Guidelines for managing HIV and HCV co-infected patients.
As many as a third of HIV-infected individuals in the US are likely co-infected with hepatitis C virus (HCV). Recent guidelines are available online as part of a CME monograph at projectsinknowledge.com/programs.html. The report includes a discussion of clinical issues such as identifying patients requiring treatment, managing the challenges faced by co-infected patients, and optimally using highly active antiretroviral therapy (HAART) to treat HIV as well as interferon-alpha and ribavirin to treat HCV infection. Although many doctors still hesitate to treat HCV in HIV-infected patients, these guidelines emphasize the simultaneous use of combination therapies for HIV and HCV. Physicians are recommended to treat both viruses by staggering the initiation of treatments and carefully monitoring liver function.
Potential benefits of treating PHI.
Investigators from Massachusetts General Hospital and Harvard Medical School, in Boston, report that in HIV-infected patients successfully treated with HAART early in infection (i.e. during primary HIV infection, PHI) improved immune control is possible later on--even after discontinuation of therapy. Their study is published in the September 28 issue of Nature (407, p. 523, 2000). They measured HIV-specific cellular immune responses in patients who were effectively treated with HAART during the acute or early phases of HIV infection. When therapy was interrupted in 8 subjects, plasma viral load levels became detectable after 7 to 38 days. In 3 of these subjects, the viral load then dropped to less than 5000 copies/mL (varying from 500 to over 5000 copies/mL). Two were then able to stay off therapy after 7.4 and 8.7 months. The third elected to restart therapy after 91 days even though his viral load never exceeded 5000 copies/mL. After discontinuing therapy again, he has a viral load of 280 copies/mL at 5.4 months. The other 5 patients had to restart therapy, which was interrupted a second time. In all of these patients, viral load again peaked (but at a lower level than originally) and consequently fell to less than 5000 copies/mL without treatment. Two of these patients remained off therapy after 5.3 and 6.5 months, with viral loads less than 300 copies/mL. Virus-specific cytotoxic T cell responses increased significantly after both treatment interruptions and expanded to target more viral epitopes. Five of the 8 patients remained off therapy at the time of the report, an average of 2.7 years after initial infection. Viral loads remained below 500 copies/mL. The authors conclude that initiating HAART during acute or early HIV infection appears to confer a distinct benefit that may lead to periods of successful containment of viremia in the absence of HAART.
Perinatal guideline changes.
The Perinatal HIV Guidelines Working Group has updated the information in the Public Health Service Task Force Recommendations for the Use of Antiretroviral Drugs in Pregnant HIV-1 Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV-1 Transmission in the United States. The primary changes include the addition of a new section titled, "Perinatal HIV-1 Transmission and Mode of Delivery" (pages 23-32), and the addition of information about lopinavir/ritonavir (Kaletra) in Table 2. The guidelines are available online at hivatis.org/trtgdlns.html# Perinatal. Single copies can be requested by phone (800.448.0440).
Carotid lesion risk with protease inhibitors.
Add another cardiovascular disease risk to the list of those associated with HAART. Italian researchers have found that HIV-infected individuals treated with protease inhibitors appear to have a much greater risk of carotid vessel lesions than uninfected controls and HIV-infected patients who are not on protease inhibitors. The study, published in AIDS (14, p. F123, 2000), looked at 102 HIV-infected patients: 55 had taken protease inhibitors and 47 were protease inhibitor naive. These individuals and 104 uninfected controls underwent ultrasonography of their epiaortic vessels. Acquired lesions of the vascular wall were seen in 52.7% of protease inhibitor experienced patients, while naive patients had a significantly lower lesion rate of 14.9%. No plaques were noted in the control group. Correlations were noted between carotid lesions and age, male sex, smoking, high triglyceride and cholesterol levels, and disease stage. However, the factor that most influenced the risk of vessel disease was protease inhibitor use. Further studies are needed to determine the mechanisms involved, and the practical clinical significance of these results must still be determined.
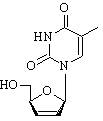
Trizivir approved.
