Cardiovascular disease affects one in four Americans. According to the American Heart Association, heart and related diseases are expected to cost Americans more than $329 billion in 2002. An estimated 10 million persons in this country are known to have diabetes and 3.6 million to have renal disease, incurring annual health care costs of $98 billion and $11 billion, respectively. Although angiotensin-converting enzyme (ACE) inhibitors have documented clinical benefits in a variety of clinical situations, the disparity between the evidence from clinical trials and bedside medicine is well documented.
The National Registry of Myocardial Infarction 2 found that fewer than one half of patients surviving acute myocardial infarction who were candidates for therapy with ACE inhibitors received these life-saving drugs at discharge. (1) A recent review of patients with asymptomatic left ventricular dysfunction revealed an underuse of ACE inhibition (48 percent of eligible candidates) and a greater likelihood of being started on an ACE inhibitor if under the care of a cardiologist rather than a noncardiologist. (2) In 2000, Bahit and colleagues (3) reviewed actual versus ideal prescribing of drugs for secondary prevention after myocardial infarction and estimated that 30,600 lives would be saved annually by offering ACE inhibitors.
Renin-Angiotensin System
The renin-angiotensin system is systemically and locally driven. The systemic process is triggered by the kidney's response to decreased effective blood volume and begins with the secretion of renin from the renal cortex. Once released, renin cleaves angiotensinogen to form angiotensin I. This product, in turn, is catalyzed by angiotensin-converting enzyme, formed primarily in the pulmonary vasculature, into angiotensin II. This potent vasoconstrictor affects tissues and systems throughout the body; research shows that these vasoconstrictor effects are attenuated by ACE inhibition (Table 1). (4,5)
Local renin-angiotensin systems exist in all vascular endothelium. Vascular cells maintain local vasomotor tone homeostasis primarily through the elaboration of angiotensin II and nitric oxide, a potent vasodilator. If this mechanism becomes impaired by oxidative stress, the endothelium can no longer maintain vasomotor tone in response to local needs. This phenomenon, termed endothelial dysfunction, precedes and contributes to atherosclerosis. (6) ACE inhibition attenuates endothelial dysfunction by decreasing the destruction of bradykinin, thereby enhancing production of nitric oxide. (5,7)
Clinical investigations support the benefits of ACE inhibition. The results of the Trial on Reversing ENdothelial Dysfunction (TREND) showed improved coronary blood flow with the administration of quinapril. (8) The Heart Outcomes Prevention Evaluation (HOPE) and the Microalbuminuria Cardiovascular and Renal Outcomes-HOPE (MICRO-HOPE) trials have provided evidence of reduced mortality rates, myocardial infarction, stroke, and overt nephropathy with the use of ramipril. (9,10)
Ace Inhibitors: Formulations
Ten ACE inhibitors presently approved for use in the United States work by competitive inhibition of angiotensin-converting enzymes. Captopril (Capoten) and enalapril (Vasotec) are off-patent, which makes them more economical. Enalapril is the only one available in intravenous form, which is called enalaprilat (Vasotec-IV). Drug formularies may dictate which ACE inhibitor a physician is able to prescribe because they are thought to be interchangeable. If a choice is possible, physicians should use those agents that have been proved by clinical trials to reduce morbidity and mortality for the condition being treated and work toward target dosages or clinical end points (Table 2). (11)
Initiating Treatment: Considerations
RENAL INSUFFICIENCY
In patients with renal insufficiency, no creatinine level is an absolute contraindication to ACE inhibitor therapy. ACE inhibitors are not nephrotoxic. Baseline serum creatinine levels of up to 3.0 mg per dL (27 [micro]mol per L) are generally considered safe. The manufacturers make recommendations for initiating treatment and suggest titrating the dosage slowly. An increase of 20 percent in the serum creatinine level is not uncommon and is not a cause for discontinuing the medication. For any higher increase, the family physician should consider a nephrologist. During the first four weeks of treatment, serum potassium and creatinine levels should be monitored closely.
