Less than 15 percent of the U.S. population is older than 65 years, yet this age group accounts for nearly one third of prescription drug use. Older patients also tend to have multiple chronic diseases, requiring them to take several drugs simultaneously. The risk of adverse events related to medication use increases among older patients because of age-related changes in metabolism and excretion of drugs. In 1991, criteria were published to determine the appropriateness of medications used by nursing home residents. These criteria were revised recently to include 28 medications or classes of medications considered inappropriate for use in older patients. Curtis and associates used these criteria to determine the extent of inappropriate outpatient prescribing for older patients.
The study design was a retrospective cohort analysis of outpatient prescription claims collected from the database of a large national pharmaceutical management company, which involved participants from all 50 states. Patients were included if they were 65 years or older at the start of the data collection period and had filed at least one prescription claim within the one-year study period. The authors limited their analysis to the 18 medications that the consensus panel recommended avoiding in older patients at any dosage or frequency. The main outcome measure was the number of patients taking one or more of the 18 medications. The secondary outcome measure was the number of patients taking two or more of the medications.
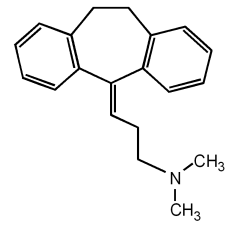
The data reviewed were from 1999 and identified 765,423 patients who met the inclusion criteria. Twenty-one percent (n = 162,370) filled a prescription for one or more of the medications. The most common prescription drugs that should be avoided in this age group include amitriptyline (Elavil) and doxepin (Sinequan; see the accompanying table). Of the patients who filled multiple prescriptions from this medication group, 16 percent received two prescriptions, and 4 percent received three or more. Psychotropic and neuromuscular drugs were the most commonly prescribed medication classes.
The authors concluded that, in 1999, more than one out of five older patients filled prescriptions for medications that should be avoided in this age group. Clinical and laboratory studies need to be performed to improve the quality of patient-specific alerts.
Curtis LH, et al. Inappropriate prescribing for elderly Americans in a large outpatient population. Arch Intern Med August 9/23, 2004;164:1621-5.
EDITOR'S NOTE: The issue of inappropriate prescription drug use by older patients has been identified for years in various publications, including two studies that were published 10 years ago. In a recent editorial, Steel (1) writes that although these and other studies concerning this issue have been published, "little or nothing" has been done to solve this problem. Various solutions include the development of computerized systems that could identify inappropriate prescriptions written for older patients. According to Steel, (1) if the outcome were this negative in any other setting, there would be a significant public reaction. The bottom line is that physicians and other health care professionals who see older patients and write prescriptions need to be aware of inappropriate medications and should avoid prescribing them to older patients.--K.E.M.
REFERENCE
(1.) Steel K. The time to act is now. Arch Intern Med 2004;164:1603-4.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group