INTRODUCTION
Benzodiazepines are among the most commonly prescribed psychotherapeutic medications and are often used clinically to manage sleep disorders (1). Although they are clinically effective in the management of sleep disorders, benzodiazepines produce a myriad of side effects. Acute administrations of benzodiazepines, for example, have consistently been shown to dose-dependently impair various aspects of human performance including learning and recall (2-6). Chronic administrations of benzodiazepines produce tolerance and dependence (7,8).
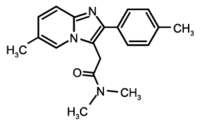
Novel compounds such as zolpidem (Ambien[R]) and zaleplon (Sonata[R]) that differ in their chemical profile are now available and may provide the desired soporific effects typical of benzodiazepines without the development of tolerance associated with chronic use (9). Zolpidem is the most commonly prescribed hypnotic (10). As with the benzodiazepines, zolpidem acts at the GAB[A.sub.A] receptor complex (11-13). However, the benzodiazepine receptor-binding profile of zolpidem is somewhat different from that of classic benzodiazepine agonists. Zolpidem binds with low affinity to [[alpha].sub.5]-containing GAB[A.sub.A]-receptor subtypes, whereas most available benzodiazepines bind with high affinity to these GAB[A.sub.A]-receptor subtypes (14).
Concordant with their biochemical differences, the results of studies with rodents suggest a dissociation between the tolerance-producing effects of classic benzodiazepines and zolpidem (15-19). In a recent study, for example, separate groups of rats received daily administrations of 12.5mg/kg lorazepam or 5.0mg/kg zolpidem for 12 days (16). Tolerance developed to the sedative, hypothermic, and muscle relaxant effects of the lorazepam, but only to the hypothermic effect of zolpidem. These results suggest that zolpidem and lorazepam, a classic benzodiazepine agonist, differ in terms of their tolerance-producing effects.
Data from studies with nonhuman primates involving zolpidem, by contrast, suggest zolpidem and classic benzodiazepine receptor agonists do not differ in their tolerance-producing effects (20). In this study, baboons received zolpidem (3.2 or 5.6mg/kg) for 8 consecutive days. The initial administration of zolpidem resulted in significant ataxia relative to vehicle. Zolpidem-induced ataxia decreased significantly over the next 7 days of treatment. These effects were similar to those produced by midazolam, a classic benzodiazepine agonist, under similar experimental conditions in the same laboratory (21).
The results of studies with humans are also mixed regarding the tolerance-producing effects of zolpidem and benzodiazepine agonists. Soldatos, Dikeos, and Whitehead (22) performed a meta-analysis on the effects of rapidly eliminated hypnotics such as triazolam and zolpidem. Data from a total of 75 studies and 1276 individuals revealed that tolerance to the effects of triazolam clearly developed after repeated administrations and that no tolerance to the effects of zolpidem developed.
There are data, however, that suggest tolerance can develop to the sleep-promoting effects of zolpidem under some conditions (23). In this study, patients (n = 99) with sleep difficulties received zolpidem (10 mg), triazolam (0.5 mg), or placebo for 28 consecutive nights. The sleep-producing effects of these drugs significantly decreased over the 28 consecutive administrations of both drugs relative to placebo, suggesting the development of tolerance to the sedative effects of both zolpidem and triazolam.
The purpose of this article is to assess the effects of repeated administrations of zolpidem and triazolam, a prototypical benzodiazepine, in humans. To accomplish this aim, 11 subjects received four doses of 15 mg zolpidem and two doses of placebo across 6 separate days. Fifteen subjects received 0.375 mg triazolam and placebo in an identical design. Drug effects were assessed with a battery of performance tasks and subject-rated drug-effect questionnaires that have previously been shown to be sensitive to the acute effects of zolpidem and triazolam [e.g., Refs. (24-27)]. Drug effects were assessed across the four administrations of each drug to determine if tolerance developed.