HYPOTENSION
Hypotension can occur in patients with volume depletion or hyponatremia (sodium <130 mEq per L [<130 mmol per L]), those taking vasodilators, those in acute congestive heart failure, and those on dialysis. The underlying problem should be corrected, starting with a low dosage and titrating slowly. Any patient with a high plasma renin level is vulnerable to first-dose hypotension, but this effect is transient and unpredictable. (12) Hypotension is not a reason to discontinue ACE inhibition. Patients should be rechallenged at one half the previous dosage. If they are taking a diuretic, the dosage should be reduced or held for three days before reattempting therapy.
COUGH
Cough occurs in 5 to 20 percent of patients. It is not dose- or brand-related, is more frequent in women than men, and is more frequent in blacks than whites. It develops within one week to six months and resolves within four days of cessation. Physicians should be aware of a confounding congestive heart failure cough and remember that changing to another formulation sometimes helps. Cough is not a reason to discontinue treatment unless the patient cannot tolerate it. A few studies have looked at the use of nonsteroidal anti-inflammatory drugs (NSAIDs), nifedipine (Procardia), cromolyn (Intal), or nebulized bupivacaine (Marcaine) for managing cough, but further studies are needed. (13)
HYPERKALEMIA
Hyperkalemia does not usually occur in renocompetent patients, but those who have renal insufficiency or diabetes. Patients who are taking potassium, salt substitutes, potassium-sparing diuretics, beta blockers, and NSAIDs are susceptible. Most clinicians discontinue potassium and potassium-sparing diuretics when starting patients on ACE inhibitor therapy. Potassium levels should be monitored carefully in patients at risk. Up to 5 percent of patients experience serum potassium levels greater than 5.7 mEq per L (5.7 mmol per L), and if levels remain higher than that on repeat testing, ACE inhibitor therapy should be discontinued.
TERATOGENICITY
Women of childbearing age should be warned to notify their physicians immediately if they become pregnant during ACE inhibitor therapy. ACE inhibitors are not considered teratogenic if they are discontinued during the first trimester (class C), but they are considered teratogenic in the second and third trimesters (class D).
Other Considerations
Neutropenia occurs rarely and tends to occur in patients with renal impairment and concurrent collagen vascular disease. Lithium toxicity is also rare, but lithium levels should be monitored if the patient is on concurrent lithium therapy. Aortic stenosis and hypertropic cardiomyopathies are considered relative contraindications because of the risk of hypotension from fixed outlet obstruction.
Absolute Contraindications
Angioneurotic edema, which occurs in 0.1 to 0.2 percent of patients, usually develops within the first week of therapy but can occur at any time. This life-threatening adverse effect also occurs with angiotensin II receptor blockers but to a lesser extent. (14) Any patient with a history of angioneurotic edema, whether related to an ACE inhibitor, angiotensin receptor blockers, or another cause, should not be given an ACE inhibitor. Other contraindications include pregnancy, renal artery stenosis, and previous allergy to ACE inhibitors.
Indications
Several chronic diseases have been shown to stabilize or improve with the use of ACE inhibitors (Table 3 (15,16)). (17) Family physicians should be familiar with these agents as appropriate primary, secondary, and tertiary prevention for these prevalent and disabling chronic diseases.
HYPERTENSION
Guidelines for the pharmacologic management of hypertension issued by the World Health Organization and the International Society of Hypertension place ACE inhibitors with diuretics and beta blockers as first-line therapy. The Sixth Report of the Joint National Committee (1997) removed ACE inhibitors as first-line therapy because they had not been shown in clinical trials to reduce all-cause mortality as had diuretics and beta blockers. (18)
In 1999, the Captopril Prevention Project (19) randomized trial compared the three agents. Captopril and conventional treatment did not differ in cardiovascular end points overall; all events except for stroke were lower in the captopril group. Improper randomization has been cited as a possible reason for increased stroke rates. (20) The results of the Swedish Trial in Old Patients with Hypertension-2 study (21) showed equal outcomes between the three drug classes.
