SAN FRANCISCO -- Perinatal exposure to zidovudine was not associated with mitochondrial defects in early childhood in a review of more than 1,000 HIV-negative children enrolled in a U.S. study of HIV perinatal transmission.
Continued study is needed to confirm these results and ensure that the risk/benefit ratio of antiretroviral therapy for HIV-infected pregnant women "continues to fall on the benefit side," Dr. I. Celine Hanson said in presenting the results at the Seventh Conference on Retroviruses and Opportunistic Infections.
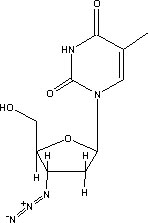
Zidovudine, a nucleoside reverse transcriptase inhibitor (NRTI), is widely used perinatally to reduce the risk of vertical HIV transmission.
Alarm bells that perinatal exposure to NRTIs carried an increased risk of mitochondrial toxicity in children were sounded at this meeting last year when French investigators reported two cases of severe, fatal mitochondrial neurologic disease in HIV-negative infants exposed to zidovudine plus the NRTI lamivudine.
The French investigators subsequently reported six nonfatal cases of mitochondrial toxicity related to perinatal exposure to zidovudine with and without lamivudine.
Since then, investigators reviewed the records of about 21,000 infants enrolled in U.S. perinatal HIV transmission databases. They found no link between antiretroviral therapy and death from mitochondrial dysfunction.
Dr. Hanson of Baylor College of Medicine in Houston and her associates looked for mitochondrial defects in living children involved in the Women and Infants Transmission study, a multicenter study of HIV-positive women and their infants.
The 1,189 HIV-negative children in the study were extensively evaluated at birth, at 1, 2, 4, 6, 9,12, and 18 months of age, and every6months thereafter.
Thirty-two percent of the children had no pre- or postnatal exposure to zidovudine; the rest of the children had at least some exposure to the agent, she said at the meeting sponsored by the Foundation for Retrovirology and Human Health.
During a mean follow-up of 30 months, 215 of the 1,189 children were identified for further investigation because of signs and symptoms possibly consistent with mitochondrial dysfunction. The most common conditions were growth abnormalities, developmental delay, neurologic findings, and oculomotor defects.
So far, 123 of these cases have been reviewed, with reviewers blinded to zidovudine exposure status. Fifty-eight of these 123 cases had no zidovudine exposure, Dr. Hanson said.
No child has been found to have proven mitochondrial defects. And none had signs and symptoms strongly suggestive of the defects--myopathy, cardiomyopathy, pancytopenia, retinitis pigmentosa, myocarditis, pericarditis, renal failure, or persistent metabolic acidosis.
Three patients had signs and symptoms that might include mitochondrial defects in the differential diagnosis. Two of these patients had had zidovudine exposure, and the other child had not been exposed.
Twenty-seven patients were classified as having limited signs and symptoms of a mitochondrial defect, but it was deemed unlikely. Thirteen of these patients had no zidovudine exposure, 13 had some exposure to the drug, and the exposure status was unknown in the other patient.
The reviewers found no evidence of mitochondrial defects in 92 patients--44 had had no zidovudine exposure, 46 had had zidovudine exposure, and the other 2 had an unknown exposure status.
Mitochondrial defect status was not assigned to 1 of the 123 children.
COPYRIGHT 2000 International Medical News Group
COPYRIGHT 2001 Gale Group