OBJECTIVE To identify and to describe the genotyping and the phenotyping testing practices of U.S. laboratories performing patient HIV-1 antiretroviral resistance testing.
DESIGN: A self-report 44-item mailed questionnaire.
PARTICIPANTS: Laboratories potentially performing HIV-1 antiretroviral resistance testing
MAIN OUTCOME MEASURE. Descriptive study.
RESULTS: Of 236 laboratories surveyed, 165 (69.9%) returned completed surveys, but only 23 performed HIV-1 antiretroviral resistance testing. Most were university hospitals (47.8%) or independent laboratories (26.1%). All 23 laboratories used genotypic methods, while nine (39.1%) used both genotyping and phenotyping. Most testing was used for clinical trials or laboratory research. The amount of patient information collected by laboratories varied, as did their type of quality assurance measures. Variation was found with regard to: testing volume, testing experience, testing reasons, testing methods availability, testing controls, specimen treatment, and storage stability.
CONCLUSIONS: Due to variation in practices in this area of patient testing, it may be advantageous for laboratory professionals to reach a consensus on what is the most acceptable.
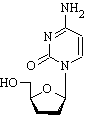
ABBREVIATIONS: 3TC = lamivudine; AZT = zidovudine; CDC = Centers for Disease Control and Prevention; CLIA = Clinical Laboratory Improvement Amendments; CT = clinical trials; d4T = stavudine; ddc = zalcitabine; ddl = didanosine; DLV = delavirdine; DT = drug treatment; ENVA = Evaluation of New Antiviral Treatments; HAART= highly active antiretroviral therapy; HIV = human immunodeficiency virus; LAP= Laboratory Assurance Program; LR = laboratory research; MPEP = Model Performance Evaluation Program; NVP = nevirapine; PT = patient treatment; QA = quality assurance; QC = quality control; VL = viral load.
INDEX TERMS: clinical laboratory techniques; drug resistance; HIV-1; quality control; viral RNA.
Clin Lab Sci 2002;15(4):213
In recent years, the development of antiretrovirals, including the use of monotherapy, and the discovery of the synergistic effects of antiretroviral drug combinations in reducing virus population, have impacted disease progression in those infected with human immunodeficiency virus (HIV). Along with these developments, tremendous strides have been made in our knowledge of the pathogenicity of HIV.1-- 4 Discovery of the massive amounts of virus production and huge viral turnover with high mutation rates offer tremendous challenges. One of these is to reduce viral replication and the subsequent mutation rates, estimated to be 3 x 10^sup -5^ mutations per nucleotide per replication, which would result in more effective antiretroviral therapy.5 As new agents are developed and current ones are increasingly used, it is vitally important to determine when they become ineffective in order to modify therapy. Antiretroviral resistance testing provides key information for monitoring treatment efficacy.
Highly active antiretroviral therapy (HAART) is currently considered the optimal treatment for HIV- 1 infection.6 The goal of this therapy is to minimize virus levels and suppress viral replication. For successful treatment using HAART, identifying the development of mutations that confer resistance is vital. As the HAART protocol becomes more common, as the number of infected individuals who meet the criteria to initiate antiretroviral therapy increases, and as the number of antiretroviral agents continues to expand, it is expected that laboratory testing for HIV-1 antiretroviral resistance will continue to increase.
Clinical laboratory practices in this area are extremely heterogeneous and lack standardization. To our knowledge, no large-scale, systematic study has occurred in the area of the phenotyping and genotyping methods or practices among laboratories performing HIV-1 antiretroviral resistance testing. Such a study is necessary in determining what measures might be taken to standardize methods and practices among laboratories in the U.S. so that patients and their physicians could obtain comparable results.
To this end, in 1999 the Laboratory Assurance Program (LAP) at San Diego State University in cooperation with the Division of Laboratory Systems, Public Health Practice Program Office, Centers for Disease Control and Prevention (CDC) undertook a survey to determine the number of laboratories performing antiretroviral resistance testing, and the methods they use.