ACE inhibitors have a side effect profile that may place them above thiazides and beta blockers. They do not affect lipid, calcium, or uric acid levels, and are less likely to cause erectile dysfunction than other antihypertensive agents. (14) There is evidence from several trials that fasting glucose levels, glycosylated hemoglobin levels, and rates of new diagnoses of type 2 diabetes are lower in patients randomized to ACE inhibitor therapy than in those taking placebo. The Diabetes Reduction Assessment with Ramipril and Rosiglitazone Medication (DREAM) trial will evaluate prospectively whether this ACE inhibitor prevents diabetes. (22) Treatment goals for blood pressure include 140/90 mm Hg (or less) in patients without comorbidities, 130/80 mm Hg (or less) in patients with diabetes (2001 American Diabetes Association [ADA] Guidelines) and 125/75 mm Hg (or less) in those with end organ damage.
CONGESTIVE HEART FAILURE
ACE inhibitors are first-line therapy in patients with left ventricular systolic dysfunction, as confirmed in multiple trials and meta-analyses. Decreases in dyspnea, emergency department visits, hospitalizations, disease progression, death, and the need for diuretics have been proved, as well as increases in ejection fraction and exercise tolerance. (23) All patients with systolic dysfunction, even if they are asymptomatic, should be considered for treatment with an ACE inhibitor. This consideration mandates wide use of cardiac imaging to identify the presence and type of heart failure.
Target dosages used in the clinical trials that showed reduced morbidity and mortality are listed in Table 2. (11) Starting doses should be determined individually and based on clinical status (i.e., blood pressure, serum sodium level) and comorbidities (i.e., age, renal insufficiency). When the dosage is titrated up, the diuretic dosage will probably need to be decreased.
Diuretics, while essential for controlling volume overload, do not confer mortality reduction like the first-line therapies of ACE inhibition and beta blockade. The one exception to this is spironolactone (Aldactone), which has shown mortality reduction in Class III and IV heart failure. (24)
MYOCARDIAL INFARCTION
In 1996 and 1999, the American Heart Association advocated the administration of an ACE inhibitor to all patients presenting with acute anterior myocardial infarction and/or clinical heart failure in the absence of hypotension or other contraindications. The guidelines recommend starting within the first 24 hours and continuing therapy indefinitely for anterior infarctions and left ventricular dysfunction. (25)
A pragmatic approach is to give ACE inhibitors to all patients with acute myocardial infarction who are clinically stable and to continue that therapy indefinitely in those with anterior myocardial infarction or systolic dysfunction. Others should be re-evaluated for continuation of therapy at four to six weeks. (15)
DIABETES MELLITUS
ACE inhibitors slow the onset of diabetic nephropathy in patients with microalbuminuria and type 1 diabetes. (26) Normotensive, nonalbuminuric diabetics also have a slower onset of nephropathy; however, the ADA currently does not recommend ACE inhibitors as primary prevention in these patients, and there is no evidence that this practice affects outcomes. (27,28)
In the MICRO-HOPE trial, patients with diabetes and one cardiac risk factor were studied; subjects were titrated to 10 mg a day of ramipril or placebo. The study was stopped prematurely because of the significant decrease in combined primary outcomes in patients taking ramipril. Total cardiovascular end points were reduced by 25 percent (95 percent confidence interval, 12 to 36; P = 0.0004); these included myocardial infarction (22 percent), cerebrovascular accident (33 percent), cerebrovascular death (37 percent), total mortality (24 percent), revascularization (17 percent) and overt nephropathy (24 percent). (10) Ramipril was approved by the U.S. Food and Drug Administration in November 2000 for primary prevention of cardiovascular events in at-risk patients.
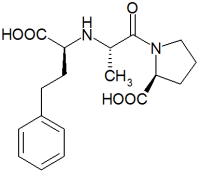
A meta-analysis of four trials including 1,123 patients with type 2 diabetes showed improved outcomes in those taking ACE inhibitors as opposed to other antihypertensive agents. (29) The authors noted in their conclusions that atenolol (Tenormin) may be equivalent to captopril and that further studies are needed in regard to these two agents. Figure 1 represents the risk reduction as calculated in this meta-analysis. (29) It will be rare for a patient with diabetes not to meet the criteria for ACE inhibition in the year 2002.