METHODS
Subjects
The volunteers in this study participated in two larger drug-discrimination studies conducted at the University of Mississippi Medical Center and the University of Kentucky Medical Center. Retrospective analyses have previously been used to reexamine data with a number of compounds (28-30). Eleven healthy adult volunteers (6 males and 5 females) were recruited via newspaper advertisements, flyers, and word of mouth to participate in the zolpidem component of this report at the University of Mississippi Medical Center. Four of the volunteers were Caucasian, one was Hispanic, and the remaining six were African American. Volunteers were paid $20 per session to participate in this experiment and also received performance-based payment stemming from correct responding on a drug-discrimination task. These volunteers ranged in age from 19 to 40 years (mean 27.7 years) and in weight from 134 to 190 pounds (mean 172 pounds). Two subjects reported smoking between 7.5 to 9 cigarettes (mean 8.3) and 1 cigar daily. Subjects who reported smoking tobacco cigarettes were permitted to do so freely except while completing the behavioral tasks.
Fifteen healthy adult volunteers (8 males and 7 females) were recruited to participate in the triazolam component of this report at the University of Kentucky Medical Center. Twelve of the volunteers were Caucasian, two were Hispanic, and one was Asian. The volunteers ranged in age from 18 to 35 years (mean 22.6 years) and in weight from 125 to 210 pounds (mean 161.6 pounds). Three subjects reported smoking 2 to 10 tobacco cigarettes daily (mean 6.5). Subjects who reported smoking tobacco cigarettes were permitted to do so halfway through each experimental session.
Before participating in the study, subjects completed questionnaires assessing drug use, medical and psychiatric histories, and provided written informed consent. Individuals with current or past histories of serious psychiatric disorder were excluded from the study. All subjects were in good health and had no contraindications to hypnotic medications. Drug urine screens conducted during screening were negative for amphetamine, benzodiazepines, barbiturates, cocaine, and opioids (Abuscreen ONTRAK, Roche Diagnostic Systems, Nutley, NJ). In female subjects, urine pregnancy tests before and during the study were negative. The Institutional Review Boards of the University of Mississippi Medical Center and of the University of Kentucky Medical Center approved these studies and the informed consent documents.
General Procedures
Data for this report were gathered during the first six sessions of the larger drug-discrimination study (27,31). These six sessions consisted of two sampling sessions and four test-of-acquisition days (two exposures to zolpidem or triazolam two exposures to placebo). On sampling days, volunteers received only doses of the active study medication (i.e., zolpidem or triazolam). During the test-of-acquisition sessions, the order of drug administration (zolpidem or triazolam and placebo) was randomized, but volunteers received two zolpidem or triazolam doses and two placebo doses during these sessions.
Subjects were informed that during their participation they could receive various drugs and that these could include placebo, various sedatives, muscle relaxants, and anxiolytics, stimulants and weight loss medications, antidepressants, and antihistamines. Subjects were told that the purpose of this study was to see if they could discriminate between various drugs, and how these drugs affect mood and behavior. Other than receiving this general information, subjects were blind to the type of drug administered and were given no information concerning expected outcomes of the study.
Before beginning the drug administration sessions, subjects completed at least 1 "practice" session to familiarize them with the behavioral tasks and the daily laboratory routine. No medications were administered on these days.
During the course of the study, subjects were instructed to abstain from using all psychoactive substances (barring tobacco and caffeinated products), alcohol for 12 hours before a scheduled session and caffeine and solid food for 4 hours before a scheduled session. On each experimental session day, subjects arrived at the laboratory at a prescheduled time. The time of sessions varied across subjects but was constant for individuals. After arriving at the laboratory, volunteers provided a urine sample that was screened on a random unannounced basis for the presence of amphetamine, barbiturates, benzodiazepines, cocaine, opioids, and THC. If a urine specimen was positive for compounds not administered experimentally, the session was canceled until the subject provided a drug-free urine. Subjects also provided an expired air specimen, which was assayed for the presence of alcohol using a hand-held Breathalyzer (Intoximeters, Inc., St. Louis, MO). All expired air specimens were negative.
On experimental session days, subjects completed the subject-rated drug effect questionnaires and performance task before drug administration. After drug administration, subjects completed the behavioral tasks periodically for 4 hours. A minimum of 24 hours separated all drug administrations. When not completing the experimental measures, subjects were allowed to engage in recreational activities or socialize with each other. Subjects were instructed not to discuss their drug effects with each other during the session or outside the laboratory.
Performance Measures
All performance tasks, except circular lights, were administered on an Apple Macintosh microcomputer. The tasks were completed in fixed order at approximately 0.5 hours before drug administration, and at 0.5, 1, 2, 3, and 4 hours after drug administration. These tasks were common to both of the larger drug-discrimination studies.
