allergy update
HONE YOUR SKILLS FOR DIAGNOSING AND MANAGIN OCULAR ALLERGIES BY FOLLOWING THESE SIMPLE GUIDELINES.
Allergic conjunctivitis is one of the most frequently occuring ocular conditions that optometrists see. Consumers purchase roughly 40 million bottles of over-the-counter (OTC) anti-allergic eye dorps each year and another 4 million in prescription drops. Did you know that 90% of allergy patients self-diagnose and self-medicate their condition? This is unfortunate because we have vastly superior prescription medications to help these ptients better manage their condition.
The first step toward serving our allergy suffers better is to understand the pathology of the disease. I'll review this topic and discuss the clinical management of ocular allergies.
Pathogenesis of ocular allergy
When most people think of ocular allergies, they think of seasonal allergic conjunctivitis (SAC). Most patients suffering from SAC are usually bothered during the spring and early fall. A variant of this condition, called perennial allergic conjunctivitis (PAC), affects patients indoors and all year long. I'll discuss these two forms of ocular allergy in more detail later.
Two rarer and more severe forms of allergic conjunctivitis (atopic keratoconjunctivitis [AKC] and vernal keratoconjunctivitis [VKC]) also exist. But because the vast majority of what we typically see are SAC and PAC, I'll limit my discussion to these two forms.
Learning about SAC & PAC
The immunopathogenesis of SAC is a type-I hypersensitivity IgE-mediated reaction with the mast cell as the most important cellular player. The same is true for PAC and the progression of both conditions is as follows:
> The patient experiences sensitization to environmental allergens. He develops no symptoms, but the IgE molecule binds to receptors on sensitized mast cells and basophils in a way that prepares them for future allergen exposure.
> When future allergen contact happens, within seconds, degranulation of the mast cells occurs, leading to the release of a wide assortment of inflammatory mediators. The most important of these is histamine, but so are prostaglandins, leukotrienes and cytokines. This is the early phase of ocular allergies.
> The late phase begins hours after the initial activation and involves additional inflammatory cells. Eosinophils, neutrophils, basophils and T lymphocytes infiltrate the conjunctival mucosa. Recurrence and prolongation of symptoms are a result of a variety of mediators released by these additional inflammatory cells.
In the following sections, I'll discuss how to manage ocular allergies with different medications.
Reviewing OTC allergy drugs
OTC ocular allergy drugs such as Opcon-A, Visine-A and Naphcon-A contain an H1-receptor antihistamine (either antazoline or pheniramine) and a vasoconstrictor (either naphazoline or tetrahydrozaline). The antihistamine component competitively blocks the Hi receptors on the nocioceptive type-C nerves of the mucosal membranes.
The result is a significant decrease in ocular itching but little effect on ocular redness or swelling. The vasoconstrictor component works on the conjunctival blood vessels to decrease redness. The problem with these OTC drops are manifold:
> Many patients complain that their eyes sting, burn and tear upon instillation.
> OTC drops have a duration of action of two hours, but are recommended for use q.i.d. That only covers eight hours of relief.
> Chronic use of these drops often leads to tachyphylaxis, rebound conjunctivitis and a permanent loss of ocular vessel tone.
These problems are a main reason why we should use the following prescription anti-allergy drugs for our patients. The drugs listed in the following categories are more effective and carry less adverse effects.
Understanding antihistamines
Two common topical antihistamines are emedastine difumarate (Emadine) and levocabastine HCl (Livostin). These compounds are primarily Hl-receptor antagonists, which help relieve redness and itching.
Because their duration of action is three to four hours, patients must use them q.i.d. They have little impact on other proinflammatory mediators, such as prostaglandins and leukotrienes, so they have minimal effect on conjunctival swelling. They are best used for the mild allergy sufferer who doesn't respond to artificial tears.
Managing predictable attacks
Medications such as pemirolast potassium (Alamast), cromolyn sodium (Crolom), lodoxamide tromethamine (Alomide) and nedocromil sodium (Alocril) prevent mast cell degranulation by interfering with a critical calcium intake step that occurs after antigen-antibody binding. By interfering with the calcium intake, the medicine blocks the release of histamine and stalls the allergic process.
Mast cell stabilizers don't relieve existing symptoms of allergy; they prevent them from occurring. This works well in a patient who has a seasonal, predictable history of allergies where you see him several weeks before the anticipated onset of symptoms and start him on the drops prophylactically. They don't work well if a patient's allergy isn't limited to discrete, predictable attacks.