RENAL INSUFFICIENCY
ACE inhibitors in nondiabetic patients with nephropathy are more effective than other antihypertensives at slowing progression to end-stage renal disease. (30) The Ramipril Efficacy in Nephropathy (REIN) study (30) (treatment goal: diastolic blood pressure less than 90 mm Hg) and the Angiotensin-Converting Enzyme Inhibition in Progressive Renal Insufficiency (AIPRI) study (30) (treatment: benazepril, in a dosage of 10 mg daily) demonstrated improved renal survival. Even in normotensive patients with nondiabetic proteinuria, the EUCLID study group demonstrated slowing of progression of renal disease. (27) Unless contraindicated, ACE inhibitors should be used in patients with renal insufficiency of any cause with a goal blood pressure of 125/75 mm Hg in those with more than 1,000 mg per 24 hours (1 g per 24 hours) proteinuria. (30)
Angiotensin Receptor Blockers
Angiotensin receptor blockers (ARBs) are a promising adjunct to ACE inhibitors because angiotensin II is synthesized through other pathways. A recent meta-analysis of ARBs in heart failure concluded that ACE inhibitors are superior to ARBs in reducing hospitalization and all-cause mortality. The combination of both agents was superior to ACE inhibitors alone for reducing hospitalizations but not mortality. (31) As single agents, ARBs have not been shown to be superior to ACE inhibitors and are an expensive alternative when the former are not tolerated.
The author indicates that she does not have any conflicts of interest. Sources of funding: none reported.
REFERENCES
(1.) Barron HV, Michaels AD, Maynard C, Every NR. Use of angiotensin-converting enzyme inhibitors at discharge in patients with acute myocardial infarction in the United States: data from the National Registry of Myocardial Infarction 2. J Am Coll Cardiol 1998;32:360-7.
(2.) Kermani M, Dua A, Gradman AH. Underutilization and clinical benefits of angiotensin-converting enzyme inhibitors in patients with asymptomatic left ventricular dysfunction. Am J Cardiol 2000;86:644-8.
(3.) Bahit MC, Granger CB, Alexander KP, Kramer J, Lapointe NM, Califf RM. Applying the evidence: opportunity in US for 80,000 additional lives saved per year. Retrieved online August 2001.
(4.) Jackson EK, Garrison JC. Renin and angiotensin. In: Goodman LS, Gilman A, Hardman JG, Limbird LE, eds. Goodman & Gilman's The pharmacological basis of therapeutics. 9th ed. New York: McGraw-Hill, Health Professions Division, 1996:733-58.
(5.) Lonn EM, Yusuf S, Jha P, Montague TJ, Teo KK, Benedict CR, et al. Emerging role of angiotensin-converting enzyme inhibitors in cardiac and vascular protection. Circulation 1994;90:2056-69.
(6.) Anderson TJ. Assessment and treatment of endothelial dysfunction in humans. J Am Coll Cardiol 1999;34:631-8.
(7.) Parmley WW. Evolution of angiotensin-converting enzyme inhibition in hypertension, heart failure, and vascular protection. Am J Med 1998;105:S27-31.
(8.) Mancini GB, Henry GC, Macaya C, O'Neill BJ, Pucillo AL, Carere RG, et al. Angiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease. The TREND (Trial on Reversing ENdothelial Dysfunction) Study. Circulation 1996;94:258-65.
(9.) Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med 2000;342:145-53.
(10.) The Heart Outcomes Prevention Evaluation Study Investigators. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet 2000;355:253-9.
(11.) Physicians' desk reference, 2001. 55th ed. Montvale, N.J.: Medical Economics, 2001.
(12.) Katzung BG. Basic & clinical pharmacology. 8th ed. Stamford, Conn.: Appleton & Lange, 2001:172-4.
(13.) Drug facts and comparisons. St. Louis: Facts and Comparisons, 2001:504-9.
(14.) Gifford RW Jr. Antihypertensive therapy. Angiotensin-converting enzyme inhibitors, angiotensin II receptor antagonists, and calcium antagonists. Med Clin North Am 1997;81:1319-33.