* Digit-Enter-and-Recall Task. The Digit-Enter-and-Recall task has been described previously [e.g., Refs. (24, 32)].
* Digit-Symbol-Substitution Test (DSST). A computerized version of the DSST, which has been described previously, was used in this experiment (33).
* Circular Lights Task. This task was completed using a Wayne Saccadic Eye Fixator (Wayne Electronics, Skokie, IL) and has been described previously (25).
Subject-Rated Drug-Effect Questionnaires
Subject-rated drug-effect questionnaires were administered on an Apple Macintosh microcomputer. The subject-rated drug-effect questionnaires were completed in a fixed order. The tasks were completed in fixed order at approximately 0.5 hours before drug administration and at 0.5, 1, 2, 3, and 4 hours after drug administration. These tasks were common to both of the larger drug-discrimination studies.
* Addiction Research Center Inventory (ARCI). The short form of the ARCI consisted of 49 true/false questions and has been described previously (34,35).
* Adjective Rating Scale. The adjective rating scale consisted of 32 items and contained two subscales: Sedative and Stimulant, which have been described previously (26).
* Drug-Effect Questionnaire. This questionnaire consisted of items that were presented on the monitor, one at a time. The items were: bad effects, good effects, high, like the drug, elated, carefree, relaxed, performance impaired, performance improved, take this drug again, and pay for this drug. These 11 items were common to the Drug-Effect Questionnaire in both studies.
Drug Administration
All drug conditions were administered in a double-blind fashion. Zolpidem (Ambien[R], Searle and Co., Chicago, IL) and triazolam (Halcion[R], Pharmacia and Upjohn Co., Kalamazoo, MI) doses were prepared by encapsulating commercially available capsules/tablets in a size 00 capsule. Each zolpidem capsule contained 5 mg zolpidem. Each triazolam capsule contained 0.125 mg triazolam. Lactose was used to fill the remainder of the all capsules. Placebo capsules contained only lactose.
During each experimental session, subjects orally ingested three capsules with approximately 150ml water. On each day of drug administration, subjects received 15 mg of zolpidem or 0.375 mg triazolam or placebo. Measures were taken to ensure that each subject swallowed all capsules and did not taste the contents. Specifically, the research assistant watched the subject swallow the capsules, conducted a brief oral examination, and spoke with the subject (36).
Data Analysis
Data were analyzed statistically as raw scores. For all statistical analyses, effects were considered significant for p [less than or equal to] 0.05.
Statistical analyses of data were conducted to determine the effect of acute administrations of zolpidem and triazolam, as well as the effects of repeated exposures to zolpidem and triazolam. Data were averaged across the two placebo administrations. Area-under-the-time-action-curve was calculated using the trapezoidal method, and analyzed with repeated measures one-factor analysis of variance with condition (Placebo, Exposure 1, Exposure 2, Exposure 3, and Exposure 4) as the factor. If there was a significant effect of condition, Fisher's protected least significant difference (PLSD) post hoc test was used to compare placebo to exposure 1 to determine the acute effects of zolpidem and triazolam. Exposure 1 and exposure 4 were then compared to determine the effects of repeated drug administration. Zolpidem and triazolam data were analyzed separately.
RESULTS
Zolpidem
Performance Measures
Zolpidem produced prototypical effects on the performance measures. Relative to placebo, the first administration of zolpidem significantly decreased the number of correct responses on the circular lights task, the number of trials correct on the Digit-Enter-and-Recall task, and the number of trials completed on the DSST. Zolpidem also significantly decreased the number of trials completed on the DSST. The magnitude of impairment following the fourth administration of zolpidem did not differ significantly from that observed following the first administration. Figure 1 shows these effects for 3 measures: number of responses on the circular lights task, number of trials correct on the Digit-Enter-and-Recall Task, and number of trials completed on the DSST.