On November 15, 2000, the US Food and Drug Administration (FDA) approved Glaxo Wellcome's application to market Trizivir. Trizivir combines zidovudine (Retrovir), lamivudine (Epivir) and abacavir (Ziagen) into one tablet. The 3 components of Trizivir, all nucleoside reverse transcriptase inhibitors, have been previously approved for use in the United States. Trizivir is dosed twice daily, with or without food. For antiretroviral naive patients with baseline viral loads less than 100,000 copies/mL, Trizivir alone could constitute a complete antiretroviral regimen. However, for patients with higher viral loads, clinical study data indicate that a Trizivir-only regimen is more likely to result in viral rebound than a regimen containing a protease inhibitor. Since Trizivir contains abacavir, patients who take the new combination pill should be advised to watch for symptoms of abacavir hypersensitivity, which include nausea, rash, fatigue, fever and respiratory symptoms.
Nevirapine (Viramune) safety warning.
In a November 2000 letter to healthcare providers, Roxane Laboratories warned of potentially fatal hepatotoxicity associated with nevirapine (Viramune) therapy. The company urges intensive clinical and laboratory monitoring of patients during the first 12 weeks of nevirapine therapy; however, one third of serious hepatic events occurred after 3 months of treatment. Patients with nevirapine-related hepatotoxicity may complain of fatigue, malaise, anorexia and nausea with or without elevated transaminase levels. Physical examination may reveal jaundice and hepatomegaly. A diagnosis of hepatotoxicity should be considered for patients who present with nonspecific symptoms of hepatitis, even if liver function tests are normal. If clinical hepatotoxicity occurs, nevirapine should be permanently discontinued. The company also reiterated the importance of the 14 day lead-in for nevirapine therapy, in which the drug is administered only once a day at 200 mg, as a measure for reducing the incidence of serious drug-related skin rashes. Clinical trial data indicate that prednisone actually increases both the incidence and severity of nevirapine-related rashes when used with nevirapine and should therefore not be used. This new safety information has been added to the nevirapine package insert, which is available at viramune.com.
Enteric coated didanosine (Videx) approved.
On October 31, 2000, the FDA approved Bristol-Myers Squibb's application to market enteric coated didanosine (Videx) capsules. Since this new formulation is licensed for once daily administration, the FDA intends it for patients "whose management requires once-daily administration" of didanosine or an alternative didanosine formulation. However, the agency cautions that twice daily dosing with buffered didanosine tablets is preferred because there are only limited data to support the durability of virologic suppression with the new once-daily capsules. As with the tablets, enteric coated didanosine must be taken on an empty stomach, defined as 1 hour before or 2 hours after food. Side effects most commonly associated with this new formulation include loose stools, mild diarrhea, nausea and abdominal discomfort; however, the drug was generally well tolerated by volunteers in clinical trial.
Methadone decreases absorption of didanosine, stavudine.
A study published last summer in the Journal of Acquired Immune Deficiency Syndromes (24, p. 241, 2000) indicates that the bioavailability of both didanosine and stavudine (Zerit) is decreased in HIV-infected patients on HAART who are also receiving methadone (Dolophine). Researchers from the University of Washington, Seattle, monitored serum levels of didanosine and stavudine in 17 patients who were on stable methadone therapy. In addition, they looked at absorption rates for didanosine and stavudine in 10 untreated individuals (as controls). Although there was a high degree of variability from patient to patient, methadone treatment on average reduced the areas under the curve by 63% for didanosine and by 25% for stavudine. In addition, peak drug concentrations were reduced by 66% for didanosine and 44% for stavudine. Levels of methadone appeared to be unaffected by either didanosine or stavudine. This study did not look at intracellular concentrations of the drugs, which is where didanosine and stavudine are active.
CD4 T cell response predicts clinical benefit.
Relying on data drawn from a prospective cohort study, French investigators report that the CD4 T cell response after 6 months of HAART predicts clinical outcome at 2 years regardless of virologic response. According to the investigators, the relationship between surrogate markers and clinical outcome among patients on HAART indicates that a CD4 T cell rise of at least 50 cells/[mm.sup.3] predicts a favorable clinical response at 24 months, even when virologic response is not optimal. Conversely, patients who have an optimal virologic response without the 50 cells/[mm.sup.3] increase have significantly higher rates of clinical disease progression. The researchers followed 2236 protease inhibitor naive patients for an average of 18 months.
COPYRIGHT 2000 The Center for AIDS: Hope & Remembrance Project
COPYRIGHT 2001 Gale Group