(15.) Gersh BJ. Optimal management of acute myocardial infarction at the dawn of the next millennium. Am Heart J 1999;138(2 pt 2): S188-202.
(16.) Pitt B, Poole-Wilson PA, Segal R, Martinez FA, Dickstein K, Camm AJ, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomised trial--the Losartan Heart Failure Survival Study ELITE II. Lancet 2000;355: 1582-7.
(17.) Barton S, ed. Clinical evidence. London, U.K.: BMJ Publishing Group, 2001(5):xiv.
(18.) The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. McLean, Va.: International Medical Publishing, 1997; NIH publication no. 98-4080.
(19.) Hansson L, Lindholm LH, Niskanen L, Lanke J, Hedner T, Niklason A, et al. Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomised trial. Lancet 1999;353:611-6.
(20.) Fournier A, Pruna A, Esper NE, Makdassi R, Oprisiu R, Westeel PF, et al. Captopril prevention project--what shall we do about captopril and the risk of stroke? Nephrol Dial Transplant 2000;15:2-5.
(21.) Hansson L, Lindholm LH, Ekbom T, Dahlof B, Lanke J, Schersten B, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet 1999;354:1751-6.
(22.) Yusef S, Gerstein H, Hoogwerf B, Pogue J, Bosch J, Wolffenbuttel BH, et al. Ramipril and the development of diabetes. JAMA 2001; 286:1882-5.
(23.) American College of Cardiology. Consensus recommendations for the management of chronic heart failure. On behalf of the membership of the advisory council to improve outcomes nationwide in heart failure. Am J Cardiol 1999;83:1A-38A.
(24.) Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 1999;341:709-17.
(25.) Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, et al. 1999 update: ACC/AHA guidelines for the management of patient with acute myocardial infarction: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation 1999;100:1016-30.
(26.) American Diabetes Association Clinical Practice Recommendations 2001. Diabetes Care 2001;24(suppl 1):S1-133.
(27.) Randomised placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria. The EUCLID study group. Lancet 1997;349: 1787-92.
(28.) Ravid M, Brosh D, Levi Z, Bar-Dayan Y, Ravid D, Rachmani R. Use of enalapril to attenuate decline in renal function in normotensive, normoalbuminuric patients with type 2 diabetes mellitus. A randomized, controlled trial. Ann Intern Med 1998;128(12 pt 1):982-8.
(29.) Pahor M, Psaty BM, Alderman MH, Applegate WB, Williamson JD, Furberg CD. Therapeutic benefits of ACE inhibitors and other antihypertensive drugs in patients with type 2 diabetes. Diabetes Care 2000:23:888-92.
(30.) Bakris GL. Improving prognosis of nondiabetic chronic renal insufficiency: the role of ACE inhibitors. Kidney Int (In press).
(31.) Jong P, Demers C, McKelvie RS, Liu PP. Angiotensin receptor blockers in heart failure: meta-analysis of randomized controlled trials. J Am Coll Cardiol 2002;39:463-70.
Richard W. Sloan, m.d., r.ph., coordinator of this series, is chairman of the Department of Family Medicine at York (Pa.) Hospital and clinical associate professor in family and community medicine at the Milton S. Hershey Medical Center, Pennsylvania State University, Hershey, Pa.
DAPHNE P. BICKET, M.D., M.L.S., is geriatric coordinator of the family practice residency program at University of Pittsburgh Medical Center-McKeesport, McKeesport, Pa. She is also a clinical instructor in family medicine in the Department of Family Medicine at the University of Pittsburgh School of Medicine. Dr. Bicket received her medical degree from Wake Forest University School of Medicine, Bowman Gray Campus, Winston-Salem, N.C., where she also completed a residency in family practice. She has a master's degree in library science.
Address correspondence to Daphne P. Bicket, M.D., M.L.S., Family Practice Residency Program, UPMC McKeesport, 2347 Fifth Ave., McKeesport, PA 15132 (e-mail: bicketdp@msx.upmc.edu). Reprints are not available from the author.
COPYRIGHT 2002 American Academy of Family Physicians
COPYRIGHT 2002 Gale Group