METHODS
Survey Population
Names of laboratories potentially performing viral resistance testing came from many sources. These included: 1) CDC's Model Performance Evaluation Program (MPEP) list, containing HIV- 1 RNA testing laboratories that participate in CDC's MPEP; 2) Association for Molecular Pathology 1998 Test Directory; 3) laboratories participating in the Evaluation of New Antiviral Treatments (ENVA) conducted by Dr. Rob Schuurman of the University Hospital Utrecht, Utrecht, The Netherlands; 4) personal communication with experts in this area; 5) prior information from LAP surveys; and 6) flyers distributed at two national conferences (14th Annual Conference on Human Retrovirus Testing, Association of Public Health Laboratories, Albuquerque, NM, March 1999; Second Annual Conference on AIDS Research in California, San Francisco, CA, February 1999).7
The survey consisted of a 44-item, eight-page questionnaire, which queried laboratories about their HIV-1 antiretroviral resistance testing practices. Items were also included which described each laboratory. Both closed- and open-ended questions were used. The questionnaire was designed with help from experts in the field of antiretroviral resistance testing. The experts consisted of one MD and five PhDs who perform and conduct research in antiretroviral resistance testing, and who in some cases authored papers in this field in peer-reviewed journals. The experts received a draft of the survey questionnaire to critique and suggested changes either by mail or telephone. The final survey reflected their comments and suggestions.
Each survey packet mailed to participants included a cover letter, the questionnaire, a business reply envelope, and a brochure describing the MPEP provided by CDC. The survey was administered utilizing a three wave system. The first wave was mailed in July 1999. Nonresponders subsequently received the second wave in August 1999, and those still nonresponsive received the third wave in October 1999. The survey was closed in December 1999.
Data Management and Analysis
Graduate students in public health, using Paradox (Paradox for Windows, Version 5.0, Borland International, Inc. 1994) entered the questionnaire data into a database. When completed, a random sample of returned questionnaires was checked to ensure accuracy of data entry. The statistical package SPSS (SPSS for Windows, Version 8.0, Inc. 1997) was used for all data editing and analysis.
Frequencies were calculated for all variables, and stratification was carried out for certain variables to determine their impact on the distributions described. Data were stratified by laboratory type, testing methodology, CLIA certification, and purpose of testing. In some cases, stratification resulted in numbers too small to be meaningful.
RESULTS
Two hundred thirty-six laboratories were located that were identifed as likely to perform antiretroviral resistance testing. Of these, 165 (response rate, 69.9%) returned their survey. Included in the respondents were hospital laboratories (94, 57.0%), health department laboratories (29, 17.6%), independent laboratories (28, 17.0%) and an `other laboratories' category (12, 7.3%), which included university medical research (six), federal research (two), clinical diagnostic company (one), research (one), and two that did not further specify the 'other'. Most of the hospital laboratories were university based (40, 42.6%), privately owned (14, 14.9%), Department of Veterans Affairs (VA) (12, 12.8%) or community (8, 8.5%). Of the 29 health department laboratories, 15 (51.7%) were state, 7 (24.1%) were county, and 7 (24.1%) were 'other'. Of the 28 independent laboratories, 16 (57.1%) considered themselves to be reference laboratories.
Of the 165 responding laboratories, only 23 (13.9%) performed HIV antiretroviral resistance testing. This testing was done predominantly by university hospital laboratories (11, 47.8%) or independent laboratories who further described themselves as reference laboratories (6, 26.1 %). Of four testing laboratories that designated themselves in the 'other' category, three (75.0%) were further described as university medical school research laboratories, while one (25.0%) was self-described only as a research laboratory.
Among these 165 respondents, 63 (38.2%) did not perform HIV antiretroviral resistance testing, but did refer these tests to other laboratories, and the remaining 79 (47.9%) laboratories neither performed nor referred such tests.
The results discussed reflect the information obtained on those laboratories which did perform such testing. For example, of the 23 laboratories performing HIV- 1 antiretroviral resistance testing, 22 participants completed the survey by responding to a majority, but not necessarily all, of the questions. One laboratory, however, responded only to the questions on laboratory type, i.e., research and indicated their personnel performed genotyping and phenotyping. Thus the results reported here reflect a varying response denominator for each question. All testing laboratories (n = 23) indicated that they used genotypic methods, while nine (39.1%) also used phenotypic methods. Most laboratories performing only genotyping were located in a hospital setting (9/14, 64.3%), while more laboratories which performed both genotyping and phenotyping were research (4/9, 44.4%) and independent laboratories (3/9, 33.3%).
