The specialized intense nursing care required during the immediate period of emergence from surgery and anesthesia resulted in the development of postanesthesia care units (PACUs). Recovery and discharge from the PACU require that, at a minimum, patients have adequate activity level, respiration, circulation, consciousness, and oxygen saturation. In some PACUs, these parameters are assessed by determining the Modified Aldrete Score (also known as the Postanesthesia Recovery Score) (1) (Table 1). Because of the need for continuity of care, patients' illness acuity, and cost containment, some critically ill patients bypass the normal recovery period in the PACU and go directly to an intensive care unit. To care safely for these patients during this crucial immediate postoperative period, critical care nurses must be familiar with the priorities for patients after both a surgical procedure and anesthesia. (2)
Anesthesia Techniques and Pharmacology
Anesthesia for surgery may be local, regional, or general. (3,4)
Local Anesthesia
Local anesthesia with lidocaine is commonly used in critical care for bronchoscopy, which typically is performed at the bedside. Many patients given local anesthetics also receive intravenous sedatives such as benzodiazepines to relieve anxiety. One of the main risks of local anesthesia is local toxic effects caused by accidental intravascular injection of the anesthetic or increased uptake of the agent from perivascular areas. Systemic toxic effects of local anesthetics are proportional to local anesthetic potency. The central nervous system is affected, and toxic effects are manifested as confusion, lethargy, and seizure activity.
Regional Anesthesia
Regional anesthesia includes spinal and epidural anesthesia and use of nerve-blocking agents. (5(p168)) Spinal anesthesia is achieved by injecting solutions of local anesthetics into the lumbar subarachnoid space. This type of anesthesia produces a profound sensory and motor anesthesia. Epidural anesthesia is achieved by injecting solutions of local anesthetics and/or narcotics into the epidural space, typically at the lumbar level. Advantages of epidural anesthesia include a lower occurrence of spinal headache and the option of providing postoperative analgesia that may benefit critically ill patients who are undergoing a surgical procedure such as a thoracotomy.
Risks of regional anesthesia are related to technique, such as accidental puncture of the dura or migration of anesthetic up to the thoracic level; migration of the epidural catheter; local direct trauma; or, to a lesser degree, compression of the nerves from edema and/or hematoma. Patients with regional anesthesia who continue to experience weakness, nerve pain, or paresthesia after the expected period of recovery should be examined by a physician for possible problems related to the anesthetic block.
Epidural catheters used intraoperatively may be left in place after surgery to provide postoperative pain control. Infusions and injections of dilute solutions of local anesthetics and special, preservative-free narcotics into the catheter are generally effective in pain control and have multiple beneficial physiological effects. The role of critical care nurses in managing these infusions may be limited by institutional policy and training requirements.
Another example of regional anesthesia is an axillary block of the nerves in the brachial plexus in the arm. Anesthesia is achieved by injecting a local anesthetic around the appropriate nerves supplying a given area of the body that requires anesthesia. Again, in this type of anesthesia, intravenous sedatives are often given along with the anesthetic.
Another example of regional anesthesia is a Bier block, a method of producing anesthesia of the arm or leg. A large volume (50 mL) of a solution of local anesthetics is injected while a tourniquet is applied to the extremity. Venous access is obtained at the distal part of the extremity, and the extremity is wrapped with an Esmarch bandage. (5(pp193-195)) The tourniquet is inflated to 2.5 times the patient's systolic blood pressure, and the anesthetics are injected. Patients may have discomfort at the tourniquet site if the surgical procedure lasts longer than 45 minutes.
General Anesthesia
During surgery, general anesthesia provides a combination of sedation, analgesia, amnesia, and muscle relaxation. (3) While maintaining patients' normal physiological status, anesthesia care providers administer a prescribed regimen of medications to achieve these goals. General anesthesia always requires airway control because the patient is unconscious. Knowing the sequence of necessary medications may help in understanding some of the potential postanesthetic complications related to general anesthesia. (6)
Inducing agents such as propofol are administered initially along with anxiolytics (eg, midazolam) (7) to depress the central nervous system and produce a hypnotic state in which patients become unconscious. Adverse effects of inducing agents include hypotension and vasodilatation, which can be more pronounced in patients with poor cardiac function. These effects should be short-lived because most of the medication should be metabolized before patients arrive in the PACU.
After the administration of the induction agents, opioids are typically administered. The most commonly administered opioids are fentanyl and morphine.
