In looking to the future of salvage therapy, consideration must be given to what treatment strategies will work best, what the salvage population will look like, what types of patients will be available for trials of new drugs, and what resources will be available to provide the new drugs. Will multi-drug resistance (MDR) of the virus occur with the treatment regimens used today? How can research provide answers for how to circumvent MDR? These were the topics discussed in Panel 3, which focused on ways to define, monitor, and treat to current salvage population and the how the salvage population will prevail over time.
Doug Ward, MD, an HIV-treating physician, defined his salvage population as 2 groups: those who were treated with sequential monotherapy and are typically stable, and those who may be stable yet have MDR. Because of the availability of back-up regimens, Dr. Ward doesn't believe he is creating any new salvage patients today. Panelists noted that it is difficult to determine the actual extent of the salvage population. Are there new salvage patients or just treatment-experienced patients who are stable but have MDR regardless of CD4 T cell count? Also, why are there clinical differences between patients who have similar viral loads? One observation is that today's patients seem to be doing better with lower T cells, and changes in viral pathogenicity may be the reason. Because Dr. Ward's clinic is not representative of the larger HIV infected community, how can we define this population?
The HIV epidemic in the US itself has changed, affecting many more women and minority populations. In addition, the development (from nonadherence and other factors) and transmission of drug resistance are affecting the epidemic in regions where antiretroviral treatments are widely available, such as the US. To make matters worst', clinical trial enrollment is becoming more challenging, perhaps because of the wide availability of existing treatments or issues of distrust concerning the medical establishment. All of these issues make studying and treating the salvage population as challenging as ever.
Because health clinics may not be completely representative of the salvage population, one way to define the salvage population is to utilize databases from Virologic or other diagnostics companies. These databases contain information on the percentage of people carrying specific resistance patterns, though such databases lack medical history information. However, if the research community can accept the drawbacks, this type of database may be useful for quantitative analysis. Nevertheless, it still comes hack to defining the salvage population. Clinical cohorts such as Johns Hopkins, the HIV Out-Patient Study (HOPS), and the University of Alabama may provide some definition of the salvage population, though they may be collecting information on just treatment-experienced patients, therefore skewing their data collection toward patients with more resistance. Little prevalence data exist in nonacademic settings to help define a population of salvage patients. One cohort study is being developed. Other data from Mike Youle, an HIV-treating physician attending the Think Tank, also exist from his clinic.
The activist community has been attempting to solicit useful data from expanded access (EA) programs that may provide some information on the salvage population. Again, the caveat is that treatment history information is often not collected in these programs. Extensive sampling technique studies that collect population-representative information may be another way to characterize the salvage population. The Centers for AIDS Research (CFARs) have the CFAR Network of Integrated Clinical Systems (CNICS), which is a large system trying to link existing CFAR site databases electronically, but there are apparently logistical complexities with the linking of sites. While this system can define the population, there is no sampling and no information on medical history. However, there is a denominator of patients, their regimens, and levels of resistance. In any case, it may be the best way we have at this point to assess the salvage population.
Another question is how can we best predict treatment failure? There is concern that quality of life (QOL) assessments in determining treatment failure in the salvage population are not being adequately monitored and evaluated. Much attention has been placed on pharmacokinetics (PK) and efficacy; but is there a standard tool for QOL evaluations that could be adapted for use in clinical trials for drug development? The ACTG uses a QOL assessment tool that is accepted for many clinical trials.