Twenty-one laboratories had been performing the testing for a median of 19 months (range, 1 to 96 months). When laboratories were stratified for genotyping-only versus genotyping-plus-phenotyping methodology, the median number of months of testing experience was 12 and 31, respectively. The median number of tests for 22 laboratories was 41 per month (range, 5 to 2000 tests). When stratified for genotyping-only versus genotyping-plus-phenotyping, those laboratories performing genotyping-plus-phenotyping had a median monthly patient resistance test volume of 80 when compared with a median of 35 for the genotyping-only laboratories. Seventeen (77.3%) of the 22 laboratories performed this testing as a component of clinical trials (CT), 18 (81.8%) for laboratory research (LR), and only 12 (54.5%) for patient treatment (PT). Of the 12 laboratories testing PT specimens, seven laboratories or 50% (7/14) of the genotyping-only laboratories and five laboratories or 62.5% of the genotyping-plus-phenotyping laboratories tested for this purpose (PT). None of the genotyping-plus-phenotyping laboratories and only one of the genotyping-only laboratories performed testing solely for patient treatment.
Additionally, ten (45.4%) laboratories performed testing for all three reasons (PT, CT, LR) and five (22.7%) for two reasons (CT, LR). The first group (PT, CT, LR) had a median number of months of experience of 23 months, the second (CT, LR), 30 months.
Specimen collection and treatment
Guidelines for specimen stability and shipping varied considerably (Table 1). Twenty laboratories provided instructions for specimen collection, while two did not. Eighty percent of the laboratories that recommended plasma for genotyping to be collected in ethylenediaminetetraacetic acid (EDTA), while 50% of the laboratories indicated that plasma could be collected in citric acid, trisodium citrate, dextrose solution (ACD). When the data were stratified by purpose for testing, 11 of 12 laboratories doing PT and 15 of 17 laboratories doing CT indicated they provided instructions for specimen collection. All 14 of the CLIA-certified laboratories provided instructions for specimen collection, and six of the seven non-CLIA-certified laboratories also provided these instructions. Two laboratories performing testing for both CT and LR and one laboratory doing testing for only PT indicated that they did not provide information about specimen stability.
Testing
Seventeen testing laboratories responded to a question on what patient information they requested. Of these, nine (52.9%) requested and collected information about the patient's HIV drug treatment history, 15 (88.2%) collected information about the patient's viral load history or previous results, and 8 (47.1 %) collected information about the patient's previous CD4+ results. Table 2 shows the responses for the purpose of testing (PT, CT, LR) and the type of patient information collected, i.e., HIV drug treatment history (DT), patient viral load history/previous results (VL), and CD4+ history/previous results (CD4+). Five of nine (55.6%) laboratories testing for all three purposes collected information on DT, eight of these nine (88.9%) on VL, and four of nine (44.4%) on CD4+. One laboratory performing this test for both PT and CT and one laboratory performing this test for both CT and LR, did not collect information on any of the three: DT, VL, or CD4+. One laboratory performing testing for only PT did not collect information on DT When stratified by genotyping-only versus genotyping-- plus-phenotyping, all (717, 100%) of responding genotyping-plus-- phenotyping laboratories collected information on VL, while 80% (8/10) of the genotyping-only laboratories collected this information. When considering collection of history on DT, 85.7% (6/7) of the genotyping-plus-phenotyping laboratories collected and 30% (3/10) of the genotyping-only laboratories collected such information. Only 30% (310) of the genotyping-only laboratories requested CD4+ information, while 71.4% (517) of the genotyping-plus-- phenotyping requested this information.
Only ten (45.5%) of 22 laboratories tested patient specimens for viral load prior to, or concurrently with, antiretroviral resistance testing. When stratified by testing method, 8 (57.1 %) of 14 of the genotyping-only laboratories and two (25.0%) of eight of the genotyping-plus-phenotyping laboratories tested for viral load prior to or concurrently with the antiretroviral resistance testing. Eighty percent indicated the reason for such testing was to determine if sufficient virus was present, 10% indicated it was a routine part of clinical care, and 10% indicated viral load would be performed if the patient had not had a viral load test within the last five months.
