Smaller, uncontrolled trials of high-dose adjuvant chemotherapy with autologous stem-cell rescue for node-positive breast cancer have produced inconsistent results. Rodenhuis and colleagues report on the results of a large, prospective, controlled, multicenter trial of aggressive "transplant" treatment in women with locally metastatic breast cancer.
The study originally enrolled fewer than 300 patients but was expanded to a total of 885 patients when a preliminary analysis did not reveal a large enough statistical outcome difference between the transplant and the standard treatment groups. The trial enrolled women younger than 56 years who had undergone surgery for breast cancer that revealed at least four axillary lymph nodes with metastases but no distant metastases. Chest radiography, bone scanning, liver sonography, and magnetic resonance imaging were used to exclude persons with widely metastatic disease. Additional exclusion criteria included renal insufficiency (creatinine clearance rate of less than 60 mL per minute [1.0 mL per second]), hepatic insufficiency (serum bilirubin level greater than 1.46 mg per dL [24.96 [micro]mol per L]), or evidence of possible marrow disease (white blood cell count less than 4,000 per [mm.sup.3] [4.0 3 [10.sup.9] per L], platelet count less than 100,000 per [mm.sup.3]).
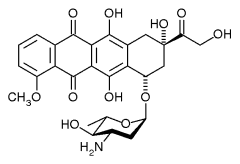
Trial participants were randomized to receive standard chemotherapy with fluorouracil (500 mg per [m.sup.2] of body surface), epirubicin (90 mg per [m.sup.2]), and cyclophosphamide (500 mg per [m.sup.2]) every three weeks for five cycles. Patients assigned to autologous, stem-cell transplant had four cycles of the same treatment, with peripheral blood harvest of stem cells after the third cycle, and a final high-dose cycle of cyclophosphamide (6 g per [m.sup.2]), thiotepa (480 mg per [m.sup.2]), and carboplatin (1,600 mg per [m.sup.2]). Of the 442 patients randomized to the high-dose group, 45 persons did not undergo high-dose treatment because of declined consent, medical complications, or other reasons. All patients with hormone-receptor-positive tumors received tamoxifen for three years after treatment. The median duration of follow-up after treatment was four and three fourths years.
Using an intent-to-treat analysis that included all randomized patients whether or not they completed their assigned therapy, there was no significant overall survival advantage to transplant therapy. The subgroup of women with 10 or more positive nodes did have significantly longer relapse-free survival at the end of follow-up (61 percent) than those receiving standard treatment (51 percent). Women with four to nine positive nodes and those whose tumors were positive for HER2/neu gene amplification (30 percent of cases) did not benefit in terms of long-term survival from transplant.
High-dose therapy could not be completed in six patients because of complications (high fever, cardiac arrhythmia, and possible heart failure), and four patients died because of adverse effects. Secondary cancers developed more frequently during follow-up in patients who received high-dose chemotherapy (21 patients; 4.8 percent) than among those receiving standard treatment (15 patients; 3.4 percent).
The authors conclude that high-dose chemotherapy with stem-cell rescue increases relapse-free survival after five years of follow-up by 10 percent but does not improve overall survival. The improved relapse-free survival is limited to women with 10 or more positive nodes and HER2/neu-negative tumors.
Rodenhuis S, et al. High-dose chemotherapy with hematopoietic stem-cell rescue for high-risk breast cancer. N Engl J Med July 3, 2003;349:7-16.
EDITOR'S NOTE: A similar study (1) of high-dose chemotherapy and stem-cell rescue is reported in the same issue. This trial, by Tallman and associates, involved 417 patients and found no significant difference in relapse-free survival with transplant treatment. The high-dose treatment was lethal in 4.6 percent of cases, and secondary cancers were more common among transplant patients (7.6 percent) than among those receiving standard chemotherapy (3.5 percent).
An accompanying editorial by Elfenbein (2) notes that relapse-free survival may be the better yardstick by which to measure treatment efficacy in these studies. Overall survival, the usual "gold standard," includes many nonrandomized, post-treatment "salvage" measures that affect ultimate survival, and time-to-relapse alone does not take into account patients who died early on because of adverse effects of treatment. Whether the 10 percent advantage in relapse-free survival after five years (demonstrated in only one trial) is worth the 0.9 to 4.6 percent risk of death with transplant and a higher rate of secondary tumors is a tough call for women with high-risk breast cancer.
REFERENCES
(1.) Tallman MS, et al. Conventional adjuvant chemotherapy with or without high-dose chemotherapy and autologous stem-cell transplantation in high-risk breast cancer. N Engl J Med 2003;349:17-26.
(2.) Elfenbein GJ. Stem-cell transplantation for high-risk breast cancer [Editorial]. N Engl J Med 2003; 349:80-2.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group