Neuromuscular blocking agents are administered next to aid with intubation, ease ventilation, and provide muscle relaxation that helps with exposure of the surgical field. These agents are divided into 2 groups: depolarizing and nondepolarizing. Depolarizing agents act at the postjunctional neuromuscular membrane to produce rapid skeletal muscle relaxation. Several undesirable effects are associated with depolarizing agents, such as massive hyperkalemia, malignant hyperthermia, anaphylaxis, and cardiac dysrhythmias. (8)
Succinylcholine is the only depolarizing agent used in the United States and is generally reserved for use in emergencies. It has a rapid onset (30-90 seconds) and a short duration of action (3-5 minutes) (9) and is usually administered for intubation. It noncompetitively inhibits the effects of acetylcholine at the neuromuscular junction and has no reversing agent. The muscle stays depolarized in a relaxed state, and no movement or contraction is possible.
Nondepolarizing agents compete with acetylcholine to impair muscle contractions and cause skeletal muscle relaxation. (10) They are longer acting than depolarizing agents and are used for intubation and to maintain muscular relaxation during surgery. They may also be used as paralytic agents in the intensive care unit to facilitate ventilatory control and to minimize metabolic demands. The choice of agent depends on the length of the procedure and the patient's medical conditions. The paralysis starts with the small fine muscles (fingers/eyes) and extends to the larger muscles of the limbs and trunk and finally to the intercostal muscles and the diaphragm. The effects of these blocking agents at the end of surgery are usually reversed by the administration of agents that allow the accumulation of acetylcholine at the neuromuscular junction.
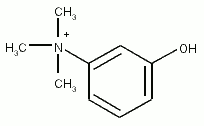
Three commonly administered reversal agents are neostigmine, edrophonium chloride, and pyridostigmine. All can cause undesirable effects by leading to the accumulation of synaptic acetylcholine in the heart, lungs, eyes, and gastrointestinal tract. An anticholinergic agent (atropine or glycopyrrolate) is always administered along with the reversal agent to prevent bradycardia, bronchospasm, and hypotension. Importantly, because the half-lives of the some neuromuscular blocking agents are longer than those of the reversal agents, patients may have signs and symptoms of voluntary muscle weakness during the early postanesthesia period. Neostigmine is more rapid and effective in completely reversing pancuronium or vecuronium than are other neuromuscular blocking agents with longer half-lives. (10) Muscle strength returns in the reverse order in which it was lost; the fingers and eyes are the last to regain strength.
The train-of-four procedure is used to assess patients' response to neuromuscular blockade and the adequacy of the reversal agent administered. When a peripheral nerve stimulator is placed on the ulnar nerve, patients should have 4 strong twitches equal in strength both visually and manually. Four equal responses or twitches indicate 0% to 70% neuromuscular blockade; no twitches indicate greater than 95% blockade. (11) Blockade is considered completely reversed when patients can maintain a 5-second hand grip, a 5-second head lift, and/or a 5-second tongue protrusion. Patients cannot perform these movements if the receptors at the neuromuscular junction are still one third occupied by a muscle relaxant. If only partial reversal occurs, another dose of reversal agents can be administered. Other parameters that should be assessed before extubation include the ability to take a deep breath, respirations greater than 12/min, inspiratory force greater than -25 cm [H.sub.2]O, tidal volume 5 mL/kg, and vital capacity greater than 15 mL/kg.
Finally, inhaled anesthetic agents, such as isoflurane and sevoflurane, and opioids, such as fentanyl, maintain general anesthesia. The exact mechanism of action for inhalation agents is unknown, but all depress the central nervous system, placing patients into a deep state of unconsciousness sufficient to allow surgery. The choice of inhalation agent varies, depending on patients' medical history. These agents are usually administered through airway devices such as an endotracheal tube or a laryngeal mask airway. Isoflurane and sevoflurane are the most widely used agents. Desflurane can cause airway irritation and should not be used in children or in patients with a history of smoking. (5(pp114-118))
Inhalation agents can cause cardiac depression, hypotension, vasodilatation, and arrhythmias. Cerebral vasodilatation can increase intracranial pressure. Opioids such as fentanyl reduce pain during and after emergence from general anesthesia and may produce lingering marked respiratory depression.