Respondent laboratories indicated which antiretroviral was used in their resistance testing procedures. All laboratories performing genotyping (n = 22) indicated resistance testing was performed for the nucleoside analogue reverse transcriptase inhibitors abacavir, didanosine (ddl), lamivudine (3TC), stavudine (d4T), zalcitabine (ddc), and zidovudine (AZT); for the non-nucleoside reverse transcriptase inhibitors efavirenz, delavirdine (DLV), and nevirapine (NVP); for the protease inhibitors indinavir, nelfinavir, retonavir, and saquinavir. On the other hand, of the phenotyping laboratories (n = 8), resistance testing was performed by 75% of the laboratories for 3TC, AZT, indinavir, and nelfinavir; by 62.5% of the laboratories for ddl, d4T, ddc, NVP, retonavir, and saquinavir; and by 50% of the laboratories for abacavir, efavirenz, and DIV. Investigational drugs, at the time of the survey, were amprenavir and adefovir for which 72.7% and 70.0%, respectively, were tested by the genotyping laboratories and 37.5% and 25.0%, respectively, were tested by phenotyping laboratories.
Ten laboratories indicated that they would be adding new drugs to their menu within the next six months. For those performing genotyping (15 responses), testing was offered per drug (6.7%), per panel (60.0%), or both (33.3%). For those performing phenotyping (seven responses), testing was offered per drug (57.1%), per panel (28.6%), or both (14.3%). The cost of genotypic testing for a single test ranged from $95 to $595 (median $398), and the cost for a panel ranged from $425 to $900 (median $450). Three laboratories, however, indicated they did not charge for a single test, and one laboratory did not charge for testing a panel of antiretrovirals. The cost for phenotypic testing for a single test (two responses) ranged from $250 to $400 (median $325), with an additional respondent performing the test at no charge, while for a panel (one response), the cost was $450.
Quality assurance
Of those performing genotyping testing, 20 (95.2%) out of 21 had a laboratory procedure manual with instructions for such testing, while only six (75.0%) out of eight of those performing phenotyping testing had such a manual. Of the 22 responding laboratories, 16 (72.7%) had criteria for rejecting samples. Table 3 displays the reasons for rejecting samples along with the number of laboratories ranking that criterion among the top three reasons for sample rejection. A specimen with too low a viral load, incorrect anticoagulant and specimen not at the appropriate shipping temperature were reasons most frequently mentioned for rejecting specimens. Respondents (n = 16) indicated that from zero to 200 specimens in a given month were rejected, with a median of three specimens.
Quality control practices
For those performing genotyping, quality control (QC) practices (n = 22), 20 (90.9%) included a negative control and 21 (95.5%) included a positive control. When laboratories were asked how frequently negative controls were run, responses included: daily; each run; with each set of seven samples; with new technologist training; weekly in every polymerase chain reaction (PCR) amplification; every run of 96; and with each batch of specimens. (It is unknown if the respondent considered a batch of samples to be a run.) Four laboratories used 'other' QC practices, indicated to be known proficiency test specimens; Pediatric AIDS Clinical Trial Group (PACTG); a patient sample; or samples run in parallel blinded with a second laboratory. Eleven (61.1 %) of 18 reported that their controls were non-kit controls.
For those performing phenotyping QC procedures (n = 6), five (83.3%) ran a negative control and three laboratories specified the frequency with every run, every seven samples, or every run of 96. Six (100%) used a positive control with every run, every run of 96, every sample, or each batch of samples tested. One specified 'other' QC practice which was patient sample run on a monthly basis. Five responded that their controls were non-kit controls.
Sources of QC materials for genotyping included commercial (n = 11), in-house (n = 12) or another laboratory (n = 3). For phenotyping QC, sources of materials were primarily in-house (n = 7), with one laboratory using another laboratory as a source.
During a one-month period, laboratories (n = 21) estimated the number of patient specimen tests that needed to be repeated to range from zero to 200, with a median of five. The laboratory estimating 200 repeats per month averaged 2000 patient specimens tested per month. Laboratories (n = 20) reported the primary reasons for repeat testing to be: failure to amplify genetic material (n = 8); poor sequence quality (n = 3); inadequate amplification (n = 3); reproducibility (n = 2); low viral load (n = 1); physician request (n = 1); part of research protocol (n = 1); human error (n = 1).
Eighteen of the laboratories responded to a question about having an established written protocol for performing quality assurance (QA) activities. Of these 18, 13 (72.2%) indicated that they had such a protocol. Ten (76.9%) of 13 CLIA-certifled laboratories and three (75%) of the non-CLIA-certified laboratories indicated they had such a written protocol. Over 77% of those performing testing for PT and over 84% performing testing for CT had such a protocol. VA hospital laboratories (n = 2) which, in one hospital, performed testing for PT and in the other, performed testing for LR, did not have a written protocol for QA activities.
