Vinorelbine tartrate (Navelbine [Burroughs Wellcome Research Triangle Park, NC; Pierre Fabre Medicament; Paris, France]) is used in the treatment of non-small cell lung cancer (NSCLC), breast cancer, and some gynecologic malignant neoplasms. The reported prevalence of adverse effects involving, the respiratory system is less than 5% and involves mostly dyspnea with occasional interstitial infiltrates. A patient with a hypercoagulable state and diffuse pulmonary NSCLC developed acute respiratory failure soon after vinorelbine infusion. Physicians should be aware of possible increased pulmonary toxicity of vinorelbine in patients with diffuse pulmonary NSCLC. (CHEST 1997; 112:846-48)
Key words: adult respiratory distress syndrome; hypercoagulable state; noncardiogenic pulmonary edema; non-small cell lung cancer; respiratory failure; thrombosis; vinorelbine
Abbreviation: INR = international normalized ratio; NSCLC = non-small cell lung cancer
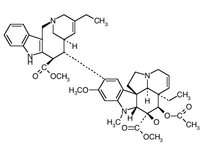
Vinorelbine tartrate is a semisynthetic Vinca alkaloid that has demonstrated activity in non-small cell lung cancer (NSCLC). Its dose-limiting toxicity usually is granulocytopenia, which is seen in almost two thirds of patients.[1] Its nonhematologic toxicities have been considered mild to moderate and easily manageable; in particular, it has less neurotoxicity than other Vinca alkaloids.[1,2] Studies in patients with NSCLC and breast cancer treated with vinorelbine have shown that dyspnea has occurred in fewer than 5% of cases, and when dyspnea has occurred, it has responded to bronchodilators or steroids when these needed to be used.[1,2] Unlike the other Vinca alkaloids, vindesine and vinblastine sulfate,[3-8] there have been no reports so far of major, life-threatening pulmonary toxicity with vinorelbine.
Herein is an unusual and interesting case of a patient with extensive pulmonary, spread of NSCLC who developed acute respiratory failure 3 days after his first infusion of vinorelbine. The lack of an autopsy means that the nature of the patient's respiratory failure is uncertain. Nevertheless, this is the first reported case in the literature of respiratory failure occurring soon after vinorelbine infusion in a patient with extensive NSCLC.
Case Report
A 70-year-old man presented to the hospital in December 1994 with swelling of the right leg after he was in a car for a 16-h trip. His past history. included left total hip replacement, type 2 diabetes, and peripheral vascular disease. One year prior to admission, he suffered an inferior myocardial infarction and underwent coronary artery bypass surgery and mitral valve replacement (Carbomedics model 700, 27 mm). There was no past history of deep venous thrombosis or malignant tumor. The patient was a previous cigarette smoker, used alcohol occasionally, and was taking various medications including warfarin sodium. Duplex ultrasonography revealed thrombosis of the distal right external iliac vein and of the distal left common femoral vein. Clot was also seen in the right thigh and calf.
Because the patient's international normalized ratio (INR) was therapeutic (2.7), an inferior vena cava filter was inserted via a jugular approach below the level of the renal veins. An arterial blood gas value with the patient breathing room air revealed a [PO.sub.2] value of 67 mm Hg and a [Pco.sub.2] level of 34 mm Hg. A chest radiograph was suggestive of a pulmonary infarct of the left lung base. Ventilation-perfusion lung scanning was not done. Results of blood tests were normal except for normocytic anemia (hemoglobin, 105 g/L), a creatinine value of 1.6 mg/dL (normal 0.4 to 1.5 mg/dL) (142 [Mu]mol/L, normal 40 to 130 ;[Mu]mol/L), and an IgG anticardiolipin titer of 27.3 (normal, [is less than] 23). An abdominal ultrasound test revealed a small cyst in the left kidney. The patient was discharged on a regimen of warfarin.