Postanesthesia Care
For most patients, recovery from anesthesia and surgery is smooth and uneventful without complications. However, for some patients, recovery can be accompanied by life-threatening complications that require prompt intervention. As with any resuscitation, initial postanesthesia care should be managed in terms of the familiar ABCs: airway, breathing, and circulation. (12) Nurses must also know which physicians are responsible for which patients and who is to be called for possible problems during this period of postanesthetic care. The appropriate physician may be an anesthesiologist, a surgeon, or an intensivist.
Airway Obstruction
Postoperatively, patients may arrive in a critical care unit either intubated or extubated. Patients may bypass the PACU because of anticipated prolonged intubation, potential for physiological instability, and/or sedation that requires ongoing monitoring in a critical care setting. All patients should have continuous pulse oximetry. (13) Extubated patients may have airway obstruction because the tongue falls backward and obstructs the posterior part of the pharynx. (11) Signs of obstruction include snoring, nasal flaring, sternal retractions, and use of accessory muscles. Often these patients are too sedated to maintain a patent airway or may be partially paralyzed.
Treatment starts with oxygen and stimulation to encourage patients to take deep breaths. Further assessment may indicate the need for a chin lift/jaw thrust or use of an oral or a nasal airway; if neither of these is successful, reintubation with an artificial airway may be required. Reintubation may be necessary until a patient is more alert or additional reversal agents such as naloxlone or neostigmine are administered. In heavily sedated patients, an oral airway is better tolerated than is a nasopharyngeal airway. In more alert patients, a nasopharyngeal airway may reestablish airway patency while avoiding gagging or vomiting. Nasopharyngeal airways (sometimes called nasal trumpets) are better tolerated than are oral airways in semiconscious patients. As the name implies, a nasopharyngeal airway is inserted through the nose, so it cannot be used for patients who have just had nasal surgery. Its use is associated with nasal bleeding, and it must be inserted carefully with lubrication, especially in patients who have known bleeding disorders or who are taking anticoagulants.
Another cause of airway obstruction in extubated patients is laryngospasm, a partial or complete spasm of the vocal cords that usually occurs soon after extubation. (14) Patients at risk for this complication include those with a history of smoking; difficult intubation, possibly with direct trauma to the vocal cords; chronic obstructive pulmonary disease; and vocal cord surgery. (14) Signs of laryngospasm include agitation, stridor, hypoxia, crowing (partial obstruction), and a total lack of breath sounds (complete obstruction).
During this airway emergency, positive-pressure ventilation should be immediately applied via an oxygen resuscitation bag or mask, other causes of airway obstruction should be alleviated, and assistance should be summoned. Critical care nurses should be prepared to assist in emergency airway management and reintubation at all times. Suctioning, oxygen, and positive-pressure ventilation should be readily accessible. A subparalytic dose (1.5 mg/kg) of succinylcholine should be administered if reintubation is necessary. Careful assessment of patients' readiness to be extubated should be determined before extubation, because an irritable airway can make reintubation difficult.
Noncardiogenic pulmonary edema is an uncommon complication associated with laryngospasm. (14) When laryngospasm occurs, patients exert a strong negative inspiratory force that may damage the epithelial layer of the lungs. This damage causes fluid to leak into the lungs and is manifested as pink frothy sputum and pulmonary edema.
Intubated patients with airway obstruction have a different set of potential airway problems. In an intubated patient, the endotracheal tube may be occluded because it is plugged by mucus or blood, because it is kinked, or because the patient is biting it. During transportation from the operating room to the critical care unit, the endotracheal tube may have become dislodged from the correct position in the trachea into the pharynx or may have migrated downward into one of the main stem bronchi. In order to help evaluate endotracheal tube placement and problems such as pulmonary collapse or pneumothorax, every postoperative patient who is to remain intubated should be assessed immediately upon arrival and as needed thereafter for the presence of breath sounds. Patients who require a postoperative chest radiograph should have the radiograph interpreted promptly by a physician.
Breathing Complications
Once the airway is considered patent, ventilation is assessed. An intubated or nonintubated patient may have signs and symptoms associated with respiratory problems such as hypoventilation (increased PaC[O.sub.2]) and hypoxemia (decreased Pa[O.sub.2]) (Table 2). Certainly, ongoing sedation, incomplete reversal of neuromuscular blockade, and pain are risk factors for poor ventilation. The degree of sedation should be assessed continually by observing such factors as patients' spontaneous awakening, maintenance of airway when not stimulated, and the ability to follow simple commands such as "take a deep breath."
