Toward a more cautious approach, as per OBRA
All drugs prescribed for the nursing home patient may be considered to be psychoactive, in that they may affect the central nervous system (CNS) (Table 1). Nurses may ascribe most of these CNS effects to underlying disease processes rather than to these medications. That is why one of the most important assessments to be made by the charge nurse, with the consultant pharmacist's input, is whether a drug effect is involved. The question is, "How did this medicine affect the patient within the first several days to weeks after the drug was started?"
For example, the nursing home patient with dementia may reverse his or her sleep cycle and "sundown" (i.e. become more confused at the evening hours) and therefore have difficulty falling asleep at the usual hours. The preferred treatment for this sleep disorder is to involve the patient in physical activities as much as possible during the daytime, and to prevent napping, especially after meals. If a hypnotic medication is prescribed nightly, especially one of the longer-acting benzodiazepines (LABZs) - whether FDA-approved or not for sleep (e.g. only fluazepam, estazolam, temazepam, triazolam and quazepam are so-approved), the patient will usually experience normal sleep for several evenings, then after days to weeks start experiencing daytime carryover sedation and increased confusion. If continued, the LABZs also increase the risk of falls and fractures, especially in the Alzheimer's disease patient.
The OBRA guidelines for hypnotic usage in long-term care patients specify that LABZs not be used unless shorter-acting benzodiazepines (SABZs) have been tried. The OBRA guidelines further state that sleeping medications should not be used for more than 10 consecutive days in any 30-day period, nor should any benzodiazepine be used for longer than 3 to 4 months for anxiety disorders (Table 2). Even the SABZs given more often than three times a week increase the risk of falls in the frail elderly patient. If the caregiver notes any increased confusion, daytime sedation, or falls, the prescriber should be contacted.
SABZs should also be used for the agitation and harmful behavior associated with psychoses. The recommended drugs and doses for SABZ use in the Alzheimer's disease patient are shown in Table 2.
It is important for patient caregivers and prescribers to realize that the need for psychotropic medication diminishes as the patient advances through the stages of dementia. The continued usage of potent antipsychotics and LABZs in particular may in fact increase the overall rate of complications in the patient. The recommended dosage of any drug for the agitated demented patient is considerably less than the OBRA requirements, as may be noted in Table 3.
It should be noted that the OBRA regulations consider the usage of all barbiturates (except phenobarbital as an anticonvulsant) and non-barbiturate sedative hypnotics as "unnecessary drugs," and attempts should be made to gradually taper these drugs by no more than 10 to 15 percent of the daily dose per week. The same tapering recommendation should be made for the LABZs when used for more than one to two weeks on a daily basis, to prevent severe withdrawal symptoms of nervousness and cramps, as well as other vague pain complaints, insomnia, hallucinations, and agitation.
The appropriate usage of medications for anxiety and sleep disorders in the nursing home patient is the shared responsibility of the administrator, nurses, attending physicians and consultant and provider pharmacists. A routine assessment of the compliance with the OBRA guidelines for appropriate agents (e.g. SABZs before LABZs), dosage, and duration of therapy, as well as efficacy and toxicity, should be a part of the ongoing Quality Assurance and Assessment Committee's commitment to utilization review for each patient of every facility.
James W. Cooper, Pharm. PhD, is Professor and Head, Department of Pharmacy Practice, The University of Georgia College of Pharmacy, Athens, GA.
TABLE 1 - Psychoactive Drugs Commonly Used in Nursing Home Patients
Antipsychotics
Mellaril, Serentil, Thorazine, Navane, Haldol, Stelazine, Prolixin, Taractan, Moban, Loxitane, Trilafon(*)
Antidepressants
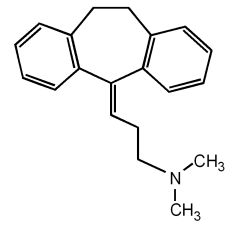
Elavil/Endep(*), Aventyl/Pamelor, Vivactyl, Tofranil/SKPramine, Norpramin/Pertofrane, Sinequan/Adapin, Ascendin, Ludiomil, Prozac, Zoloft, Paxil, Wellbutrin, Surmontil, lithium, Clozaril, Anafranil. AVOID MAOI TYPE AGENTS ALTOGETHER
Antiparkinsonism Agents
L-DOPA, Sinemet, Symmetrel, Cogentin, Artane, Kemadrin, Benadryl, Akineton, Parlodel, Permax, Eldepryl
Antianxiety and Hypnotic Agents