[FIGURE 1 OMITTED]
Subject-Rated Drug-Effect Questionnaires
The first exposure of zolpidem also produced prototypical sedative-like on the subject-rated drug-effect questionnaires. Relative to placebo, the first administration of zolpidem significantly increased scores on the Sedative subscale of the Adjective Rating Scale, Pentobarbital, Chlorpromazine, Alcohol Group (PCAG) scores on the ARCI, and subject-ratings of bad effects, carefree, elated, good effects, high, like the drug, pay for this drug, performance impaired, relaxed, and take this drug again on the Drug-Effect Questionnaire. The first administration of zolpidem also significantly decreased scores on the Benzedine Group (BG) scale of the ARCI. Repeated administrations of zolpidem significantly decreased scores on the sedative subscale of the Adjective Rating Scale, and PCAG scale on the ARCI, as well as subject-ratings of bad effects, elated, good effects, high, and performance impaired, and relaxed on the Drug-Effect Questionnaire (Exposure 1 > Exposure 4). Figure 2 shows these effects for scores on the BG and PCAG scales of the ARCI, and subject-ratings of high and performance impaired from the Drug-Effect Questionnaire. Repeated administrations of zolpidem did not significantly decrease scores on any other subject-rated drug-effect-questionnaires.
[FIGURE 2 OMITTED]
Triazolam
Performance Measures
Triazolam produced prototypical effects on the performance measures. Relative to placebo, the first administration of triazolam significantly decreased the number of correct responses on the circular lights task and the number of trials correct on the Digit-Enter-and-Recall task and DSST, and the number of trials completed on the DSST. The magnitude of impairment after the fourth administration of triazolam was significantly lower than that observed following the first administration. Figure 3 shows these effects for three measures: number of responses on the circular lights task, number of trials correct on the Digit-Enter-and-Recall Task, and number of trials completed on the DSST.
[FIGURE 3 OMITTED]
Subject-Rated Drug-Effect Questionnaires
The first exposure of triazolam produced prototypical sedative-like subject-rated drug-effects. Relative to placebo, the first administration of triazolam significantly increased scores on the sedative subscale of the Adjective Rating Scale, scores on the PCAG scale of the ARCI, and subject-ratings of bad effects, carefree, good effects, high, like the drug, pay for this drug, performance impaired, performance improved, and take this drug again on the Drug-Effect Questionnaire. The first administration of triazolam also significantly decreased scores on the BG scale of the ARCI. Repeated administrations of triazolam significantly decreased subject-ratings of performance improved, relaxed, and take this drug again (Exposure 1 > Exposure 4). Repeated administration of triazolam did not significantly decrease scores on the other subject-rated items. Figure 4 shows these effects for the BG and PCAG scales of the ARCI, and subject-ratings of high and performance impaired.
[FIGURE 4 OMITTED]
DISCUSSION
In the present article, we have retrospectively examined the tolerance-producing effects of zolpidem, a novel imidazopyridine sedative, and triazolam, a classic benzodiazepine-receptor agonist. The results from the present investigation demonstrate that over four administrations, tolerance develops to some of zolpidem's subject-rated effects, but not to its performance-impairing effects. By contrast, over four administrations, tolerance developed to both the subject-rated and performance-impairing effects of triazolam.
The observation in the present report that tolerance developed to the performance-impairing effects of triazolam, but not to those of zolpidem is generally concordant with preclinical studies in rodents. The results of these studies suggest that tolerance does not develop to the effects of zolpidem (15-19). By contrast, tolerance to the effects of benzodiazepines like triazolam has consistently been observed in preclinical studies (15-19). The difference in tolerance-producing effects of zolpidem and triazolam may be due to zolpidem's binding specificity on the GAB[A.sub.A] receptor complex (12,14).
By contrast, the observation that tolerance did not develop to zolpidem's performance impairing effects is discordant with data from studies with nonhuman primates (20). As noted previously, in this study, baboons received zolpidem (3.2 or 5.6mg/kg) over 8 consecutive days. Over these administrations, the ataxia produced by zolpidem decreased significantly compared to the initial administration. The results of this study suggest that nonhuman primates become tolerant to the effects of zolpidem after a chronic regimen of administration. The reason for the discrepancy between the present study and this preclinical experiment is not known, but may be due to the use of different methods. Most notably, in the preclinical study, the baboons received doses of either 3.2 or 5.6 mg/kg zolpidem. These doses are much higher than those that can be administered to humans either clinically or experimentally. However, future studies with humans might test a higher dose than that used in this study (e.g. 20 mg).
The observation that tolerance developed to some of the subject-rated effects of zolpidem, however, is inconsistent with most previous clinical studies (17,22,37-43). Our findings that tolerance did not develop to the performance-impairing effects of zolpidem is consistent with most previous preclinical and clinical studies, and may indicate that performance measures, rather than subject-rated drug effect questionnaires, may be better suited for studying the pharmacological effects of sedative-hypnotics in humans.
