Cardiovascular disease (CVD) is the nation's number-one killer and still claims more lives than any other major cause of death, including cancer, according to the American Heart Association's Heart Disease and Stroke Statistics - 2004 Update.1 [Cardiovascular diseases include high blood pressure, coronary heart disease (heart attack and angina), congestive heart failure, stroke, and congenital heart defects.] Smoking, obesity, hypercholesterolemia, type II diabetes and hypertension are leading contributors to development of coronary heart disease and stroke. Medications can be used to treat most precursor conditions for CX7D. However, many people are not treated or are undertreated, and control is dismal even among those being treated. For example, hypertension is a highly prevalent chronic disease, with one in four adults affected. Yet, only 59% of Americans with hypertension are currently being treated; and, of those, only 34% have an acceptable blood pressure.2 Similar statements could be made about control of cholesterol and diabetes. Some reasons for the lack of blood pressure, blood glucose and cholesterol control in the US population include that:
* High blood pressure and high cholesterol are relatively asymptomatic diseases until target organ damage has occurred.
* A combination of medications is often needed to control high blood pressure and blood glucose, especially in those with higher baseline levels.
* Levels of physical activity have decreased, and obesity has increased among the population.
* The cost of medication, especially for brand-name drugs, is high.
* Medications can have undesirable side effects, particularly at higher doses.
Better Control With Combination Therapy
Clinically, control of CVD is best achieved through a combination of blood pressure and/or other cardiac medications. Two recent review articles14 by Law and WaId in the British Medical Journal illustrate the advantages of using low-dose combination therapy for hypertension (three drugs) and cardiac disease prevention (six drugs). In the first article," the authors conducted a metaanalysis of well-designed (double-blind, randomized, controlled) clinical trials of thiazides, β-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARB) and calcium channel blockers, involving a total of 40,000 treated and 16,000 placebo patients. They found that all five categories of antihypertensive drugs produced similar reductions in blood pressure. The average reduction in systolic blood pressure was 9.1 mm Hg at standard dose and 7.1 mm Hg at half standard dose; and the average diastolic blood pressure reduction was 5.5 mm Hg at standard dose and 4.4 mm Hg at half standard dose, irrespective of the category of antihypertensive drug used. They also found that the blood pressure-lowering effects gained by combining different categories of antihypertensive drugs were additive.
Side effects were related strongly to dose in all categories except the ACE inhibitors (eg, cough). Side effects were less than additive when different categories of drugs were combined. Side effects at half standard doses were much lower than at standard dose among ARBs, β-blockers, calcium channel blockers and thiazides.' In conclusion, Law and WaId found that the combination of three blood-pressure drugs at half standard dose reduced average systolic pressure by 20 mm Hg and diastolic pressure by 11 mm Hg in patients with initial blood pressure > 150/90 mm Hg. They also estimated that this level of blood-pressure lowering would reduce the risk of stroke by 63% and of ischemie heart disease by 46% in 60- to 69-year-old hypertensive patients.
The second study4 by WaId and Law was conducted to determine the combination of drugs and vitamins needed to prevent CVD. Using data from meta-analyses and cohort studies, they devised a formulation designed to reduce the incidence of ischemie heart disease and strokes by reducing low-density lipoprotein, blood pressure, homocysteine and platelet function. They came up with a formulation of six drugs, including a statin, folic acid, low-dose aspirin and three blood-pressure drugs at half standard dose, which they called the "polypill." They estimated that the risk of ischemie heart disease could be reduced by 88% (CI, 84% to 91%) and stroke risk by 80% (CI, 71% to 87%) if everyone over the age of 55 took a "polypill." They estimated that 8% to 15% of those taking the "polypill" would have symptomatic side effects. While the idea of primary prevention in everyone over the age of 55 years is controversial, the use of multiple medications for primary treatment or secondary prevention of CVD is not. In the United Kingdom, the Department of Health is talking with Law and WaId about testing the "polypill" idea using fixed combinations of generic drugs.'
Back to the Future?
