychotic drug. Like others in this class (risperidone, olanzapine, quetiapine, and ziprasidone), it acts at certain dopamine and serotonin receptors.
Aripiprazole is indicated for treatment of schizophrenia. Because its actions at dopamine and serotonin receptors differ somewhat from the effects of most other antipsychotic drugs, it may help patients who haven't responded well to other drugs. Its convenient once-a-day dosage, which may improve patient adherence to therapy, is also an advantage over some of the similar drugs, such as quetiapine, that must be taken two or three times a day.
Some patients taking aripiprazole experience orthostatic hypotension, light-headedness, or syncope, so use it cautiously in patients taking antihypertensives or medications active in the central nervous system (CNS), in patients with cardiovascular or cerebrovascular disease, and in patients with conditions that would predispose them to hypotension, such as dehydration. Advise your patient to avoid alcoholic beverages, which have a CNS-depressant effect.
Other adverse reactions associated with aripiprazole include headache, anxiety, insomnia, nausea and vomiting, somnolence, akathisia, extrapyramidal symptoms, and weight gain; rarely reported adverse reactions include seizures, tardive dyskinesia, neuroleptic malignant syndrome, dysphagia, and altered body-temperature regulation. Because of the risk of impaired judgment, thinking, and motor skills, tell the patient to avoid driving and other activities requiring alertness until he's sure the medication isn't clouding his judgment.
Aripiprazole has the potential to interact with many other drugs, including other psychiatric drugs metabolized via the same enzyme pathways. If the patient is taking other drugs concurrently, consult the product labeling for precautions and recommended dosage adjustments.
Aripiprazole is supplied in 10-mg, 15-mg, 20-mg, and 30-mg oral tablets. The recommended starting dosage is 10 to 15 mg once a day without regard to food. Higher dosages haven't been proven effective. However, if the prescriber decides to raise the dose, she should wait at least 2 weeks after initiating therapy to allow the drug to achieve a steady state.
Drug for BPH
Dutasteride
Easing symptoms and reducing the need for prostate surgery
Most men over age 50 experience benign prostatic hyperplasia (BPH), characterized by urinary urgency or hesitancy, incomplete bladder emptying, incontinence, and nocturia. Symptoms can be managed with medications in some men, but in others, BPH worsens and requires surgery.
Dutasteride (Avodart, GlaxoSmithKline) joins finasteride as the second steroid 5-alpha-reductase inhibitor marketed in the United States. Both drugs inhibit the conversion of testosterone to 5-alpha-dihydrotestosterone (DHT), a potent androgen that's primarily responsible for prostate gland enlargement. In clinical studies, dutasteride reduced the risk of both acute urinary retention and BPH-related surgery. It's considered similar to finasteride in effectiveness, although the two drugs haven't been directly compared.
Dutasteride is contraindicated for use in women and in patients with a known hypersensitivity to it or to finasteride. Because suppression of DHT may cause birth defects in a male fetus, pregnant women must avoid handling dutasteride, which is supplied in a soft capsule and could be absorbed through the skin. Concentrations in semen are considered too low to jeopardize a woman who's the patient's sexual partner, even if she's pregnant. However, because of dutasteride's long half-life, it can linger in the blood for months. Consequently, a man shouldn't donate blood for at least 6 months after his last dose of dutasteride to avoid the possibility of exposing a pregnant blood transfusion recipient to the drug.
Most men tolerate dutasteride well, with no change in libido or sexual potency. However, most of the adverse reactions reported involve sexual changes: impotence, decreased libido, ejaculation disorder, and gynecomastia. Most adverse reactions abate as treatment progresses.
Dutasteride is likely to reduce levels of serum prostate-specific antigen (PSA) in the blood. Clinicians should take this into account so they don't misinterpret PSA values when screening for prostate cancer. To correctly interpret an isolated PSA value in a man treated with dutasteride for 6 months or more, the clinician should double the patient's PSA value for comparison with normal values in untreated men.
Dutasteride is metabolized via the CYP 3A4 pathway and may interact with drugs that inhibit this pathway, including clarithromycin, erythromycin, itraconazole, and HIV protease inhibitors.
Dutasteride is supplied in 0.5-mg soft gel capsules. The recommended dosage is 0.5 mg once a day, taken without regard to food.
Antineoplastic drug
Oxaliplatin
Cancer treatment wins fast FDA approval.
Oxaliplatin (Eloxatin, Sanofi-Synthelabo) was approved to treat advanced colorectal cancer under provisions of the FDA's accelerated approval process. Although no patients in the trial groups experienced a complete response, oxaliplatin helped some patients who'd have otherwise been out of options.