The findings suggest that tolerance develops to the performance-impairing and subject-rated effects of triazolam following four administrations. Tolerance to classic benzodiazepines such as triazolam has been demonstrated under numerous laboratory settings at both the preclinical and clinical levels [for a review of these findings see Ref. (1)]. Tolerance to the subject-rated effects of triazolam observed in the present study is concordant with the results of sedative drug-discrimination studies in nonhumans. Drug discrimination in nonhumans is thought to be a model of subject-rated effects in humans (44). In one study, for example, rats were trained to discriminate midazolam (1 mg/kg) from pentylenetetrazole (20mg/kg) and from saline (45). After a chronic regimen of diazepam (20 mg/kg/8 hours for 7 days), tolerance and cross-tolerance developed to the discriminative-stimulus effects of midazolam.
Interestingly, with zolpidem, tolerance developed differentially between subjective estimates of performance impairment and objective assessments of performance. These diminished ratings of impairment associated with repeated zolpidem administration are concordant with previous studies regarding the impairment-producing effects of other hypnotics (46). In this experiment, human volunteers consistently underestimated their performance impairment after acute administrations of triazolam, but not pentobarbital, a barbiturate. The present findings extend these previous observations by demonstrating that tolerance develops differentially between subject-rated estimates of performance impairment and objective measures of performance. One implication of this observation is that patients chronically treated with zolpidem may become tolerant to its subject-rated effects (i.e., their ability to discriminate performance impairment), whereas their objective performance actually remains impaired. Thus prescribing physicians should perhaps instruct patients taking zolpidem that while they may not feel as if they are impaired after a few administrations, their actual ability to perform tasks may remain diminished. Future studies should examine the relationship between subject-rated and objective estimates of drug-induced impairment using other behavioral measures such as a driving simulator. These studies should administer the drugs both acutely and subchronically.
To our knowledge, this is the first report to compare the tolerance-producing effects of zolpidem and triazolam in humans under laboratory conditions. Although the results of the present study suggest differences between zolpidem and triazolam in terms of their tolerance-producing effects, they must be viewed with caution because of the methods used. Most notably, this report is retrospective in nature. The two experiments used in this report were not completed at the same location, and the differences could be due to subtle differences between the two samples. Future studies should prospectively compare the tolerance-producing effects of zolpidem and triazolam in humans. Further research should also examine the tolerance-producing effects of other novel sedative hypnotics like zaleplon. Finally, future studies that examine the tolerance-producing effects of these drugs should be conducted over a longer period (e.g., 2 weeks) to more closely approximate the use of these compounds in a naturalistic setting.
ACKNOWLEDGMENTS
This research was supported by the National Institute on Drug Abuse, Grant Number DA [09841] W.W.S. supported by the University of Kentucky Behavioral Science NIDA Predoctoral Traineeship (5-T32-DA07304-03).
REFERENCES
(1.) Hollister LE, Muller-Oerlinghausen B, Rickels K, Shader RI. Clinical uses of benzodiazepines. J Clin Psychopharmacol 1993; 23:1S-169S.
(2.) Cole SO. Effects of benzodiazepines on acquisition and performance: a critical assessment. Neurosci Biobehav Rev 1986; 10:265-272.
(3.) Curran HV. Benzodiazepines, memory and mood: a review. Psychopharmacology (Berl) 1991; 105:1-8.
(4.) Ghoneim MM, Mewaldt SP. Benzodiazepines and human memory: a review. Anesthesiology 1990; 72:926-938.
(5.) Lister RG. The amnestic action of benzodiazepines in man. Neurosci Biobehav Rev 1985; 9:87-94.
(6.) Roth T, Roehrs TA. A review of the safety profiles of benzodiazepine hypnotics. J Clin Psychiatry 1991; 52:38-41.
(7.) Woods JH, Katz JL, Winger G. Abuse liability of benzodiazepines. Pharmacol Rev 1987; 39:251-413.
(8.) Woods JH, Katz JL, Winger G. Benzodiazepines: use abuse, and consequences. Pharmacol Rev 1992; 44:151-347.
(9.) Chodera A, Nowakowska E, Bartczak G. Tolerance to a new class of non-benzodiazepine anxiolytics. Pol J Pharmacol 1994; 46:479-481.
(10.) Cardinale V. Drug Topics Redbook. Montvale, NJ: Medical Economics, 1996.