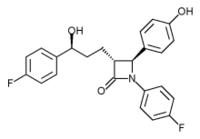
In the United States, the concept of combination therapy for cardiac disease has not gone unnoticed by drug manufacturers.'1 Most new branded antihypertensives are marketed as combination drugs with hydrochlorothiazide. Pfizer recently obtained approval from the US Food and Drug Administration to market a combination drug containing Norvasc and Lipitor. Merck has filed to obtain marketing approval for a combination of Zocor and Zetia. Bristol-Myers Squibb is developing a combination of aspirin and Pravachol. Problems with this approach are that available commercial preparations usually combine only two drugs, and that these preparations are in fixed dosage and tend to be very expensive.
A major part of the difficulty in achieving control of cardiac disease is the need for polydrug therapy. Most patients with high blood pressure (or another CVD) need at least three drugs to achieve good control and often are asked to take a cholesterol-lowering drug as well. Combine this with the need for medicines for other common symptomatic conditions, such as acid reflux, allergy, depression and osteoarthritis, and a relatively "healthy" adult could easily be taking five medicines per day. It is rational for patients to forego drugs that do not relieve any symptoms. This is a problem that could be cured by a compounding pharmacist.
Compounding pharmacists have an ideal opportunity to work with physicians to simplify drug-taking regimens by combining multiple cardiac drugs into a single capsule, thereby increasing treatment flexibility (not fixed doses), decreasing side effects (with lower doses) and most likely decreasing drug cost, ie, fewer co-pays, fewer drugs to buy. The benefits for compliance could be tremendous. Additionally, the compounding required is relatively simple, the chemicals are readily available, and capsule formulations are physically stable.
The Devil is in the Detail
Some operational issues need to be overcome to market "cardiac polycaps." Foremost among these is the need for massive re-education of primary care physicians and cardiologists, who for years have been taught to avoid fixed-combination drugs. Also, most internists and cardiologists are not aware of advances in the availability of compounding. Conversely, most compounding pharmacists do not have an extensive network of contacts among cardiologists. Cardiologist support is crucial for this type of compounding to succeed because internists will take guidance from cardiologists on the best formulations to use.
Additionally, there are the inevitable insurance issues and, since this is potentially a huge patient population, some accommodation with insurers should be worked out to obtain fair compensation. Insurers, eg, health plans and employers, probably would save money with increased use of generics and decreased cardiac events. On the other hand, increasing treatment among people who are noncompliant or undertreated could raise drug costs. A couple of well-designed outcomes studies are needed; perhaps this could be pursued directly with a health plan. Pharmacy benefit managers would have no incentive to approve compounded cardiac combination drugs because they would lose money through loss of rebates on the branded products and from loss of mail-service revenue.
Finally, there are clinical and pharmaceutical issues to resolve. What are the preferred formulations based on clinical trial evidence? What are the starting doses? How many of these drugs can fit into a number 1 or smaller capsule? What are the stability issues? Are there interactions with excipients? How can extended-release brand drugs be incorporated? Part 2 in this series will begin to address these questions.
References
1. [No author listed.] Heart Disease and Stroke Statistics - 2004 Update. Available at: www.americanheart.org. Accessed February 9, 2004.
2. [No author listed.] The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206-1252.
3. Law MR, WaId NJ, Morris JK et al. Value of low dose combination treatment with blood pressure lowering drugs: Analysis of 354 randomised trials. BMJ2003; 326(7404): 1427.
4. WaId NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80%. BMJ2003; 326(7404): 1419.
5. [No author listed.] Talks on marketing the polypill begin in UK. Medscape Cardiology2QQ3;7(2).
6. Tsao M. The biotech beat. Superpills with one-two punch. BusinessWeek Online2003. Available at: www.businessweek.com/technology/content/ oct2003Ac2003109_1337.htm. Accessed November 12, 2003.
Catherine A. Harrington, PharmD, PhD
Jacintha Cauffield, PharmD, BCPS
Nova Southeastern University
College of Phannacy
Palm Beach Gardens, Florida
Address correspondence to: Catherine A. Hinritigton, PharmD, PhD, Palm Beach Compounding Pharmacy, 155 TOIICY Pen mi Drive, Suite IB, Jupiter, FL 33-1-58. E-mail: catby@pahiibeachcoiHpotiiiding.com
Copyright International Journal of Pharmaceutical Compounding Mar/Apr 2005
Provided by ProQuest Information and Learning Company. All rights Reserved