Librium, Valium, Dalmane, Miltown/Equanil, Tranxene, Paxipam, Centrax, Klonopin, Ativan, ProSom, Doral, Serax, Xanax, Halcion, chloral hydrate, Doriden, Noludar, Placidyl, Seconal, Nembutal, Amytal, Tuinal, Butisol, phenobarbital
Antihistamines (Combination, cold/hay fever products with decongestants)
Chlor-trimeton (Ornade, Isochlor) Dimetane (Dimetapp), Benadryl, Tavist, Ambodryl, Clistin, Decapryn, Polaramine, Forhistal, Actidil (Actifed), PBZ, Histadyl, Tacaryl, Phenergan, Temaril, Atarax/Vistaril, Optimine, Periactin, Seldane, Hismanal, Claritin
Antinauseants
Phenergan, Tigan, Compazine, Torecan, Reglan, Propulsid, Trans-Scop, Antivert/Bonine, Marezine
Antidiarrheals
Lomotil, Immodium, Donnagel, Parapectolin
Antisecretory
Robinul, Donnatal, Levsin, atropine, scopolamine, Pamine, Quarzan, Tral, Darbid, Cantil, Bathine, Pro-Banthine, Pathilon, Bentyl, Daricon, Ditropan, various combination products
Antiulcer Drugs
Tagamet, Zantac, Pepcid, Axid, Prilosec, Cytotec
Analgesics
Darvocet/Wygesic, Talwin, Percodan, Percocet, Lortabs, codeine, morphine, all narcotics analgesics (NAs)
Antihypertensives (with central nervous system effects)
Aldomet, Sytensin, Tenex, Catapres, Ismelin, Hylorel, reserpine, Inderal, Corgard, Tenormin, Blocadren, Lopressor, Visken, Normodyne/Trandate, Sectral, Levatol, Cartrol, Isoptin/Calan/Verelan, Kerlone
Antianginals
Isoptin/Calan/Verelan, Cardizem, Procardia/Adalat, Cardene, Plendil, Norvasc, DynaCirc, Vascor
Antiarrhythmics
Quinidine, Pronestyl/Procan, Norpace, Tonocard, Tambocor, Mexitil, Cardarone, Enkaid, DecaBid
Anticonvulsants
Dilantin, phenobarbital, Tegretol, Depakene/Depakote, Mysoline, Zarontin, Klonopin
CNS Stimulants
Theophylline products, caffeine, Trental, Ritalin, Cylert
* indicates that these drugs may also be available in combination products.
SOURCE: Cooper JW. Community and Nursing Home Practice Drug Therapy OBRA Monitoring and Patient Education Guidelines, 1993. Watkinsville, GA, Consultant Press, 1200 Colliers Creek Rd., Watkinsville, GA 30677
TABLE 2. Benzodiazepine OBRA Recommendations
For the Longer-Acting BZS (LABZs) - (Half-Life 20 to 200 Hours)
1. LABZ must not be used unless trial with shorter-acting BZ (SABZ) (Half-life less than 10-20 hours has been tried). (See #4 in this table for shorter-acting).
2. LABZs should not be given daily for more than four (4) consecutive months for anxiety or dementia and 10 continuous days of any months unless gradual dose reduction is unsuccessful and must show improvement in functional status, and,
3. No more than the doses listed in Schedule 1 are used:
4. Shorter-Acting BZ and other anxiolytics
A. Use for other than sleep induction.
B. Daily use at any dose not more than 4 months unless an attempt to taper is unsuccessful (10-25% per week maximum) - twice within the year.
C. Use is for one or more of the following:
1. Generalized anxiety disorder (per DSM IV)
2. Organic mental syndrome (e.g. dementia) with associated agitated states as defined by specific behaviors documented as representing a danger to the patient or others (e.g. caregivers).
3. Panic disorder - agoraphobia, simple phobia, post-traumatic disorder, depression with anxiety symptoms or anxiety not otherwise specified, and daily dose is less than or equal to those listed in Schedule 2:
D. Sleep Induction
1. Other treatable causes of sleep disorder must have been addressed, e.g. depression and pain, (and post-prandial sleep not allowed), and
2. The use of a hypnotic maintains and improves the functional status of a patient (with no falls, etc.), and,
3. Use of a drug to induce sleep is less than 10 consecutive days out of any 30-day period and,
4. Dose is equal or less than those listed in Schedule 3:
SOURCES: Cooper JW, op cit. 22-13, 14; 1990 OBRA Regulations Transmittal
The recommended doses of any drug for the agitated demented patient is considerably less than the OBRA requirements, as may be noted in Table 3 below.
Table 3. Current Pharmacotherapy Recommendations for the Agitated Demented Elderly Patient Note: The patient must have a diagnosis of dementia, psychosis, and hurtful behavior
Non-Sedating Neuroleptics - haloperidol 0.25-0.5 mg BID to TID; fluphenazine 0.25-0.5 mg BID to TID
Sedating Neuroleptic - thioridazine 5-10 mg 3 to 4 times daily.
NOTE: 1 mg haloperidol is approx. equal to 50 mg thioridazine
Beta Blockers - propranolol 5-20 BID-QID; nadolol 20-40 mg/d
Antidepressants - desipramine 25-75 mg per day; trazodone 50 mg 1-4 xd
Anxiolytics - only SABZs - preferably not more than 3 times weekly. Alprazolam 0.125-0.25 mg once to BID or oxazedpam 10 mg once to TID lorazepam 0.5-1mg once to BID. Non-BZ - buspirone 5mg to 10mg once to thrice daily.
Anticonvulsant - carbamazepine 50mg once to QID
Lithium - 75 to 300mg per day.
COPYRIGHT 1993 Medquest Communications, LLC
COPYRIGHT 2004 Gale Group