The patient was readmitted 2 weeks later with increased leg swelling and weight loss. Duplex ultrasound revealed extension of the thrombus up to the inferior vena cava filter. The INR was in the therapeutic range. Over 24 h, there was progressive ischemia of the right great toe. Recombinant tissue plasminogen activator was given intravenously (total, dose 100 mg over a period of 90 min) with some clinical improvement. Therapy with warfarin was discontinued, and the patient then began receiving maintenance therapy with intravenous and then subcutaneous heparin to keep the activated partial thromboplastin time between 50 and 70 s.
A chest radiograph revealed a nodule in the right upper lobe and small bilateral pleural effusions but no pulmonary edema (Fig 1). A CT scan revealed a 2.5-cm nodule in the posterior aspect of the upper lobe of the right lung; right paratracheal, pretracheal, and subcarinal lymphadenopathy; and small multiple nodules throughout both lungs. These findings were consistent with those of metastatic disease. A CT scan of the abdomen was normal except for a splenic infarct. Transthoracic needle aspiration of the pulmonary mass revealed moderately differentiated adenocarcinoma. The patient was given one dose of vinorelbine, 57 mg, intravenously (30 mg/[m.sup.2], 1.90 [m.sup.2]).
The patient complained of dyspnea 3 days later, and a physical examination revealed expiratory wheezing with no evidence of heart failure. He was treated with bronchodilators. With the patient breathing room air, arterial blood gas determination revealed a [PO.sub.2] of 64 mm Hg, a [Pco.sub.2] of 32 mm Hg, and a pH of 7.47. A chest radiograph showed new diffuse interstitial lung disease, and the patient was given intravenous furosemide. The next day, while receiving 50% oxygen, the patient's arterial blood gas determination revealed a [Po.sub.2] of 86 mm Hg, a [Pco.sub.2] of 30 mm Hg, and a pH of 7.54. A chest radiograph showed progression of the diffuse interstitial lung disease (Fig 2). An echocardiogram showed left atrial enlargement and mild tricuspid regurgitation with mild pulmonary hypertension. The ejection fraction, wall motion, and prosthetic valvular function were all normal. There was no pericardial effusion. Ventilation-perfusion lung scanning showed matching nonuniform uptake in both lungs; this finding was interpreted as suggestive of a low probability for pulmonary embolism. Serial cardiac enzyme levels were within normal limits, and sputum and blood cultures were negative for organisms. He was treated with aerosolized albuterol (Salbutamol) and ipratropium bromide, intravenously administered erythromycin, cefotaxime sodium, and furosemide.
On the following day, the chest radiograph had worsened (Fig 3), and he required increased amounts of oxygen to maintain a saturation level of 90%. He was given high-dose intravenous methylprednisolone sodium succinate (500 mg). Because of the extensive nature of his disease, the decision was made not to intubate him. He died that night, and the family refused autopsy.
Discussion
Of the 327 patients with breast cancer and NSCLC who were part of the North American clinical trials, vinorelbine use was associated with dyspnea in 5% of patients.[1] Two types of reactions were noted: an acute bronchospastic reaction which responded to bronchodilators and a subacute reaction with cough and dyspnea within 1 h of the infusion. Some of the patients with the latter reaction showed evidence of interstitial infiltrates on a chest radiograph and responded well to steroid treatment. In the subgroup of the North American patients with NSCLC, serial pulmonary function testing demonstrated no decrease in diffusing capacity during the trial.[1] Other trials to date make no mention of pulmonary toxicity, and there have been no reports of death from respiratory toxicity attributed directly to vinorelbine.
In this case, there was no evidence of massive pulmonary embolism or cardiac dysfunction. The patient reported herein was treated with broad-spectrum antibiotics, diuretics, bronchodilators, and finally corticosteroids. There has been a case report of ARDS occurring with heparin-associated thrombocytopenia,[9] but this patient's platelet count was both unchanged and normal. Although this patient showed no evidence of myocardial ischemia or infarction, there have been reports of myocardial ischemia after vinorelbine infusion.[10-12] The time course of this patient's respiratory failure does not fall into one of the two known patterns of vinorelbine reactions.