Incomplete reversal of neuromuscular blockade can be diagnosed as generalized weakness, such as the inability to lift the head from the bed. Also, rocking-boat respirations (the chest collapses and the abdomen protrudes as the diaphragm descends with inspiration) can indicate intercostal muscle weakness due to partial neuromuscular blockade. (6) Patients recovering from major abdominal or thoracic surgery may experience pain that limits their use of abdominal and chest musculature.
Breath sounds should be assessed for iatrogenic pneumothorax, which can occur after a placement of a central venous catheter, operative injury to the pleura such as during a nephrectomy, or barotrauma associated with positive ventilation used during general anesthesia. Also, chest tubes placed during the surgical procedure should be draining correctly and be free of air leaks. Mucus plugs in the bronchus and associated pulmonary collapse can be a problem, especially for patients maintained in a lateral decubitus position during surgery.
Circulatory Complications
Cardiogenic pulmonary edema can occur and may be caused by overzealous fluid or blood resuscitation during surgery, particularly in patients with a history of congestive heart failure or left ventricular dysfunction. Operative or early postoperative myocardial infarction may be manifested as pulmonary edema. Postoperative hypotension has many diverse causes (15) (Table 3). Some may be obvious, such as a blood-soaked wound dressing suggesting ongoing bleeding. Many of the causes are readily recognized.
Postoperative hypertension is common in patients who are preoperatively hypertensive. Patients with pain, anxiety, a full bladder, and/or confusion may have hypertension. Sedation and adequate pain control may be all that is needed. Hypercapnia, hypoxemia, and volume overload are other common causes. Management of refractory hypertension usually requires an intravenous bolus or a continuous infusion of an antihypertensive medication.
Management of Monitoring Catheters
Means of intravenous access must be patent and must be properly secured because of the need to administer medications and fluids. Central venous and arterial catheters may become unsecured or dislodged during transportation and should be adjusted in the critical care unit. Arterial catheters used for monitoring must be recalibrated, and blood pressure values obtained via the catheters must be correlated with values obtained by using a blood pressure cuff. If not previously obtained, a chest radiograph is needed to verify the position of intraoperatively placed central venous catheters; function of the catheters can be confirmed by the presence of venous blood return. Central venous pressures should be measured in any hypotensive patient who has a central venous catheter in place.
Postanesthetic Conditions Hypothermia
Up to 60% of postoperative patients experience some degree of hypothermia, defined as a core temperature less than 36[degrees]C. (16) Hypothermia can cause cardiac arrhythmias and dysfunction, hypotension, and coagulopathy. Many factors contribute to postanesthetic hypothermia. (17) Hypothermia is common in the elderly and in infants. Anesthetic agents can alter the ability of the hypothalamus to regulate body temperature. Muscle-relaxing agents prevent shivering. Patients may lose heat after anesthesia of long duration (>1 hour) and with major open chest and abdominal operations associated with large amounts of fluid and/or blood replacement.
Traditionally, patients are wrapped in warm cotton blankets that do not increase the core body temperature. The most effective intervention is the use of a forced-air convection warming system. (17) Other rewarming methods include injection of warm intravenous fluids or blood, increased room temperature, and, in intubated patients, warmed air via the ventilator.
Shivering
Shivering can be a sign of hypothermia or an adverse effect of inhalation agents and occurs in 5% to 10% of postoperative patients. Muscles of the trunk and extremities are often involved, but shivering may be more obvious in the jaw and shoulders. (16) Shivering is especially detrimental to patients with cardiac disease because it increases cardiac oxygen consumption and the metabolic rate by 400% to 500%. Shivering can be controlled by warming patients and/or giving intravenous meperidine. Caution is required in the dosing and frequency of administration of meperidine in the immediate postoperative period while anesthetics are still present in the body and in newly extubated patients.
