Clinical Question
Do antiviral medications prevent perinatal transmission of genital herpes to neonates?
Evidence-Based Answer
There is no evidence that the use of antiviral agents in women who are pregnant and have a history of genital herpes prevents perinatal transmission of herpes simplex virus (HSV) to neonates. [Strength of recommendation: A, based on multiple systematic reviews]
However, treatment with antivirals during the last month of pregnancy does reduce the rate of HSV outbreaks in pregnant women and the resultant need for cesarean delivery. [Strength of recommendation: A, based on multiple systematic reviews]
Evidence Summary
Neonatal herpes infection is the major consequence of maternal HSV. Fortunately, the transmission rate is quite low (less than 1 percent) for nonprimary HSV outbreaks. This poses a problem in assessing the effectiveness of antivirals for preventing this serious illness, because even a large meta-analysis is underpowered in addressing this issue.
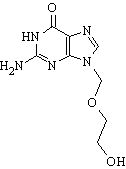
One systematic review and one meta-analysis reviewed a total of five randomized controlled trials. Both reviews were of good quality. The trials involved pregnant women with recurrent and first-episode HSV infections. In each study, women were randomized to either acyclovir (Zovirax) or placebo for HSV prophylaxis beginning at 36 weeks' gestation. The dosages of acyclovir ranged from 800 to 1,200 mg per day. Acyclovir was the only antiviral agent evaluated in either study.
The aggregate data involved nearly 800 patients. There were no reported cases of neonatal HSV infection in either the treatment or placebo groups. There was good evidence that prophylaxis with antiviral agents during the last month of pregnancy was effective in reducing the rate of HSV outbreaks during the perinatal period in mothers with HSV infections (15 of 424 in the acyclovir group versus 58 of 375 in the placebo group had HSV outbreaks during the perinatal period, absolute risk reduction [ARR] = 11%, number needed to treat [NNT] = 9). Presumably because of the significant reduction in HSV recurrences with antiviral prophylaxis, the total cesarean delivery rate was significantly lower in the treatment group (17 versus 26 percent, ARR = 9%, NNT = 11) as well as the rate of cesarean delivery for HSV recurrence (4 versus 15 percent, ARR = 11%, NNT = 9). Treatment also eliminated the risk of laboratory-detected HSV infection at delivery (0 versus 5 percent, ARR = 5%, NNT = 20).
Recommendations from Others
The 2001 National Guideline for the Management of Genital Herpes, published by the Association for Genitourinary Medicine and the Medical Society for the Study of Venereal Disease, recommends the use of continuous acyclovir during the last month of pregnancy as a treatment option in women with recurrent genital herpes. (4) The American College of Obstetricians and Gynecologists (ACOG) recommends that women with a first episode of HSV during any stage of pregnancy should be treated with a seven- to 14-day course of an antiviral agent. ACOG also notes that for women at risk of recurrent HSV, initiation gestation. The of antiviral therapy during the last month of pregnancy may be warranted.
Clinical Commentary
With the evidence that antiviral treatment reduces the rates of maternal HSV outbreaks in the perinatal period and subsequent cesarean deliveries, one could argue that maternal morbidity and costs are decreased with treatment. A cheap, safe medicine (acyclovir) and a small NNT of 93 add credence to this argument. Despite the lack of data regarding the outcome of neonatal HSV infection, the sample size required is so large that such a study may never be performed. Thus, acyclovir use for the prevention of perinatal HSV in the final month of pregnancy appears to be a reasonable treatment option
REFERENCES
(1.) Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51:1-78.
(2.) Jungmann E. Genital herpes. Clin Evid 2004;12:2212-27. Accessed online August 19, 2005, at: http://www.clinicalevidence.com/ceweb/conditions/seh/1603/1603.jsp.
(3.) Sheffield JS, Hollier LM, Hill JB, Stuart GS, Wendel GD. Acyclovir prophylaxis to prevent herpes simplex virus recurrence at delivery: a systematic review. Obstet Gynecol 2003;102:1396-403.
(4.) Clinical Effectiveness Group (Association for Genitourinary Medicine and the Medical Society for the Study of Venereal Disease). 2001 National guideline for the management of genital herpes. Accessed online August 19, 2005, at: http://www.bashh.org/guidelines/2002/hsv_0601.pdf.
(5.) ACOG Practice Bulletin. Management of herpes in pregnancy. Number 8, October 1999. Clinical management guidelines for obstetrician-gynecologists. Obstet Gynecol 1999;94:1-10.
CHRISTOPHER WENNER, M.D. St. Cloud Hospital/Mayo Family Medicine Residency Program St. Cloud, Minnesota
JOAN NASHELSKY, M.L.S. Managing Editor and Librarian Coordinator Family Physicians Inquiries Network Iowa City, Iowa
Author disclosure: Nothing to disclose.
Address correspondence by e-mail to Christopher Wenner, M.D., wennerc@centracare.com. Reprints are not available from the authors.
Copyright Family Physicians Inquiries Network. Used with permission.
Clinical Inquiries provides answers to questions submitted by practicing family physicians to the Family Physicians Inquiries Network (FPIN). Members of the network select questions based on their relevance to family medicine. Answers are drawn from an approved set of evidence-based resources and undergo peer review. The strength of recommendations and the level of evidence for individual studies are rated using criteria developed by the Evidence-Based Medicine Working Group (http:// www.cebm.net/levels_of_evidence.asp).
This series of Clinical Inquiries is coordinated for American Family Physician by John Epling, M.D., State University of New York Upstate Medical University, Syracuse, N.Y. The complete database of evidence-based questions and answers is copyrighted by FPIN. If you are interested in submitting questions to be answered or writing answers for this series, go to http://www. fpin.org or contact questions@fpin.org.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group