Studies of vinorelbine distribution in human lung tissue demonstrate that the concentration is higher and the disposition rate is slower in malignant compared with nonmalignant tissue.[13] Patients with diffusely metastatic lung cancer may be prone to lung injury as an increased volume of lung may be exposed to higher concentrations of vinorelbine. Patients with anatomically limited disease may be exposing a smaller volume of their "normal" lung tissue to higher concentrations of vinorelbine in the malignant tissue. The multiple nodules in the reported patient's lungs had become apparent during his illness, which does not support the presence of long-standing granulomatous lung disease or pneumoconiosis.
Although this patient's hypercoagulable state was not well characterized, it was a great source of morbidity and possibly mortality. Several reports have shown that patients with lung cancer may have thrombosis-inducing activity in their serum.[14] This Subgroup seems to be prone to the development of ARDS.[15]
Although definite conclusions cannot be drawn from this report, physicians should be cautious and aware when using vinorelbine and other Vinca alkaloids in patients with extensive NSCLC.
References
[1] Hohneker JA. A summary of vinorelbine (Navelbine) safety data from North American clinical trials. Semin Oncol 1994; 21(5 suppl 10):42-7
[2] Navelbine product insert. Research Triangle Park, NC: Burroughs Wellcome, 1994
[3] Israel RH, Olson JP. Pulmonary edema associated with intravenous vinblastine [letter]. JAMA 1978; 240:1585
[4] Rao SX, Ramaswamy G, Levin M, et al. Fatal acute respiratory failure after vinblastine-mitomycin therapy in lung carcinoma. Arch Intern Med 1985; 145:1905-07
[5] Lagler U, Gattiker HH. Akute Dyspnoe nach intravenoser gabe von vinblastin/mitomycin C. Schweiz Med Wschr 1989; 119:290-92
[6] Konits PH, Aisner J, Sutherland JC, et al. Possible pulmonary toxicity secondary to vinblastine. Cancer 1982; 50:2771-74
[7] Duedke D, McLaughlin TT, Daughaday C, et al. Mitomycin C and vindesine associated pulmonary toxicity with variable clinical expression. Cancer 1985; 55:542-45
[8] Kris MG, Pablo D, Gralla RJ, et al. Dyspnea following vinblastine or vindesine administration in patients receiving mitomycin plus vinca alkaloid combination therapy. Cancer Treat Rep 1984; 68:1029-31
[9] Asimacopoulos PJ, Athanasiadis I, McCarthy JJ, et al. Can heparin cause adult respiratory distress syndrome by a similar mechanism as heparin-associated thrombocytopenia? Chest 1994; 105:1266-68
[10] Bergeron A, Raffy O, Vannetzel JM. Myocardial ischemia and infraction associated with vinorelbine [letter]. J Clin Oncol 1995; 13:531-32
[11] Dubos C, Prevost JN, Brun J, et al. Infarctus myocardique et vinorelbine. Rev Mal Respir 1982; 8:299-300
[12] Nesme P, Trillet-Lenoir V, Brune J. Infarctus du myocarde induit par la vinorelbine? Cah Oncol 1993; 2:237-38
[13] Leveque D, Quoix E, Dumont P, et al. Pulmonary distribution of vinorelbine in patients with non-small-cell lung cancer. Cancer Chemother Pharmacol 1993; 33:176-78
[14] Maruyama M, Yagawa K, Hayashi S, et al. Presence of thrombosis-inducing activity in plasma from patients with lung cancer. Am Rev Respir Dis 1989; 140:778-81
[15] Ogino H, Hayashi S, Kawasaki M, et al. Association of thrombosis-inducing activity (TIA) with fatal hypercoagulable complications in patients with lung cancer. Chest 1994; 105:1683-86
COPYRIGHT 1997 American College of Chest Physicians
COPYRIGHT 2004 Gale Group