Malignant Hyperthermia
Malignant hyperthermia is a rare genetic disorder that is triggered by anesthetic agents, including succinylcholine, isoflurane, halothane, sevoflurane, and desflurane. It is due to the release of intracellular calcium that causes total-body sustained muscle contractions. These contractions generate heat and can excessively raise body temperature to more than 40[degrees]C. Early warning signs include jaw contracture followed by increasing end-tidal carbon dioxide and tachycardia. The best practice is to detect this potential problem preoperatively by obtaining a good history, soliciting information such as unexplained intraoperative deaths in family members, a history of adverse events associated with anesthesia, and central core neurological diseases (eg, muscular dystrophy). (18) Typically, malignant hyperthermia is detected in the operating room while the patient is anesthetized, and PACU nurses often must manage this condition. (19) If malignant hyperthermia is suspected, the anesthesiologist stops administering the offending anesthetic agents, initiates hyperventilation with 100% oxygen, and administers dantrolene at 2.5 mg/kg intravenously; the dose of dantrolene can be repeated every 5 minutes as needed for effect, up to a total dose of 10 mg/kg. Efficacy of treatment is monitored via arterial blood gas analysis, measurement of serum levels of creatinine kinase, and frequent determination of vital signs. Treatment of hyperthermia includes use of cooling blankets, ice packs, and iced intravenous solutions (19); treatment should be tempered as needed to avoid hypothermia.
Continuous cardiac monitoring is necessary to assess for cardiac dysrhythmias due to hyperkalemia. Management of hyperkalemia requires administration of insulin and glucose. One hundred percent oxygen is administered; for intubated patients, an increased ventilatory rate is needed to eliminate any excessive production of carbon dioxide. Patients with malignant hyperthermia are at risk for rhabdomyolysis, so aggressive fluid resuscitation including administration of diuretics (mannitol) is needed to prevent renal failure.
Emergence Delirium
A few patients awaken from anesthesia with emergence delirium. (5(p418)) This condition is more common in the young and the elderly than in other age groups and in patients who were particularly anxious preoperatively. Often this delirium is associated with use of anesthetic medications such as ketamine, (20) anticholinergics, barbiturates, and benzodiazepines. However, critical care nurses must further assess patients with emergence delirium by using arterial blood gas analysis and measuring serum electrolyte levels to determine the source, such as physiological causes, which include hypoxemia, hypothermia, hypoglycemia, and hypoventilation. (13)
Treatment consists of administering additional doses of reversal agents or sedatives and allowing time to pass and medication levels to decrease. Patients may need to be protected from self-harm during this period, and critical care nurses may need to use soft restraints, reorient the patient frequently, and ensure airway patency.
Nausea and Vomiting
Postoperative nausea and vomiting occur in an estimated 10% to 50% of patients and are considered some of the most undesirable effects of anesthesia. (21) This complication typically occurs during the first 2 hours after surgery. The effects of postoperative nausea and vomiting range from minor discomfort to aspiration and death and can result in delays in discharge from the PACU. (22) The causes are multifactorial, including, but not limited to, anesthetic- and nonanesthetic-related factors, postoperative administration of opioids, emergency surgery performed when the patient's stomach is full, and abdominal and head and neck surgeries (21,22) (Table 4). Table 5 is a list of commonly administered antiemetics.
Perioperative Alterations in Laboratory Values
Both hypoglycemia and hyperglycemia can occur immediately after surgery. Patients who have elective surgery are usually asked to fast after midnight for surgery the next day. For most patients, fasting is not a problem in terms of blood glucose. For patients with diabetes mellitus, fasting can be more complicated. Even though most patients with diabetes do not take their insulin or hypoglycemic agents the morning of surgery, many of these medications can be long acting and have effects the day after they are taken. Therefore, any patient with diabetes should have a blood glucose level determined during the postanesthetic recovery period. Patients with diabetes who have sepsis may have marked hyperglycemia.
Another group of patients at risk for glucose control problems are patients undergoing surgery while being treated with intravenous hyperalimentation. Maintaining hyperalimentation during surgery can be associated with hyperglycemia, and stopping or reducing hyperalimentation can cause hypoglycemia. Finally, patients with liver disease may not have adequate glucose reserves and are at risk for early postoperative hypoglycemia.
For patients who lose large volumes of blood (>1000 mL), hemoglobin level and hematocrit may be measured when the patients arrive in the critical care unit. Obtaining the measurements depends on whether blood products were administered during the operation, the type of surgery performed, anticipated fluid shifts that may occur early in the postoperative period, and the potential for future blood loss. The results should be compared with baseline values and reported promptly to the physician managing the patient's care.
Conclusions
Nursing care of patients recovering from anesthesia presents many challenges. Patients often are extremely critically ill and are brought directly to the critical care unit, bypassing the PACU, because their physiological status is unstable, they must remain intubated, or they require sedation for a prolonged period. Critical care nurses must understand and respond to the postanesthetic needs of these patients in a prompt manner.