Laboratories were asked if they would be willing to participate in a cost-free model performance evaluation program (MPEP) if it were available for HIV-1 antiretroviral resistance testing. Nineteen of 22 respondents (86.4%) indicated a willingness to participate in a laboratory QA program sponsored by CDC. Three (13.6%) indicated indecisiveness regarding participation at such a program. None declined participation.
All (n = 20) respondents believed testing for the antiretrovirals abacavir, 3TC, AZT, d4T, efavirenz, indinavir, nelfinavir, and saquinavir would be most valuable in a performance evaluation program. Ninety-five percent believed that ddl, ddc, DLV, NVR and retonavir should be included. Amprenavir and adefovir were considered by 75% and 65% respectively, to be of value in a performance evaluation program.
Respondents would like the methods incorporated in such a program to be: for both phenotyping and genotyping; genotyping by direct sequencing; genotyping (preferring that a panel is used with a cloned virus that has been qualified so that the contents are known); genotypes, especially defined mixtures similar to the ENVA panels; and phenotype-selected reference strains or blinded panels.
Personnel
Table 4 indicates most testing personnel (85.7%) are trained in-house by a supervisor, regardless of laboratory type, while supervisors are usually trained in-house by the manufacturer. Six (28.6%) of 21 respondents indicated that they had minimum time for personnel training, ranging from three weeks to six months. Supervisor training ranged from one month to two years (median time = 3.3 months). Those who supervised personnel in laboratories performing antiretroviral testing had been in this position from three months to 15 years (median time = 27 months).
Table 5 displays the responses regarding the types of questions physicians asked of laboratorians about testing and the number of respondents who ranked that question among the top three. More respondents indicated receiving questions about interpreting results (76.2%); collecting, transporting, or storing specimens (66.7%); or issues of cross-resistance (47.6%) than any other areas. Laboratory individuals responding to such questions by physicians had MD, PhD or both MD/PhD degrees and included laboratory directors, research directors, or infectious diseases physicians.
DISCUSSION
Given our resources and contacts, 23 laboratories were located which perform antiretroviral resistance testing. This testing is an integral part of patient management, and the questions of test availability and patient service become important issues. Even though access to testing may be a concern, the QA and standardization of this testing are clearly behind its utilization. Laboratory tests can only be relied upon when QA methods are in place. Our results showed that 95.2% of the laboratories performing genotyping testing had a procedure manual, while only 75.0% of those performing phenotyping had such a manual. This may reflect differences in facility types or purpose for testing. While most utilized positive and negative controls, the frequency of such use varied considerably, e.g., each run, weekly, or with newly trained technologist. Only 13 (72.2%) of 18 responding laboratories had an established written protocol for performing QA activities.
Laboratories varied also in their experience in performing this type of testing, from one month to 96 months for an average of five tests to 2000 tests per month. The average testing experience in laboratories is thus slightly more than two years. Laboratories performing few tests need more time to gain expertise with this testing. This falls into the category of complex testing and, given its nature, would warrant strict adherence to QA procedures.
The results of a laboratory test can be no better than the specimen collected. From this survey, 90.9% of the laboratories provide instructions regarding the manner by which specimens are collected; 81.8% specify guidelines on time limits for specimen stability, 77.3% for shipping conditions, and only 72.7% have criteria for rejecting samples.
The laboratory role is critical in assisting physicians on test requisition and interpretation of results. Our study indicates that physicians most frequently asked laboratorians about interpretation of results (76.2%). It is not clear whether this number reflects the method of reporting, i.e., ambiguity, the novelty of the testing, or both. For example, resistance testing is very difficult to perform if the viral load is less than 1000 copies/mL; yet only 88.2% collected information on the patient's viral load history (previous results) and only 45.5% performed this testing on each specimen prior to, or concurrently with, antiretroviral resistance testing.
Only 52.9% of the laboratories collected information about prior drug treatment, although these data are also pertinent to interpreting test results and selecting antiretrovirals to be used. Such testing represents information on the predominant circulating variants and may miss minor variants." The minor variants can predominate if inappropriate antiretrovirals are chosen.