(11.) Haefely WE. Pharmacology of the benzodiazepine receptor. Eur Arch Psychiatr Neurol Sci 1989; 238:294-301.
(12.) Sanger DJ, Morel E, Perrault G. Comparison of the pharmacological profiles of the hypnotic drugs zaleplon and zolpidem. Eur J Pharmacol 1996; 313:35-42.
(13.) Sauvanet JP, Langer SZ, Morselli PL. Imidazopyridines in sleep disorders. New York: Raven Press, 1988.
(14.) Besnard F, Avenet P, Itier V, Granger P, Partiseti M, Depoortere H, Graham G, Langer SZ. GAB[A.sub.a] Receptor subtypes and the mechanism of action in zolpidem. In: Freeman H, Puech AJ, Roth T, eds. Zolpidem: An Update of Its Pharmacological Properties and Therapeutic Place in the Management of Insomnia. Paris: Elsevier, 1996:21-32.
(15.) Cox A, Boyland P, Gent JP, Feely M. An investigation of anticonvulsant tolerance to zolpidem I mice. Br J Pharmacol 1988; 95:667P.
(16.) Elliott EE, White JM. Precipitated and spontaneous withdrawal following administration of lorazepam but not zolpidem. Pharmacol Biochem Behav 2000; 66:361-369.
(17.) Perrault G, Morel E, Sanger DJ, Zivkovic B. Lack of tolerance and physical dependence upon repeated treatment with the novel hypnotic zolpidem. J Pharmacol Exp Ther 1992; 263:298-303.
(18.) Sanger DJ, Zivkovic B. Investigation of the development of tolerance to the actions of zolpidem and midazolam. Neuropharmacology 1987; 26:1513-1518.
(19.) Sanger DJ, Zivkovic B. Differential development of tolerance to the depressant effects of benzodiazepine and nonbenzodiazepine agonists at the omega (BZ) modulatory sites of GAB[A.sub.a] receptors. Neuropharmacology 1992; 31:693-700.
(20.) Griffiths RR, Sannerud CA, Ator NA, Brady JV. Zolpidem behavioral pharmacology in baboons: self-injection, discrimination, tolerance, and withdrawal. J Pharmacol Exp Ther 1992; 260:1199-1208.
(21.) Sannerud CA, Cook JM, Griffiths RR. Behavioral differentiation of benzodiazepine ligands after repeated administration in baboons. Eur J Pharmacol 1989; 167:333-343.
(22.) Soldatos CR, Dikeos DG, Whitehead A. Tolerance and rebound insomnia with rapidly eliminated hypnotics: a meta-analysis of sleep laboratory studies. Int Clin Psychopharmacol 1999; 14:287-303.
(23.) Ware JC, Walsh JK, Scharf MB, Roehrs T, Roth T, Vogel GW. Minimal rebound insomnia after treatment with 10mg zolpidem. Clin Neuropharmacol 1997; 20:116-125.
(24.) Evans SM, Funderburk FR, Griffiths RR. Zolpidem and triazolam in humans: behavioral and subjective effects and abuse liability. J Pharmacol Exp Ther 1990; 255:1246-1255.
(25.) Griffiths RR, Bigelow GE, Liebson I. Differential effects of diazepam and pentobarbital on mood and behavior. Arch Gen Psychiatry 1983; 40:865-873.
(26.) Oliveto AH, Bickel WK, Hughes JR, Shea PJ, Higgins ST, Fenwick JW. Caffeine drug discrimination in humans: acquisition, specifications, and correlation with self-reports. J Pharmacol Exp Ther 1992; 261:885-894.
(27.) Rush CR, Baker RW, Rowlett JK. Discriminative-stimulus effects of zolpidem, triazolam, pentobarbital, and caffeine in zolpidem-trained humans. Exp Clin Psychopharmacol 2000; 8:22-36.
(28.) Kollins SH, Rush CR. Sensitization to the cardiovascular but not subject-rated effects of oral cocaine in humans. Biol Psychiatry 2002; 51:143-150.
(29.) Singha AK, McCance-Katz EF, Petrakis I, Kosten TR, Oliveto A. Sex differences in self-reported and physiological response to oral cocaine and placebo in humans. Am J Drug Alcohol Abuse 2000; 26:643-657.