Online
Continuing Education
To receive CE credit for this article, visit the American Association of Critical-Care Nurses' (AACN) Web site at http://www.aacn.org.click on "Education" and select "Continuing Education," or call AACN's Fax On Demand at (800) 222-6329 and request item No. 1174.
References
1. Vasanawala M, Macario A, Canales M. Some common problems in the postanesthetic care unit. Contemp Surg. 2000;56:691-700.
2. Rose D. Recovery room problems or problems in the PACU? Can J Anaesth. 1996;43:R116-R122.
3. Arsenault C. Nurse's guide to general anesthesia, I. Nursing98. March 1998;28(suppl): 32cc1-36cc6.
4. Litwack K. Post Anesthesia Care Nursing. St Louis, Mo: Mosby; 1995:127-184.
5. Stoelting RK, Miller RD. Basics of Anesthesia. 4th ed. Philadelphia, Pa: Churchill Livingstone; 2000.
6. Arsenault C. Nurse's guide to general anesthesia, II. Nursing98. May 1998;28(suppl): 32cc1-32cc5.
7. Berg M. An introduction to anesthesia-related medications. J Perianesth Nurs. 1998; 13:239-242.
8. Christopherson TJ. Succinylcholine side effects. In: Faust RJ, ed. Anesthesiology Review. New York, NY: Churchill Livingstone; 2002:134-136.
9. Faust RJ. Prolongation of succinylcholine effect. In: Faust RJ, ed. Anesthesiology Review. New York, NY: Churchill Livingstone; 2002:137-138.
10. Keegan MT. Nondepolarizing muscle relaxants. In: Faust RJ, ed. Anesthesiology Review. New York, NY: Churchill Livingstone; 2002: 139-141.
11. Kervin MW. Residual neuromuscular blockade in the immediate postoperative period. J Perianesth Nurs. 2002;17:152-158.
12. Wilson M. Giving postanesthesia care in the critical care unit. Dimens Crit Care Nurs, 2000; 19:38-43.
13. Marley R. Postoperative oxygen therapy. J Perianesth Nurs. 1998;13:394-412.
14. Murray-Calderon P, Connolly M. Laryngospasm and noncardiogenic pulmonary edema. J Perianesth Nurs. 1997;12:89-94.
15. Bryant C, Ray C, Haas RE. Hypotension in the PACU: an algorithmic approach. J Perianesth Nurs. 2002;17:159-163.
16. Drain CB. The Post Anesthesia Care Unit. 3rd ed. Philadelphia, Pa: WB Saunders Co; 1994:563-569.
17. Jerran L. Clinical guideline for the prevention of unplanned perioperative hypothermia. J Perianesth Nurs. 2001;16:305-314.
18. Wedel DJ. Malignant hyperthermia. In: Faust RJ, ed. Anesthesiology Review. New York, NY: Churchill Livingstone; 2002:488-489.
19. Redmond M. Malignant hyperthermia: perianethesia recognition, treatment, and care. J Perianesth Nurs. 2001;16:259-270.
20. Lockwood SA. Ketamine. In: Faust RJ, ed. Anesthesiology Review. New York, NY: Churchill Livingstone; 2002:124-125.
21. Koivuranta M, Laara E, Snare L, Alahuhta S. A survey of postoperative nausea and vomiting. Anaesthesia. 1997;52:443-449.
22. Nelson TP. Postoperative nausea and vomiting: understanding the enigma. J Perianesth Nurs. 2002;17:178-189.
Claudia P. Barone, RN, EdD, LNC, CPC
Carmelita S. Pablo, MD
Gary W. Barone, MD
Authors
Claudia P. Barone is a clinical associate professor in the college of nursing at the University of Arkansas for Medical Sciences in Little Rock, Ark. She also maintains a clinical practice in the outpatient postanesthesia care unit at University Hospital in Little Rock.
Carmelita S. Pablo is a professor and the chairperson of the anesthesia department at the University of Arkansas for Medical Sciences.
Gary W. Barone is an associate professor in the department of surgery, division of transplant surgery at the University of Arkansas for Medical Sciences.
To purchase reprints, contact The InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 809-2273 or (949) 362-2050 (ext 532); fax, (949) 362-2049; e-mail, reprints@aacn.org.
COPYRIGHT 2004 American Association of Critical-Care Nurses
COPYRIGHT 2004 Gale Group