In addition, guidelines on how to treat these patients are still unclear. Is "mega-HAART" (HAART that employs more than 3 drugs, and as many as 6 or 8 drugs, to treat HIV) still a useful strategy for salvage patients? Most panelists agreed there is little evidence to support it. However, if used today, mega-HAART would mean fewer pills since many drugs have been reformulated or coformulated. Have dual-boosted protease inhibitors (PIs) caught on for salvage therapy? An increase in pill burden and potential pharmacologic interactions may be reasons to not use dual-boosted PIs. What about enfuvirtide (Fuzeon or T-20) for those who are treatment experienced but fairly stable with relatively low viral loads and a CD4 T cell count above 200? Consideration must be given to save future options in this population and to avoid using novel therapies like T-20 too early, as it may be more useful in a deeper salvage setting. Intermittent therapy and regularly switching regimens may become promising approaches as more drugs are developed from new classes. Also, there may be utility in alternating Kaletra monotherapy in such a setting, given recent promising data. Further, would the use of an intermittent strategy be beneficial in patients who start therapy early and gain viral control?
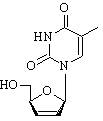
Newer drugs are selecting for different types of resistance, especially in nucleoside reverse transcriptase inhibitors (NRTIs), so that there may not be large numbers of thymidine analog mutations (TAMs) developing in patients who have started therapy in recent years. This changes the treatment paradigm and the expectations for new drugs. We know about "type 2" or "second generation" nucleosides, such as abacavir (Ziagen) or lamivudine (Epivir), which are distinguished by the 184 codon susceptibility. So, there needs to be newer compounds in the older thymidine analog nucleoside generation--drugs such as Retrovir (zidovudine or AZT) and Zerit (stavudine or d4T)--without the toxicities, which should be considered for any new drugs being developed. Some panel members questioned whether this would be applicable over time depending on growing mutation patterns and the variability of viruses with the 65 or 184 mutations. Other questions persist with newer drugs; for example, whether tenofovir (Viread) is clinically effective in those who are highly treatment experienced and for whom it is the only phenotypically susceptible NRTI.
Is there additional benefit for use of phenotypic testing in MDR patients? This type of testing may be useful depending on the patient. Phenotypic testing provides a benefit when there is some susceptibility to antiretroviral drugs. Questions still exist concerning cost effectiveness and where the use of phenotype and genotype tests is most practical. A replicative capacity (RC) assay is currently done with a commercially available phenotype test, and there is pressure to explore the idea of requiring a separate payment for RC tests. Obviously, the clinical utility of such a test should first be established through more studies in large numbers of patients.
One of the biggest salvage research questions today is where would the therapeutic drug monitoring (TDM) lest be most useful in the salvage paradigm? Such testing is used widely in Europe. The panelists agreed that TDM results are much simpler to read than those of a resistance test. If TDM is being used to choose drugs for patients with multi-PI resistance, then population-based information on PK and protein binding for the particular drug being tested should be considered. However, drug PK reports are not updated, especially in the current era of boosted PIs. Also, TDM cannot be used for nucleosides because of their intracellular activity (blood plasma levels may not accurately be a reflection of drug penetration and therapeutic activity). Therefore, the use of TDM will be best for determining therapeutic doses for individual patients or in patients with hepatitis co-infection to look for liver toxicities.
In summary, resource allocation and access to drugs will continue to be an issue for patients in salvage situations. One panel participant suggested that the problem was the overall structure of the healthcare system. At present, this is especially problematic for indigent patients who cannot access specialty care. Such situations actually create salvage patients. Recent studies have shown that adherence is actually improving in salvage patients, so treatment failure may get worse but resistance data may improve. Some consider it for worse to be highly resistant to a bad regimen than nonadherent to a good regimen. As far as treatment guidelines are concerned, the pendulum may swing in the direction of starting antiretrovirals earlier as regimens become easier to take and have less toxicity. Starting treatment early may be advantageous for several reasons. While no one is advocating that patients be on therapy for the rest of their lives, a brief period of early therapy may be beneficial. Some believe that patients are easier to treat overall if they start therapy earlier. With more research, time will tell if this is true.
Matt Sharp is a person living with AIDS and is Director of Treatment Education with Test Positive Aware Network in Chicago (tpan.com).
COPYRIGHT 2004 The Center for AIDS: Hope & Remembrance Project
COPYRIGHT 2004 Gale Group