Oxaliplatin, as part of a treatment regimen that includes fluorouracil and leucovorin, is indicated for metastatic colon or rectal cancer that's recurred or progressed within 6 months of completion of first-line therapy with the combination of bolus fluorouracil/leucovorin and irinotecan. It's contraindicated in patients with a history of allergy to any platinum-based drug.
Possible adverse reactions include the following:
* acute, reversible peripheral neuropathy. More than half of patients in trials experienced peripheral neuropathy within 2 days of dosing. This typically resolved within 14 days but recurred with further dosing. Because symptoms may be triggered or exacerbated by cold temperatures or cold objects, tell your patient to avoid cold drinks and ice and to cover exposed skin before going out into the cold.
* persistent peripheral neuropathy (lasting more than 14 days). This reaction may also include deficits in proprioception that interfere with ordinary activities, such as writing and walking. Some patients improve after therapy ends.
* hematologic adverse reactions, including anemia, leukopenia, neutropenia, and thrombocytopenia. Monitor the patient's white blood cell count, platelets, hemoglobin, and blood chemistries before each cycle of chemotherapy.
* GI adverse reactions, including diarrhea, abdominal pain, stomatitis, nausea, and vomiting. Premedicate the patient with antiemetics, as ordered.
* fatigue, fever, back pain, edema, dyspnea, and coughing.
A few patients using oxaliplatin have developed pulmonary fibrosis. If your patient develops unexplained respiratory symptoms, treatment should be stopped until pulmonary fibrosis or interstitial lung disease can be ruled out.
Oxaliplatin is supplied in single-use vials containing 50 or 100 mg of oxaliplatin. For more details on preparing the drug, see the product insert.
Oxaliplatin is incompatible with alkaline medications or solutions, such as basic solutions of fluorouracil. Don't mix oxaliplatin with these solutions or administer it simultaneously through the same line. After administering oxaliplatin, flush the infusion line with 5% dextrose injection before administering any other medication.
Because aluminum can degrade platinum compounds, don't use needles or I.V. administration sets that contain any aluminum parts that could come in contact with the drug.
Uricolytic drug
Rasburicase
Controlling uric acid concentrations in children who need chemotherapy
In some patients with cancer, the rapid turnover of malignant cells or the initiation of chemotherapy leads to tumor lysis syndrome, which is characterized by hyperuricemia, hyperkalemia, hyperphosphatemia, and acute renal failure. Tumor lysis syndrome is associated with excess uric acid in the plasma and urine. When the uric acid concentration in urine exceeds its solubility, crystals form in the renal tubules, triggering renal insufficiency or failure.
Produced by recombinant DNA technology, rasburicase (Elitek, Sanofi-Synthelabo) is indicated for the initial management of plasma uric acid concentrations in pediatric patients with leukemia, lymphoma, and solid tumor malignancies who are receiving chemotherapy expected to result in tumor lysis and elevation of plasma uric acid. In one clinical study, uric acid concentrations were significantly reduced within 4 hours of the first dose of rasburicase. Standard treatment with allopurinol, a drug that prevents uric acid formation but has no effect on existing uric acid, doesn't significantly reduce uric acid concentrations for 1 to 3 days.
Because of rare reports of serious adverse reactions, rasburicase has black-box warnings regarding the potential for hemolysis, methemoglobinemia, and anaphylaxis. Rasburicase should be immediately discontinued if the patient experiences symptoms of an allergic reaction.
Rasburicase is contraindicated in patients with a deficiency of glucose-6-phosphate dehydrogenase (G6PD) because they may experience severe hemolysis. Patients of African or Mediterranean descent, who may be at higher risk for G6PD deficiency, should be screened before starting rasburicase therapy.
Treatment with rasburicase should be stopped immediately in patients who experience methemoglobinemia or hemolysis, and future use of the drug is contraindicated.
The most frequently reported adverse reactions associated with rasburicase are vomiting and fever. Others include nausea, headache, abdominal pain, constipation, diarrhea, respiratory distress, sepsis, neutropenia, mucositis, and rash.
At room temperature, rasburicase causes enzymatic degradation of the uric acid in blood specimens, which may result in misleadingly low plasma uric acid assay readings. To prevent inaccurate results, follow a special specimen handling procedure as detailed in the product labeling. This includes collecting blood into prechilled tubes containing heparin and immediately immersing the specimens in an ice water bath. Specimens must remain in the ice water and be analyzed within 4 hours of collection.
The recommended dosage of rasburicase is 0.15 or 0.2 mg/kg as a single daily dose for 5 days. The effectiveness and safety of therapy has been established only for a single 5-day course of therapy, so continuing or repeating therapy isn't recommended.
Rasburicase is supplied in cartons containing three single-use vials, each containing 1.5 mg of the drug, as well as three ampules containing 1 ml of diluent. Store the drug and diluent in the refrigerator.
