Esophageal abnormalities are common in patients with noncardiac chest pain, but the cause and effect link to chest pain remains unclear. Frobert and associates evaluated esophageal dysfunction as a possible source of pain in patients with angina-like chest pain but normal coronary angiograms.
Patients with chronic angina-like pain and normal coronary angiograms were evaluated for myocardial metabolism and left ventricular abnormalities. They were selected for assessment of esophageal function according to the following criteria: (1) chronic chest pain and normal coronary angiograms; (2) left ventricular ejection fraction greater than 50 percent; (3) no evidence of valvular or myocardial disease or dysfunction, and (4) no coronary artery vasospasm during hyperventilation testing. Myocardial and peripheral lactate levels were also measured.
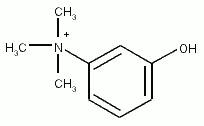
Sixty-three patients participated, along with a control group of 22 healthy persons. All of the subjects completed a questionnaire describing chest and esophageal symptoms. Esophageal manometry and two esophageal provocation tests--one using intravenous edrophonium chloride and one using acid perfusion--were performed. Forty-six of the 63 patients had a total of 248 episodes of chest pain during the esophageal studies.
Reflux indexes and esophageal motor function did not differ between study subjects and control subjects. Chest pain was elicited by esophageal provocation tests in study subjects but not in control subjects. The exact mechanism of pain occurring during acid perfusion testing is unknown. It has been hypothesized that patients with a positive provocation test may have heightened sensitivity to esophageal stimuli, although the clinical significance of this mechanism is not clear.
The authors conclude that no relationship is apparent between chest pain and abnormal esophageal function. Medical therapy directed against pain presumed to have an esophageal etiology has been disappointing. Routine esophageal evaluation does not appear to be necessary in these patients, although the positive results of provocation tests indicate that some yet-unknown form of esophageal involvement, perhaps through abnormal visceral pain perception, may play a role in pain generation.
In a related editorial, Goyal notes that chest pain may be caused by esophageal dysfunction, including food impaction, diffuse esophageal spasm and achalasia. These diagnoses, however, are generally suspected because of associated symptoms of dysphagia and regurgitation. Without these additional symptoms, esophageal studies in patients with noncardiac chest pain are not likely to be helpful. Current theories are focusing on mechanisms of hyperalgesia of the esophagus, heart or other visceral organs. (Frobert O, et al. Diagnostic value of esophageal studies in patients with angina-like chest pain and normal coronary angiograrns. Ann Intern Med 1996;124:959-69, and Goyal RK. Changing focus on unexplained esophageal chest pain [Editorial]. Ann Intern Med 1996; 124:1008-10.)
COPYRIGHT 1996 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group