Although the ordering of a laboratory test is frequently left to the discretion of the attending physician, it is the laboratory's role to provide advice to the physician regarding usefulness or appropriateness of such testing. Such an approach tends to increase the quality of health care service to the patient. The responding laboratories indicated that they provided inclusive panels of antiretrovirals for consideration by the physician. All (100%) of the listed antiretrovirals were included for those laboratories performing genotyping (Table 3). Approximately 70% provided test results for investigational drugs. This practice allows the physician a complete choice of drugs from which to select for treatment and eliminates delays that might occur due to the necessity for reordering or expanded testing.
The physician, and consequently the patient, can best be served by the laboratory's provision of high-quality, informative, and accurate test results. These study results demonstrate great heterogeneity among the kinds of laboratories that perform HIV-- I antiretroviral resistance testing, the kind of testing performed (genotyping-only or genotyping-plus-phenotyping), and the reason for testing, i.e., PT CT or LR. A wide variety of protocols and procedures appear to exist between laboratories. Sources of training, length of training, and purpose of testing were also inconsistent. QA and QC practices varied from laboratory to laboratory regarding adherence to existing requirement standards such as CLIA '88. In some settings, patient testing, which requires the strictest application of standards, may not be the focus of the laboratory's activities. A consensus of what laboratories should be doing in the arena of antiretroviral resistance testing is clearly needed. Because of the heterogeneity among laboratories, it may be difficult to achieve compliance to existing standards and to create consensus in areas where standards do not exist. On the other hand, having few laboratories performing this testing may facilitate the consensus process. The benefit of successful consensus building is that as more and more laboratories undertake HIV- 1 antiretroviral testing, they will have guidelines and standards to follow.
This study was funded by the Centers for Disease Control and Prevention through a cooperative agreement with the Association of Schools of Public Health.
The opinions expressed are those of the authors and do not necessarily reflect institutional policy.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
REFERENCES
1. Ho DD, Neumann AU, Perelson AS, and others. Rapid turnover of plasma virions and CD4+ lymphocytes in HIV-1 infection. Nature 1995;373:123-6.
2. Wei X, Ghosh SK, Taylor ME, and others. Viral dynamics in human immunodeficiency virus type I infection. Nature 1995;373:117-22.
3. Havlir DV, Richman DD. The role of viral dynamics in the pathogenesis of HIV disease and implications for antiretroviral therapy. Springer Seminars in Immunopathology 1997; 18:267-85.
4. Coffin JM. HIV population dynamics in vivo: implications for genetic variation, pathogenesis and therapy. Science 1995;267:483-9.
5. Mansky LM, Temin HM. Lower in vivo muta
tion rate of human immunodeficiency virus type 1 than that predicted from the fidelity of purified reverse transcriptase. J Virol 1995;69(8):5087-94.
6. Carpenter CC, Cooper DA, Fischl MA, and others. Antiretroviral therapy in adults: updated recommendations of the International AIDS Society - USA Panel. JAMA 2000;283:381-90.
7. Schuurman R, Demeter L, Reichelderfer P, and others. Worldwide evaluation of DNA sequencing approaches for identification of drug resistance mutations in the human immunodeficiency virus type 1 reverse transcriptase. J Clin Microbiol 1999;37(7):2291-6.
8. Hirsch MS, Conway B, D'Azuila RT, and others. For the International AIDS Society-USA Panel. Antiretroviral drug resistance testing in adults with HIV infection. JAMA 1998;279(24):1984-91.
Louise K Hofherr PhD is the Principal Investigator, Laboratory Assurance Program, Graduate School ofPublic Health, San Diego State University, San Diego CA.
Diane P Francis MPH is Program Administrator, Laboratory Assurance Program at San Diego State University, San Diego CA.
Rex Astles PhD is Senior Health Scientist at CDC, Atlanta GA.
Wiliam O Schalla MS is Senior Health Scientist at CDC, Atlanta GA.
Address for correspondence: Louise KHofherr PhD, Principal Investigator Laboratory Assurance Program, Graduate School of Public Health, 6330AIvarado Court, #208, San Diego, 92120. (619) 594-- 5006 (619) 594-8816 (fax). Ihofherr@mail.sdsu. edu
Copyright American Society for Clinical Laboratory Science Fall 2002
Provided by ProQuest Information and Learning Company. All rights Reserved