To reconstitute the drug, add 1 ml of diluent to each vial of medication ordered and mix the solutions by swirling the vial very gently (don't shake). Remove the quantity of reconstituted solution needed to provide the ordered dose from the vial and inject it into an infusion bag containing the appropriate volume of 0.9% sodium chloride injection to achieve a final volume of 50 ml.
Administer the drug by I.V. infusion over 30 minutes (never as a bolus infusion). Don't use a filter. Initiate chemotherapy 4 to 24 hours after the first rasburicase dose and provide I.V. hydration as ordered.
Refrigerate reconstituted solution and use it within 24 hours of preparation. If possible, infuse it through a different line than that used for other drugs. If you can't use a separate line, flush the line with at least 15 ml of 0.9% sodium chloride before and after the rasburicase infusion.
Anticataplectic drug
Sodium oxybate
New respectability for a notorious date-rape drug
Once banned by the FDA, sodium oxybate (Xyrem, Orphan Medical) is now the first drug to be approved for treatment of cataplexy in patients with narcolepsy. About 120,000 Americans suffer from narcolepsy. More than half of patients with narcolepsy also experience cataplexy, which is characterized by sudden loss of muscular control and muscle weakness or paralysis, usually triggered by strong emotions, such as laughter or anger.
Sodium oxybate, also known as gamma hydroxybutyrate, is a CNS depressant that's been used as a general anesthetic in some countries. Its mechanism of action as a treatment for cataplexy isn't understood.
In the United States, sodium oxybate was once available in over-the-counter products, purportedly to enhance athletic and sexual performance as well as to induce sleep. However, it was widely abused as a recreational and date-rape drug, prompting the FDA to take it off the shelves.
Considered to have a high abuse potential, sodium oxybate is available only from a single centralized pharmacy through a restricted distribution program. Because of concerns about respiratory depression and the drug's abuse potential, sodium oxybate has a black-box warning in the product labeling and is distributed with a patient medication guide.
Commonly reported CNS-related adverse reactions include dizziness, somnolence, asthenia, nervousness, confusion, sleepwalking, depression, abnormal dreams, and insomnia. Other problems reported with sodium oxybate use include headache, nausea and vomiting, pain, pharyngitis, infection, viral infection, flu syndrome, diarrhea, and urinary incontinence. Some patients have reported difficulty breathing and an increase in symptoms associated with sleep apnea, a problem for many patients with narcolepsy.
Because of the drug's sedative effects and rapid onset of action, a patient shouldn't drive or engage in other activities requiring alertness for at least 6 hours after taking the drug. Sodium oxybate is contraindicated in patients being treated with sedative-hypnotic drugs and shouldn't be used concurrently with other CNS depressants, including alcohol.
Sodium oxybate is catalyzed by succinic semialdehyde dehydrogenase, so it's contraindicated in patients with a deficiency of this enzyme. Use it cautiously in patients with heart failure, hypertension, or compromised renal function because the recommended daily dosage of sodium oxybate will result in a daily intake of 1 to 1.6 grams of sodium. The initial dosage should be reduced by half in patients with impaired hepatic function.
The recommended initial dosage is 4.5 grams/day divided into two equal doses of 2.25 grams. The dosage can be increased to a maximum of 9 grams/day in increments of 1.5 grams/day (0.75 grams/dose). An interval of 2 weeks should separate dosage increases to allow the prescriber to evaluate the patient's clinical response and to minimize adverse reactions.
Teach the patient these important points:
* Take both daily doses at bedtime, while in bed, because of the rapid onset of sedation. After taking each dose, remain in bed.
* Take the second dose 2 1/2 to 4 hours after the first dose. Set an alarm to awaken yourself for the second dose.
* Take the drug several hours after eating because food significantly reduces its bioavailability.
* Take the drug at about the same time each day in relation to eating.
Sodium oxybate is supplied through the Xyrem Success Program and distributed solely by Express Scripts Specialty Distribution Services. A prescriber initiates the program by contacting the pharmacy at 1-866-XYREM88.
* Common adverse reactions are italicized throughout this article.
SELECTED REFERENCES
Drug Facts, and Comparisons. St. Louis, Mo., Facts and Comparisons, Inc., 2003.
Nursing2003 Drug Handbook. Springhouse, Pa., Springhouse Corp., 2003.
Physicians' Desk Reference, 57th edition. Montvale, N.J., Medical Economics, 2003.
BY DANIEL A. HUSSAR, PHD
Remington Professor of Pharmacy
Philadelphia College of Pharmacy [middot] University of the Sciences in Philadelphia, Pa.
Copyright Springhouse Corporation Aug 2003
Provided by ProQuest Information and Learning Company. All rights Reserved