(30.) Zacny JP. Morphine responses in humans: a retrospective analysis of sex differences. Drug Alcohol Depend 2001; 63:23-28.
(31.) Rush CR, Kelly TH, Fillmore MT, Hays LR. Discriminative-stimulus and subject-rated effects of triazolam in light versus moderate drinkers: a dose-response analysis, Under Review.
(32.) Mumford GK, Rush CR, Griffiths RR. Abecarnil and alprazolam in humans: behavioral, subjective, and reinforcing effects. J Pharmacol Exp Ther 1995; 272:570-580.
(33.) McLeod DR, Griffiths RR, Bigelow GE, Yingling JE. An automated version of the digit symbol substitution test (DSST). Behav Res Methods Instrum 1982; 14:463-466.
(34.) Jasinski D. Assessment of the abuse potentiality of morphine like drugs (methods used in man). In: Martin WR, ed. Drug Addiction I. New York: Springer-Verlag, 1977:197-258.
(35.) Martin WR, Sloan JW, Sapira JD, Jasinski DR. Physiologic, subjective, and behavioral effects of amphetamine, methamphetamine, ephedrine, phenmetrazine, and methylphenidate in man. Clin Pharmacol Ther 1971; 12:245-258.
(36.) Abreu ME, Griffiths RR. Drug tasting may confound human drug discrimination studies. Psychopharmacol (Bed) 1996; 125:255-257.
(37.) Fairweather DB, Kerr JS, Hindmarch I. The effects of acute and repeated doses of zolpidem on subjective sleep, psychomotor performance and cognitive function in elderly volunteers. Eur J Clin Pharmacol 1992; 43:597-601.
(38.) Monti JM, Attali P, Monti D, Zipfel A, de la Giclais B, Morselli PL. Zolpidem and rebound insomnia--a double-blind, controlled polysomnographic study in chronic insomnia patients. Pharmacopsychiatry 1994; 27:166-175.
(39.) Poirrier R, Franck G, Scheldewaert R, Jolie A, Tomas M. The effect of long-term zolpidem treatment on nocturnal polysomnography and daytime vigilance in patients with psychophysiological insomnia. Acta Ther 1994; 20:77-86.
(40.) Roger M, Attali P, Coquelin JP. Multicenter, double-blind, controlled comparison of zolpidem and triazolam in elderly patients with insomnia. Clin Ther 1993; 15:127-136.
(41.) Scharf MB, Roth T, Vogel GW, Walsh JK. A multi-center, placebo-controlled study evaluating zolpidem in the treatment of chronic insomnia. J Clin Psychiatry 1994; 55:192-199.
(42.) Schlich D, Heritier CL, Coquelin JP, Attali P. Long-term treatment of insomnia with zolpidem: a multicentre general practitioner study of 107 patients. J Int Med Res 1991; 19:271-279.
(43.) Shaw SH, Curson H, Coquelin JP. A double-blind, comparative study of zolpidem and placebo in the treatment of insomnia in elderly psychiatric inpatients. Int J Med Res 1992; 20:150-161.
(44.) Schuster CR, Johanson CE. Relationship between the discriminative stimulus properties and subjective effects of drugs. In: Colpaert FC, Balster RL, eds. Transduction Mechanisms of Drug Stimuli. Berlin: Springer, 1988:161-175.
(45.) Pugh SL, Boone MS, Emmett-Oglesby MW. Tolerance, cross-tolerance, and withdrawal in rats made dependent on diazepam. J Pharmacol Exp Ther 1992; 262:751-758.
(46.) Roache JD, Griffiths RR. Comparison of triazolam and pentobarbital: performance impairment, subjective effects and abuse liability. J Pharmacol Exp Ther 1985; 234:120-133.
(#) Supported by NIDA Grant 09841.
William W. Stoops (1,2) and Craig R. Rush (1,2,3) *
(1) Department of Behavioral Science, (2) Department of Psychology, and (3) Department of Psychiatry, College of Medicine, University of Kentucky, Lexington, Kentucky, USA
* Correspondence: Craig R. Rush, Ph.D., Department of Behavioral Science, College of Medicine, College of Medicine Office Building (Rm. 127), University of Kentucky, Lexington, KY 40536-0086, USA; Fax: +1 (859) 323-5350; E-mail: crush2@uky.edu.
COPYRIGHT 2003 Marcel Dekker, Inc.
COPYRIGHT 2003 Gale Group