Combining benefits
Dual-acting compounds such as olopatadine HCI (Patanol), ketotifen fumarate (Zaditor) and azelastine HCl (Optivar) combine the quick response of antihistamines with the prolonged action of mast cell stabilizers. This is a considerable advantage over mast cell stabilizers that do nothing for the immediate needs of the allergy sufferer. It's also better than topical antihistamines, which do nothing for the delayed response of ocular allergies.
Of the drugs in this category, olopatadine has the broadest range of approvals while ketotifen has the longest duration of action - 12 hours. Although both olopatadine and azelastine are indicated for b.i.d. dosing, their duration of action is only eight hours.
Azelastine is described as a mast cell stabilizer as well as an antihistamine, but this statement hasn't been confirmed in human studies. In addition, olopatadine and ketotifen show a positive effect on rhinitis and sinusitis in combination allergy sufferers. It's proposed that this effect is caused by the draining of topical ocular anti-allergic medications through the nasolacrimal duct to the inferior turbinate of the nose. This is beneficial for patients who have watery eyes and runny noses.
Not-so-novel NSAIDs
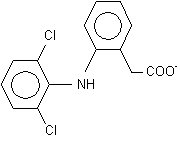
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ketorolac tromethamine (Acular) and diclofenac sodium (Voltaren) decrease the production of prostaglandins and thromboxane by inhibiting the cyclooxygenase pathway.
By inhibiting this pathway, NSAIDs help alleviate patient complaints of itchiness and conjunctival swelling with minimal effect on ocular redness.
The main problems with prescribing NSAIDs is that patients must take them q.i.d. (so compliance becomes an issue) and they can delay corneal wound healing. O.D.s rarely use NSAIDs to treat seasonal allergy anymore because of newer, more effective medications.
Topical corticosteroids
Steroids are often used for severe and chronic forms of allergy (such as VKC, AKC and allergic giant papillary conjunctivitis). Steroids act by blocking a vital enzyme in the arachidonic acid pathway of prostaglandin and leukotriene synthesis. Their clinical use in ocular allergies is usually limited to patients who don't respond to other treatments.
When prescribing this class (which includes loteprednol etabonate [Alrex], rimexolone [Vexol], fluorometholone [FML] and prednisolone acetate [PredForte]), prescribe the steroid first to decrease symptoms and then switch over to a combination mast cell stabilizer/antihistamine.
The safety and efficacy profile of loteprednol usually makes it the steroid of choice, although you can safely use the others for short time periods.
The skinny on oral meds
The more popular drugs include diphenhydramine HCI (Benadryl), fexofenadine HCI (Allegra), loratadine (Claritin) and cetirizine HCl (Zyrtec). Many patients think that the oral anti-allergy medications are stronger, but be forewarned. These drugs inhibit muscarinic receptors, leading to mucosal dryness. A dry eye with a defective tear film offers less protection against the allergens and pollutants.
Thus, oral antihistamines may actually exacerbate ocular allergies by lowering the defense offered by a healthy tear film. If your patient has complaints only dealing with his eyes and you have him on systemic medication, consider a change.
Scanning the future
The development of new agents is ongoing. A new formulation of olopatadine with a higher concentration to maximize efficacy and increased duration of action will be introduced in early 2003. Early studies indicate that this drug might be efficacious with oncedaily dosing.
For example, Allergan has presented clinical studies with its new histamine blocker, epinastine. EV131 (Evolutec, Ltd.), a novel histamine-binding protein with anti-inflammatory properties should enter clinical trials by the end of the year.
Research is ongoing for the development of leukotriene blockers, new generation prostaglandin blockers such as COX-2 inhibitors, adhesion molecule blockers and binding proteins. With our present selection of anti-allergy medicine, combined with those awaiting future release, we shouldn't have a hard time diagnosing and treating ocular allergies.
Our knowledge of available drugs, their benefits and their downfalls, will make our patients happier and they'll appreciate us more than they do the results they get from self medicating.
By DEEPAK GUPTA, O.D. Stamford, Conn.
Dr. Gupta has no financial interests in any of the companies or products mentioned in this arti
cle. You can reach him at deegup4919@hotmail.com.
Copyright Boucher Communications, Inc. Feb 2003
Provided by ProQuest Information and Learning Company. All rights Reserved